Abstract
The aim of this study was to assess the efficacy of the Wallis interspinous device for treating lumbar disc herniation (LDH) as well as to investigate whether the device could reduce the incidence of recurrent herniation in comparison with disc excision alone. A total of 72 patients with LDH were treated with primary discectomy and the Wallis interspinous device was implanted in 36. Clinical outcomes were evaluated with a visual analog scale (VAS) for low back and leg pain and the Oswestry Disability Index (ODI) before and after surgery. The incidence of recurrent disc herniation after the operation was also evaluated. There was a significant improvement (p < 0.01) in the clinical outcomes assessed by the VAS and ODI scores compared with preoperative values in both groups. Up to the final follow-up, there were no significant differences between the two groups in VAS and ODI scores (p > 0.05). In addition, there was no significant difference regarding the incidence of recurrent disc herniation between the two groups (13.9% vs. 16.6%, p > 0.05). Of the patients five underwent second discectomy or fusion surgery. The Wallis interspinous device was unable to improve the already good clinical outcome after discectomy for LDH and prevent or reduce recurrence of herniated disc in the current follow-up interval. Whether the device for should be used for LDH should be carefully considered before surgery.
Zusammenfassung
Ziel der vorliegenden Studie war, die Wirksamkeit des interspinösen Wallis-Implantats bei lumbalem Bandscheibenvorfall (LBSV) zu bestimmen und zu prüfen, ob das Device die Inzidenz rezidivierender Bandscheibenvorfälle gegenüber der alleinigen Diskektomie senken kann. Insgesamt 72 Patienten mit LBSV wurden einer primären Diskektomie unterzogen, bei 36 wurde das interspinöse Wallis-Device implantiert. Klinische Ergebnisse wurden mit einer visuellen Analogskala (VAS) für Schmerzen am unteren Rücken und Bein sowie mit dem Oswestry Disability Index (ODI) vor und nach dem operativen Eingriff beurteilt. Die Inzidenz rezidivierender Bandscheibenvorfälle nach Operation wurde ebenfalls bestimmt. Bezüglich der klinischen Ergebnisse, die mit VAS- und ODI-Scores beurteilt wurden, fand sich in beiden Gruppen eine signifikante Verbesserung (p < 0,01) im Vergleich zu den präoperativen Werten. Bis zur letzten Follow-up-Untersuchung waren keine signifikanten Unterschiede zwischen den beiden Gruppen in VAS- und ODI-Scores zu verzeichnen (p > 0,05). Des Weiteren bestand kein signifikanter Unterschied in der Inzidenz rezidivierender Bandscheibenvorfälle zwischen den beiden Gruppen (13,9% vs. 16,6%, p > 0,05). Bei 5 der Patienten wurde eine zweite Diskektomie oder eine Spondylodese durchgeführt. Das interspinöse Wallis-Device konnte bei LBSV das bereits gute klinische Ergebnis nach Diskektomie nicht verbessern und auch nicht die Rezidive des Bandscheibenvorfalls im aktuellen Follow-up-Intervall verhindern oder reduzieren. Vor dem operativen Eingriff gilt es, sorgfältig abzuwägen, ob das Device bei LBSV eingesetzt werden soll.

