Abstract
Study design
Retrospective cohort case study.
Objective
To evaluate significance of segmental instability (SI) in cervical ossification of the posterior longitudinal ligament (OPLL) myelopathy and effectiveness of a posterior hybrid technique in the treatment of OPLL associated with SI.
Summary and background data
Some studies suggested both static and dynamic compression factors accounted for the pathogenesis of myelopathy in the OPLL patients.
Method
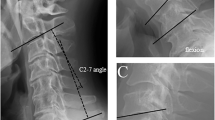
Between May 2005 and August 2007, 15 patients with multilevel cervical OPLL, diagnosed to be associated with SI, were treated by a posterior hybrid technique including laminoplasty and fusion at instable levels with lateral mass screw fixation. Another 15 cohort patients without SI treated by laminoplasty in the same period were included in the control group. Radiological and clinical data were compared between two groups.
Results
There were no significant differences in Preop. lordotic angle, extent of OPLL, type of OPLL and occupying rate, but more patients tended to present high-intensity zone (HIZ) on MRI in the group with SI. In 15 patients with SI, 17 intervertebral levels had SI, which were distributed at the noncontinuous levels of mixed-type OPLL or the adjacent levels of continuous-type OPLL. They were also consistent with the presence of HIZ levels in the major of patients. After operation, the lordotic angle was maintained well by the posterior hybrid technique in the OPLL with SI group, and was significantly greater than that in the OPLL without SI at the 3- and 4-year follow-up point. Postoperative kyphotic change of the cervical spine and postoperative progression of the ossified lesion were not observed in the OPLL with SI group, but they were respectively observed in four cases (26.7 %) and two cases (13.3 %) in the OPLL without SI group at the 4-year follow-up point. The preoperative C-JOA score in the OPLL with SI group was lower than that in the OPLL without SI group. The average C-JOA score and improvement rate were comparable in the first 2 years after operation between two groups, but there was a decrease in C-JOA score and improvement rate in the following 2 years in the OPLL without SI group. At the 3- and 4-year follow-up points, both postoperative C-JOA score improvement rate in the OPLL with SI group were superior to those in the OPLL without SI group. Each group had one case developing C5 palsy, but three cases in the OPLL without SI group developed late neurological deterioration due to postoperative kyphotic change or progression of the ossified lesion.
Conclusions
Segmental instability, a degenerative dynamic factor, is important to the OPLL myelopathy. The posterior hybrid technique seemed to be effective and safe in the treatment of selective OPLL patients associated with SI. The benefits may include providing stabilization environment for spinal cord recovery, and preventing progressive kyphotic change and progression of OPLL.




Similar content being viewed by others
References
Azuma Y, Kato Y, Taguchi T (2010) Etiology of cervical myelopathy induced by ossification of the posterior longitudinal ligament: determining the responsible level of OPLL myelopathy by correlating static compression and dynamic factors. J Spinal Disord Tech 23:166–169
Chen Y, Guo YF, Chen DY et al (2009) Long-term outcome of laminectomy and instrumented fusion for cervical ossification of the posterior longitudinal ligament. Int Orthop 33:1075–1080
Chiba K, Yamamoto I, Hirabayashi H et al (2005) Multicenter study investigating the postoperative progression of ossification of the posterior longitudinal ligament in the cervical spine: a new computer-assisted measurement. J Neurosurg Spine 3:17–23
Hirabayashi K, Watanabe K, Wakano K et al (1983) Expansive open-door laminoplasty for cervical spinal stenotic myelopathy. Spine 8:693–699
Hori T, Kawaguchi Y, Kimura T (2007) How does the ossification area of the posterior longitudinal ligament thicken following cervical laminoplasty? Spine 32:E551–E556
Houten JK, Cooper PR (2003) Laminectomy and posterior cervical plating for multilevel cervical spondylotic myelopathy and ossification of the posterior longitudinal ligament: effects on cervical alignment, spinal cord compression, and neurological outcome. Neurosurgery 52:1081–1088
Iwasaki M, Kawaguchi Y, Kimura T et al (2002) Long-term results of expansive laminoplasty for ossification of the posterior longitudinal ligament of the cervical spine: more than 10 years follow up. J Neurosurg 96(Suppl 2):180–189
Kato Y, Iwasaki M, Fuji T et al (1998) Long-term follow-up results of laminectomy for cervical myelopathy caused by ossification of the posterior longitudinal ligament. J Neurosurg 89:217–223
Kawaguchi Y, Kanamori M, Ishihara H et al (2001) Progression of ossification of the posterior longitudinal ligament following an bloc cervical laminoplasty. J Bone Jt Surg Am 83A:1798–1802
Koyanagi I, Iwasaki Y, Hida K et al (2003) Acute cervical cord injury associated with ossification of the posterior longitudinal ligament. Neurosurgery 53:887–892
Matsumura A, Yanaka K, Akutsu H et al (2003) Combined laminoplasty with posterior lateral mass plate for unstable spondylotic cervical canal stenosis. Neurol Med Chir (Tokyo) 43:514–519
Matsunaga S, Kukita M, Hayashi K et al (2002) Pathogenesis of myelopathy in patients with ossification of the posterior longitudinal ligament. J Neurosurg 96:168–172
Mochizuki M, Aiba A, Hashimoto M et al (2009) Cervical myelopathy in patients with ossification of the posterior longitudinal ligament. J Neurosurg Spine 10:122–128
Ogawa Y, Toyama Y, Chiba K et al (2004) Long-term results of expansive open-door laminoplasty for ossification of the posterior longitudinal ligament of the cervical spine. J Neurosurg Spine 1:168–174
Sakaura H, Hosono N, Mukai Y et al (2003) C5 palsy after decompression surgery for cervical myelopathy. Spine 28:2447–2451
Sakai K, Okawa A, Takahashi M et al (2012) Five-year follow-up evaluation of surgical treatment for cervical myelopathy caused by OPLL: a prospective comparative study of anterior decompression and fusion with floating method versus laminoplasty. Spine 37:367–376
Sun Q, Hu H, Zhang Y et al (2011) Do intramedullary spinal cord changes in signal intensity on MRI affect surgical opportunity and approach for cervical myelopathy due to ossification of the posterior longitudinal ligament? Eur Spine J 20:1466–1473
White AA, Johnson RM, Panjabi MM et al (1975) Biomechanical analysis of clinical stability in the cervical spine. Clin Orthop 109:85–96
Conflict of interest
No funds were received in supported of this work. No benefits in any form have been or will be received from a commercial party related directly or indirectly to the subject of this manuscript.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Chen, Y., Chen, D., Wang, X. et al. Significance of segmental instability in cervical ossification of the posterior longitudinal ligament and treated by a posterior hybrid technique. Arch Orthop Trauma Surg 133, 171–177 (2013). https://doi.org/10.1007/s00402-012-1658-5
Received:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00402-012-1658-5