Abstract
Background
Vertebral compression fractures are common in multiple myeloma. Percutaneous vertebroplasty is used to stabilize vertebral collapse and treat the pain. The major technical drawbacks of percutaneous vertebroplasty are the potential for neural comprise and pulmonary embolism of cement from leakage of polymethylmethacrylate into epidural space and perivertebral veins. We have retrospectively evaluated the safety and complication of percutaneous vertebroplasty in the vertebral compression fractures resulting from multiple myeloma.
Methods
From August 2003 to July 2008, we describe 24 patients with multiple myeloma who were treated for vertebral compression fractures with percutaneous vertebroplasty to a total of 36 vertebrae. There were 4 male and 20 female patients with an average age of 67 (range 54–81 years). The pain symptoms were measured on a visual analog pain scale and quality of life as measured by the physical component summary scale of the Short Form-36 before operation and at 24 h, at 3 months and at 1 year following vertebroplasty. Radiography was reviewed for evidence of cement leakage and pulmonary complication.
Results
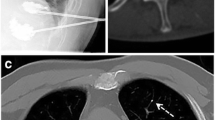
The mean visual analog pain scale decreased from a preoperative value of 9.0–3.8 at 24 h following operation and SF-36 score improved from 22.1 to 41.8. Of the twenty-four patients, four had cement leakage (2 leak through inferior endplate into disc, 2 leak into perivertebral vessels). There were no intra-postoperative neurologic or pulmonary complications. Eight patients died 2–18 months post-operatively due to multiple myeloma-related organ failure.
Conclusions
In this study, vertebroplasty significantly improved pain scores and function and, thereby, the quality of life. There were no major procedure-related complications in this study. Direct cytotoxic effect, polymerization and biomechanical microfractures stabilizer of polymethylmethacrylate play multiple roles in pain relief. In multiple myeloma, when pathological spinal compression fractures cause intractable pain and are unresponsive to conservative treatment, vertebroplasty remains the best option for pain relief and is effective in increasing quality of life.


Similar content being viewed by others
References
Kyle RA, Gertz MA, Witzig TE et al (2003) Review of 1,027 patients with newly diagnosed multiple myeloma. Mayo Clin Proc 78:21–33
Croucher PI, Apperley JF (1998) Bone disease in myeloma. Br J Haematol 103:902–910
Kumar A, Loughran T, Alsina M et al (2003) Management of multiple myeloma: a systematic review and critical appraisal of published studies. Lancet Oncol 4:293–304
Anderson KC (2003) Multiple myeloma: how far have we come? Mayo Clin Proc 78:15–17
Diamond T, Champion B, Clark W (2003) Management of acute osteoporotic vertebral fractures: a nonrandomised trial comparing percutaneous vertebroplasty with conservative therapy. Am J Med 114:257–265
Barragan-Campos HM, Vallee JN, Lo D et al (2006) Percutaneous vertebroplasty for spinal metastases: complications. Radiology 238(1):354–362
Ware J Jr, Kosinski M, Keller S (1994) SF-36 Physical and mental health summary scales: a user’s manual. The Health Institute, New England Medical Center, Boston
Lieberman I, Reinhardt MK (2003) Vertebroplasty and kyphoplasty for oste-olytic vertebral collapse. Clin Orthop 415(suppl):S176–S186
Jensen ME, Kallmes DE (2002) Percutaneous vertebroplasty in the treatment of malignant spinal disease. Cancer J 8:194–206
Diamond H, Hartwell T, Clarke W et al (2004) Percutaneous vertebroplasty for acute vertebral body fracture and deformity in multiple myeloma: a short report. Br J Hoematol 124(4):485–487
Lemke DM, Hacein-Bey L (2003) Metastatic compression fractures–vertebro-plasty for pain control. J Neurosci Nurs 35:50–55
Barr JD, Barr MS, Lemley TJ et al (2000) Percutaneous vertebroplasty for pain relief and spinal stabilization. Spine 25:923–928
Fourney DR, Schomer DF, Nader R et al (2003) Percutaneous vertebroplasty and kyphoplasty for painful vertebral body fractures in cancer patients. J Neurosurg 98(1 Suppl):21–30
Jensen ME, Kallmes DE (2002) Percutaneous vertebroplasty in the treatment of malignant spinal disease. Cancer J 8:194–206
Belkoff SM, Mathis JM, Jasper LE et al (2001) The biomechanics of vertebro- plasty. The effect of cement volume on mechanical behavior. Spine 26:1537–1541
Cotton A, Dewatr F, Cortet B et al (1996) Percutaneous vertebroplasty for osteolytic metastases and myeloma: effects of percentage of lesion filling and the leakage of methyl methacrylate at clinical follow-up. Radiology 200:525–530
Gangi A, Guth S, Imbert JP et al (2003) Percutaneous vertebroplasty: indications, technique, and results. Radiographics 23(2):e10
Lemke DM, Hacein-Bey L (2003) Metastatic compression fractures–vertebro-plasty for pain control. J Neurosci Nurs 35:50–55
Fourney DR, Schomer DF, Nader R et al (2003) Percutaneous vertebroplasty and kyphoplasty for painful vertebral body fractures in cancer patients. J Neurosurg Spine 98:21–30
Lieberman I, Reinhardt MK (2003) Vertebroplasty and kyphoplasty for oste-olytic vertebral collapse. Clin Orthop 415(suppl):S176–S186
Cosar M, Sasani M, Oktenoglu T et al (2009) The major complications of transpedicular vertebroplasty. J Neurosurg Spine 11(5):605–606
Jensen ME, Kallmes DE (2002) Percutaneous vertebroplasty in the treatment of malignant spinal disease. Cancer J 8:194–206
Phillips FM, Todd Wetzel F, Lieberman I, Campbell-Hupp M (2002) An in vivo comparison of the potential for extravertebral cement leak after vertebroplasty and kyphoplasty. Spine 27:2178–2179
Deramond H, Depriester C, Galibert P et al (1998) Percutaneous vertebro- plasty with polymethylmethacrylate: technique, indications, and results. Radiol Clin North Am 36:533–546
Deramond H, Wright NT, Belkoff SM (1999) Temperature elevation caused by bone cement polymerization during vertebroplasty. Bone 25(2 Suppl):17S–21S
Acknowledgments
We thank the Department of Orthopaedic Surgery for their contribution to the study.
Conflict of interest
The authors declare that they have no competing interests.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Chen, LH., Hsieh, MK., Niu, CC. et al. Percutaneous vertebroplasty for pathological vertebral compression fractures secondary to multiple myeloma. Arch Orthop Trauma Surg 132, 759–764 (2012). https://doi.org/10.1007/s00402-012-1474-y
Received:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00402-012-1474-y