Abstract
Purpose
The effectiveness of vertebral augmentation techniques is a currently highly debated issue. The biomechanical literature suggests that cement filling volumes may play an important role in the “dosage” of vertebral augmentation and its pain alleviating effect. Good clinical data about filling volumes are scarce and most patient series are small. Therefore, we investigated the predictors of pain alleviation after balloon kyphoplasty in the nationwide SWISSspine registry where cement volumes are also recorded.
Methods
All single-level vertebral fractures with no additional fracture stabilization and availability of at least one follow-up within 6 months after surgery were included. The following potential predictors were assessed in a multivariate logistic regression model with the group’s average pain alleviation of 41 points on VAS as the desired outcome: patient age, patient sex, diagnosis, preoperative pain, level of fracture, type of fracture, age of fracture, segmental kyphotic deformity, cement volume, vertebral body filling volume, and cement extrusions.
Results
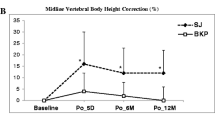
There were 194 female and 82 males with an average age of 70.4 and 65.3 years, respectively. Female patients were about twice as likely for achieving the average pain relief compared to males (p = 0.04). The preoperative pain level was the strongest predictor in that the likelihood for achieving an at least 41-point pain relief increased by about 8 % with each additional point of preoperative pain (p < 0.001). A thoraco-lumbar fracture had a three times higher odds for the average pain relief compared with a lumbar fracture (p = 0.03). An A.3.1 fracture only had about a third of the probability for average pain relief compared with an A.1.1 fracture (p = 0.004). Cement volumes up to 4.5 ml only had an approximately 40 % chance for a minimum 41-point pain alleviation as compared with cement volumes of at least 4.5 ml (p = 0.007). In addition, the relationship between cement volume and pain alleviation followed a dose-dependent pattern.
Conclusions
Cement volume was revealed as a significant predictor for pain relief in BKP. Cement volume was the third most important influential covariate and the most important modifiable and operator dependent one. The clear dose-outcome relationship between cement filling volumes and pain relief additionally supports these findings. Cement volumes of >4.5 ml seem to be recommendable for achieving relevant pain alleviation. Patient sex and fracture type and location were further significant predictors and all these covariates should be recorded and reported in future studies about the pain alleviating effectiveness of vertebral augmentation procedures.



Similar content being viewed by others
References
Buchbinder R, Kallmes D, Glasziou P (2010) Vertebroplasty versus conservative treatment for vertebral fractures. Lancet 376:2070–2071; author reply 2071–2072. doi:10.1016/S0140-6736(10)62288-X
Kallmes DF, Comstock BA, Heagerty PJ, Turner JA, Wilson DJ, Diamond TH, Edwards R, Gray LA, Stout L, Owen S, Hollingworth W, Ghdoke B, Annesley-Williams DJ, Ralston SH, Jarvik JG (2009) A randomized trial of vertebroplasty for osteoporotic spinal fractures. N Engl J Med 361:569–579. doi:10.1056/NEJMoa0900563
Aebi M (2009) Vertebroplasty: about sense and nonsense of uncontrolled “controlled randomized prospective trials”. Eur Spine J 18:1247–1248. doi:10.1007/s00586-009-1164-9
Bono CM, Heggeness M, Mick C, Resnick D, Watters WC 3rd (2010) North American Spine Society: newly released vertebroplasty randomized controlled trials: a tale of two trials. Spine J 10:238–240. doi:10.1016/j.spinee.2009.09.007
Klazen CA, Lohle PN, de Vries J, Jansen FH, Tielbeek AV, Blonk MC, Venmans A, van Rooij WJ, Schoemaker MC, Juttmann JR, Lo TH, Verhaar HJ, van der Graaf Y, van Everdingen KJ, Muller AF, Elgersma OE, Halkema DR, Fransen H, Janssens X, Buskens E, Mali WP (2010) Vertebroplasty versus conservative treatment in acute osteoporotic vertebral compression fractures (Vertos II): an open-label randomised trial. Lancet 376:1085–1092. doi:10.1016/S0140-6736(10)60954-3
Boszczyk B (2010) Volume matters: a review of procedural details of two randomised controlled vertebroplasty trials of 2009. Eur Spine J 19:1837–1840. doi:10.1007/s00586-010-1525-4
Melloh M, Roder C, Staub LP, Zweig T, Barz T, Theis JC, Muller U (2011) Randomized-controlled trials for surgical implants: are registries an alternative? Orthopedics 34:161. doi:10.3928/01477447-20110124-03
Diel P, Reuss W, Aghayev E, Moulin P, Roder C (2010) SWISSspine-a nationwide health technology assessment registry for balloon kyphoplasty: methodology and first results. Spine J 10:961–971. doi:10.1016/j.spinee.2009.08.452
Cochrane AL (1989) Archie Cochrane in his own words. Selections arranged from his 1972 introduction to “Effectiveness and efficiency: random reflections on the health services” 1972. Control Clin Trials 10:428–433