Similar content being viewed by others
Abbreviations
- CT:
-
Computed tomography
- LDH:
-
Lumbar disc herniation
- MRI:
-
Magnetic resonance imaging
- ODI:
-
Oswestry disability index
- PEEK:
-
Polyetheretherketone
- ROM:
-
Range of motion
- TLIF:
-
Transforaminal lumbar interbody fusion
- VAS:
-
Visual analog scale
References
Jordan J, Konstantinou K, O’Dowd J (2011) Herniated lumbar disc. BMJ Clin Evid 2011:1118
Gugliotta M, da Costa BR, Dabis E, Theiler R, Juni P, Reichenbach S, Landolt H, Hasler P (2016) Surgical versus conservative treatment for lumbar disc herniation: a prospective cohort study. BMJ Open 6:e12938
Osterman H, Sund R, Seitsalo S, Keskimaki I (2003) Risk of multiple reoperations after lumbar discectomy: a population-based study. Spine (Phila Pa 1976) 28:621–627
Lebow RL, Adogwa O, Parker SL, Sharma A, Cheng J, McGirt MJ (2011) Asymptomatic same-site recurrent disc herniation after lumbar discectomy: results of a prospective longitudinal study with 2‑year serial imaging. Spine (Phila Pa 1976) 36:2147–2151
Parker SL, Mendenhall SK, Godil SS, Sivasubramanian P, Cahill K, Ziewacz J, McGirt MJ (2015) Incidence of low back pain after lumbar discectomy for herniated disc and its effect on patient-reported outcomes. Clin Orthop Relat Res 473:1988–1999
Fritzell P, Knutsson B, Sanden B, Stromqvist B, Hagg O (2015) Recurrent versus primary lumbar disc herniation surgery: patient-reported outcomes in the Swedish Spine Register Swespine. Clin Orthop Relat Res 473:1978–1984
Wang SZ, Rui YF, Tan Q, Wang C (2013) Enhancing intervertebral disc repair and regeneration through biology: platelet-rich plasma as an alternative strategy. Arthritis Res Ther 15:220
Stoll TM, Dubois G, Schwarzenbach O (2002) The dynamic neutralization system for the spine: a multi-center study of a novel non-fusion system. Eur Spine J 11(Suppl 2):S170–S178
Senegas J (2002) Mechanical supplementation by non-rigid fixation in degenerative intervertebral lumbar segments: the Wallis system. Eur Spine J 11(Suppl 2):S164–169
Parchi PD, Evangelisti G, Vertuccio A, Piolanti N, Andreani L, Cervi V, Giannetti C, Calvosa G, Lisanti M (2014) Biomechanics of interspinous devices. Biomed Res Int. https://doi.org/10.1155/2014/839325
Son IN, Kim YH, Ha KY (2015) Long-term clinical outcomes and radiological findings and their correlation with each other after standard open discectomy for lumbar disc herniation. J Neurosurg Spine 22:179–184
Jarman JP, Arpinar VE, Baruah D, Klein AP, Maiman DJ, Muftuler TL (2014) Intervertebral disc height loss demonstrates the threshold of major pathological changes during degeneration. Eur Spine J 24:1944–1950
Hartmann F, Dietz SO, Hely H, Rommens PM, Gercek E (2011) Biomechanical effect of different interspinous devices on lumbar spinal range of motion under preload conditions. Arch Orthop Trauma Surg 131:917–926
Christie SD, Song JK, Fessler RG (2005) Dynamic interspinous process technology. Spine (Phila Pa 1976) 30:73–78
Erbulut DU, Zafarparandeh I, Hassan CR, Lazoglu I, Ozer AF (2015) Determination of the biomechanical effect of an interspinous process device on implanted and adjacent lumbar spinal segments using a hybrid testing protocol: a finite-element study. J Neurosurg Spine 23:200–208
Wilke HJ, Drumm J, Haussler K, Mack C, Steudel WI, Kettler A (2008) Biomechanical effect of different lumbar interspinous implants on flexibility and intradiscal pressure. Eur Spine J 17:1049–1056
Swanson KE, Lindsey DP, Hsu KY, Zucherman JF, Yerby SA (2003) The effects of an interspinous implant on intervertebral disc pressures. Spine (Phila Pa 1976) 28:26–32
