Abstract
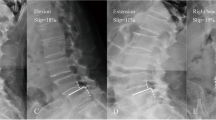
Few studies have investigated the factors related to the disability and physical function in degenerative lumbar spondylolisthesis using axially loaded magnetic resonance imaging (MRI). Therefore, we aimed to investigate the effect of axial loading on the morphology of the spine and the spinal canal in patients with degenerative spondylolisthesis of L4–5 and to correlate morphologic changes to their disability and physical functions. From March 2003 to January 2004, 32 consecutive cases (26 females, 6 males) with degenerative L4–5 spondylolisthesis, grade 1–2, intermittent claudication, and low back pain without sciatica were included in this study. All patients underwent unloaded and axially loaded MRI of the lumbo-sacral spine in supine position to elucidate the morphological findings and to measure the parameters of MRI, including disc height (DH), sagittal translation (ST), segmental angulation (SA), dural sac cross-sectional area (DCSA) at L4–5, and lumbar lordotic angles (LLA) at L1–5 between the unloaded and axially loaded condition. Each patient’s disability was evaluated by the Oswestry Disability Index (ODI) questionnaire, and physical functioning (PF) was evaluated by the Physical Function scale proposed by Stucki et al. (Spine 21:796–803, 1996). Three patients were excluded due to the presence of neurologic symptoms found with the axially loaded MRI. Finally, a total of 29 (5 males, 24 females) consecutive patients were included in this study. Comparisons and correlations were done to determine which parameters were critical to the patient’s disability and PF. The morphologies of the lumbar spine changed after axially loaded MRI. In six of our patients, we observed adjacent segment degeneration (4 L3–L4 and 2 L5–S1) coexisting with degenerative spondylolisthesis of L4–L5 under axially loaded MRI. The mean values of the SA under pre-load and post-load were 7.14° and 5.90° at L4–L5 (listhetic level), respectively. The mean values of the LLA under pre-load and post-load were 37.03° and 39.28°, respectively. There were significant correlations only between the ODI, PF, and the difference of SA, and between PF and the post-loaded LLA. The changes in SA (L4–L5) during axial loading were well correlated to the ODI and PF scores. In addition, the LLA (L1–L5) under axial loading was well correlated to the PF of patients with degenerative L4–L5 spondylolisthesis. We suggest that the angular instability of the intervertebral disc may play a more important role than neurological compression in the pathogenesis of disability in degenerative lumbar spondylolisthesis.


Similar content being viewed by others
References
Boden SD, Wiesel SW (1990) Lumbosacral segmental motion in normal individuals: have we been measuring instability properly? Spine 15:571–576. doi:10.1097/00007632-199006000-00026
Caputy AJ, Luessenhop AJ (1992) Long-term evaluation of decompressive surgery for degenerative lumbar stenosis. J Neurosurg 77:669–676
Cartolari R, Argento G, Cardello P et al (1998) Axial loaded computed tomography (AL-CT), and cine AL-CT. Riv Neuroradiol 11:275–286
Danielson B, Willen J (2001) Axially loaded magnetic resonance image of the lumbar spine in asymptomatic individuals. Spine 26:2601–2606. doi:10.1097/00007632-200112010-00015
Danielson BI, Willen J, Gaulitz A et al (1998) Axial loading of the spine during CT and MR in patients with suspected lumbar spinal stenosis. Acta Radiol 39:604–611
Dupuis PR, Yong-Hing K, Cassidy JD et al (1985) Radiological diagnosis of degenerative lumbar spinal instability. Spine 10:262–266. doi:10.1097/00007632-198504000-00015
Fairbank JC, Couper J, Davies JB et al (1980) The Oswestry low back pain disability questionnaire. Physiotherapy 66:271–273
Fritz JM, Delitto A, Welch WC et al (1998) Lumbar spinal stenosis: a review of current concepts in evaluation, management, and outcome measurements. Arch Phys Med Rehabil 79:700–708. doi:10.1016/S0003-9993(98)90048-X
Fujiwara A, Lim TH, An HS et al (2000) The effect of disc degeneration and facet joint osteoarthritis on the segmental flexibility of the lumbar spine. Spine 25:3036–3044. doi:10.1097/00007632-200012010-00011
Hanley EN Jr (1995) The indications for lumbar spinal fusion with and without instrumentation. Spine 20(suppl):143–153. doi:10.1097/00007632-199512151-00012
Hiwatashi A, Danielson B, Moritani T et al (2004) Axial loading during MR imaging can influence treatment decision for symptomatic spinal stenosis. AJNR Am J Neuroradiol 25:170–174
Iguchi T, Kanemura A, Kasahara K et al (2004) Lumbar instability and clinical symptoms: which is the more critical factor for symptoms: sagittal translation or segment angulation? J Spinal Disord Tech 4:284–290. doi:10.1097/01.bsd.0000102473.95064.9d
Jayakumar P, Nnadi C, Saifuddin A et al (2006) Dynamic degenerative lumbar spondylolisthesis: diagnosis with axial loaded magnetic resonance imaging. Spine 31:E298–E301. doi:10.1097/01.brs.0000216602.98524.07
Morgan FP, King T (1957) Primary instability of lumbar vertebrae as a common cause of low back pain. J Bone Joint Surg Br 39:6–22
Soini J, Antti-Poika I, Tallroth K et al (1991) Disc degeneration and angular movement of the lumbar spine comparative study using plain and flexion–extension radiography and discography. J Spinal Disord 4:183–187. doi:10.1097/00002517-199106000-00008
Stucki G, Daltroy L, Liang MH et al (1996) Measurement properties of a self-administered outcome measure in lumbar spinal stenosis. Spine 21:796–803. doi:10.1097/00007632-199604010-00004
Willen J, Danielson B, Gaulitz A et al (1997) Dynamic effects on the lumbar spinal canal: axially loaded CT-myelography and MRI in patients with sciatica and/or neurogenic claudication. Spine 22:2968–2976. doi:10.1097/00007632-199712150-00021
Acknowledgments
The authors did not receive any outside funding or grants in support of their research for or preparation of this work. Neither they nor a member of their immediate families received payments or other benefits or a commitment or agreement to provide such benefits from a commercial entity. No commercial entity paid or directed, or agreed to pay or direct, any benefits to any research fund, foundation, division, center, clinical practice, or other charitable or nonprofit organization with which the authors, or a member of their immediate families, are affiliated or associated.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Huang, KY., Lin, RM., Lee, YL. et al. Factors affecting disability and physical function in degenerative lumbar spondylolisthesis of L4–5: evaluation with axially loaded MRI. Eur Spine J 18, 1851–1857 (2009). https://doi.org/10.1007/s00586-009-1059-9
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00586-009-1059-9