Limthongkul W, Karaikovic EE, Savage JW, Markovic A (2010) Volumetric analysis of thoracic and lumbar vertebral bodies. Spine J 10:153–158. doi:10.1016/j.spinee.2009.11.018
Ioannou M, Roumeliotis G, Limaxis E, Theodorou O (2010) Efficacy and safety of balloon kyphoplasty-are high cement volumes required? Internet J Minim Invasive Spinal Technol 5(Supplement III to IJMIST IV). doi:10.5580/22af
Luo J, Daines L, Charalambous A, Adams MA, Annesley-Williams DJ, Dolan P (2009) Vertebroplasty: only small cement volumes are required to normalize stress distributions on the vertebral bodies. Spine (Phila Pa 1976) 34:2865–2873. doi:10.1097/BRS.0b013e3181b4ea1e
Molloy S, Mathis JM, Belkoff SM (2003) The effect of vertebral body percentage fill on mechanical behavior during percutaneous vertebroplasty. Spine (Phila Pa 1976) 28:1549–1554
Liebschner MA, Rosenberg WS, Keaveny TM (2001) Effects of bone cement volume and distribution on vertebral stiffness after vertebroplasty. Spine (Phila Pa 1976) 26:1547–1554
Grafe I, Nöldge G, Weiss C, Libicher M, Baier M, Nawroth P, Meeder P-J, Wiedenhöfer B, Kasperk C (2011) Prediction of immediate and long-term benefit after kyphoplasty of painful osteoporotic vertebral fractures by preoperative MRI. Eur J Trauma Emerg Surg 37:7
Karam M, Lavelle WF, Cheney R (2008) The role of bone scintigraphy in treatment planning, and predicting pain relief after kyphoplasty. Nucl Med Commun 29:247–253. doi:10.1097/MNM.0b013e3282f30598
Alvarez L, Perez-Higueras A, Granizo JJ, de Miguel I, Quinones D, Rossi RE (2005) Predictors of outcomes of percutaneous vertebroplasty for osteoporotic vertebral fractures. Spine (Phila Pa 1976) 30:87–92
Kaufmann TJ, Trout AT, Kallmes DF (2006) The effects of cement volume on clinical outcomes of percutaneous vertebroplasty. AJNR Am J Neuroradiol 27:1933–1937
Ren H, Shen Y, Zhang YZ, Ding WY, Xu JX, Yang DL, Cao JM (2010) Correlative factor analysis on the complications resulting from cement leakage after percutaneous kyphoplasty in the treatment of osteoporotic vertebral compression fracture. J Spinal Disord Tech 23:e9–e15. doi:10.1097/BSD.0b013e3181c0cc94
Georgy BA (2010) Clinical experience with high-viscosity cements for percutaneous vertebral body augmentation: occurrence, degree, and location of cement leakage compared with kyphoplasty. AJNR Am J Neuroradiol 31:504–508. doi:10.3174/ajnr.A1861
Rapan S, Jovanovic S, Gulan G, Boschi V, Kolarevic V, Dapic T (2010) Vertebroplasty—high viscosity cement versus low viscosity cement. Coll Antropol 34:1063–1067
Anselmetti GC, Zoarski G, Manca A, Masala S, Eminefendic H, Russo F, Regge D (2008) Percutaneous vertebroplasty and bone cement leakage: clinical experience with a new high-viscosity bone cement and delivery system for vertebral augmentation in benign and malignant compression fractures. Cardiovasc Intervent Radiol 31:937–947. doi:10.1007/s00270-008-9324-6
Acknowledgments
We are thankful to the Swiss Spine Society and the SWISSspine registry group who made this research possible by populating the database with their valuable and much appreciated entries. The Kyphoplasty group contributing data to the current study is comprised of the 47 following surgeons (in order of case contribution): Maestretti G (70 cases), Forster T (64 cases), Schueler M (59 cases), Sgier F (58 cases), Aebi M (50 cases), Beele B (39 cases), Bärlocher C (32 cases), Kroeber M (28 cases), Schaeren S (26 cases), Broger I (24 cases), Blay M (23 cases), Etter C (21 cases), Mueller U (20 cases), Mueller K (20 cases), Berlemann U (19 cases), Binkert C (14 cases), Moulin P (12 cases), Lutz T (11 case), Sheikh-Sarraf B (9 cases), Schwarz U (9 cases), Heimberger K (8 cases), Kuehlling F (8 cases), Morard M (7 cases), Otten P (7 cases), Stoll T (7 cases), Kunz S (6 cases), Martinez R (6 cases), Tessitore E (6 cases), Jeanneret B (5 cases), Payer M (5 cases), Baur M (4 cases), Hamburger C (4 cases), Markwalder T (4 cases), Hausmann O (3 cases), Schirm A (3 cases), Van Dommelen K (3 cases), Heinzelmann M (2 cases), Panche T (2 cases), Schwarzenbach O (2 cases), Wanner G (2 cases), Bachmann M (1 case), Bothmann M (1 case), Koehler M (1 case), Ramadan A (1 case), Schizas C (1 case), Vernet O (1 case), Witzmann A (1 case).
There was no external source of funding for the current study.
Conflict of interest
None.
Author information
Authors and Affiliations
Corresponding author
Additional information
On behalf of the SWISSspine Registry Group.
Rights and permissions
About this article
Cite this article
Röder, C., Boszczyk, B., Perler, G. et al. Cement volume is the most important modifiable predictor for pain relief in BKP: results from SWISSspine, a nationwide registry. Eur Spine J 22, 2241–2248 (2013). https://doi.org/10.1007/s00586-013-2869-3
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00586-013-2869-3