Vaga S, Brayda-Bruno M, Perona F, Fornari M, Raimondi MT, Petruzzi M, Grava G, Costa F, Caiani EG, Lamartina C (2009) Molecular MR imaging for the evaluation of the effect of dynamic stabilization on lumbar intervertebral discs. Eur Spine J 18(Suppl 1):40–48
Ciavarro C, Caiani EG, Brayda-Bruno M, Zerbi A, Galbusera F, Vaga S, Lamartina C (2012) Mid-term evaluation of the effects of dynamic neutralization system on lumbar intervertebral discs using quantitative molecular MR imaging. J Magn Reson Imaging 35:1145–1151
Xu L, Yu X, Bi LY, Liu GZ, Li PY, Qu Y, Jiao Y (2012) Intermediate and long-term follow-up evaluation of posterior dynamic lumbar stabilization in lumbar degenerative disease. Zhonghua Wai Ke Za Zhi 50:792–796
Senegas J, Vital JM, Pointillart V, Mangione P (2009) Clinical evaluation of a lumbar interspinous dynamic stabilization device (the Wallis system) with a 13-year mean follow-up. Neurosurg Rev 32:335–341 (discussion 341–332)
Zhao Y, Wang YP, Qiu GX, Zhao H, Zhang JG, Zhou X (2010) Efficacy of the dynamic interspinous assisted motion system in clinical treatment of degenerative lumbar disease. Chin Med J 123:2974–2977
van den Akker-van Marle ME, Moojen WA, Arts MP, Vleggeert-Lankamp CL, Peul WC, Leiden-The Hague Spine Intervention Prognostic Study Group (2016) Interspinous process devices versus standard conventional surgical decompression for lumbar spinal stenosis: cost-utility analysis. Spine J 16:702–710
Smith ZA (2014) Interspinous process device versus standard conventional surgical decompression for lumbar spinal stenosis results in increased reoperation rates and costs without improving patient outcomes. Evid Based Med 19:136
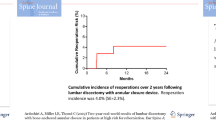
Floman Y, Millgram MA, Smorgick Y, Rand N, Ashkenazi E (2007) Failure of the Wallis interspinous implant to lower the incidence of recurrent lumbar disc herniations in patients undergoing primary disc excision. J Spinal Disord Tech 20:337–341
Sun HL, Li CD, Liu XY, Lin JR, Yi XD, Liu H, Lu HL (2011) Mid-term follow-up and analysis of the failure cases of interspinous implants for degenerative lumbar diseases. Beijing Da Xue Xue Bao 43:690–695
Aizawa T, Ozawa H, Kusakabe T, Nakamura T, Sekiguchi A, Takahashi A, Sasaji T, Tokunaga S, Chiba T, Morozumi N, Koizumi Y, Itoi E (2012) Reoperation for recurrent lumbar disc herniation: a study over a 20-year period in a Japanese population. J Orthop Sci 17:107–113
McGirt MJ, Eustacchio S, Varga P, Vilendecic M, Trummer M, Gorensek M, Ledic D, Carragee EJ (2009) A prospective cohort study of close interval computed tomography and magnetic resonance imaging after primary lumbar discectomy: factors associated with recurrent disc herniation and disc height loss. Spine (Phila Pa 1976) 34:2044–2051
Yue ZJ, Liu RY, Lu Y, Dong LL, Li YQ, Lu EB (2015) Middle-period curative effect of posterior lumbar intervertebral fusion (PLIF) and interspinous dynamic fixation (Wallis) for treatment of L45 degenerative disease and its influence on adjacent segment degeneration. Eur Rev Med Pharmacol Sci 19:4481–4487
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
Z. Zhou, X. Jin, C. Wang and L. Wang declare that they have no competing interests.
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1975 Helsinki declaration and its later amendments or comparable ethical standards. Informed consent was obtained from all individual participants included in the study.
Additional information
Zihui Zhou und Xinmeng Jin contributed equally to this work.
Rights and permissions
About this article
Cite this article
Zhou, Z., Jin, X., Wang, C. et al. Wallis interspinous device versus discectomy for lumbar disc herniation. Orthopäde 48, 165–169 (2019). https://doi.org/10.1007/s00132-018-3639-z
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00132-018-3639-z