Abstract
Purpose
This study evaluated differences in outcome variables between percutaneous, traditional, and paraspinal posterior open approaches for traumatic thoracolumbar fractures without neurologic deficit.
Methods
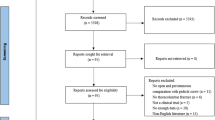
A systematic review of PubMed, Cochrane, and Embase was performed. In this meta-analysis, we conducted online searches of PubMed, Cochrane, Embase using the search terms “thoracolumbar fractures”, “lumbar fractures”, ‘‘percutaneous’’, “minimally invasive”, ‘‘open”, “traditional”, “posterior”, “conventional”, “pedicle screw”, “sextant”, and “clinical trial”. The analysis was performed on individual patient data from all the studies that met the selection criteria. Clinical outcomes were expressed as risk difference for dichotomous outcomes and mean difference for continuous outcomes with 95 % confidence interval. Heterogeneity was assessed using the χ 2 test and I 2 statistics.
Results
There were 4 randomized controlled trials and 14 observational articles included in this analysis. Percutaneous approach was associated with better ODI score, less Cobb angle correction, less Cobb angle correction loss, less postoperative VBA correction, and lower infection rate compared with open approach. Percutaneous approach was also associated with shorter operative duration, longer intraoperative fluoroscopy, less postoperative VAS, and postoperative VBH% in comparison with traditional open approach. No significant difference was found in Cobb angle correction, postoperative VBA, VBA correction loss, Postoperative VBH%, VBH correction loss, and pedicle screw misplacement between percutaneous approach and open approach. There was no significant difference in operative duration, intraoperative fluoroscopy, postoperative VAS, and postoperative VBH% between percutaneous approach and paraspianl approach.
Conclusions
The functional and the radiological outcome of percutaneous approach would be better than open approach in the long term. Although trans-muscular spatium approach belonged to open fixation methods, it was strictly defined as less invasive approach, which provided less injury to the paraspinal muscles and better reposition effect.









Similar content being viewed by others
References
Sihvonen T, Herno A, Paljarvi L, Airaksinen O, Partanen J, Tapaninaho A (1993) Local denervation atrophy of paraspinal muscles in postoperative failed back syndrome. Spine (Phila Pa 1976) 18:575–581
Muller U, Berlemann U, Sledge J, Schwarzenbach O (1999) Treatment of thoracolumbar burst fractures without neurologic deficit by indirect reduction and posterior instrumentation: bisegmental stabilization with monosegmental fusion. Eur Spine J 8:284–289
Magerl F, Aebi M, Gertzbein SD, Harms J, Nazarian S (1994) A comprehensive classification of thoracic and lumbar injuries. Eur Spine J 3:184–201
De Iure F, Cappuccio M, Paderni S, Bosco G, Amendola L (2012) Minimal invasive percutaneous fixation of thoracic and lumbar spine fractures. Minim Invasive Surg 2012:141032. doi:10.1155/2012/141032
Verlaan JJ, Diekerhof CH, Buskens E, van der Tweel I, Verbout AJ, Dhert WJ, Oner FC (2004) Surgical treatment of traumatic fractures of the thoracic and lumbar spine: a systematic review of the literature on techniques, complications, and outcome. Spine (Phila Pa 1976) 29:803–814
Lee JK, Jang JW, Kim TW, Kim TS, Kim SH, Moon SJ (2013) Percutaneous short-segment pedicle screw placement without fusion in the treatment of thoracolumbar burst fractures: is it effective? Comparative study with open short-segment pedicle screw fixation with posterolateral fusion. Acta Neurochir (Wien) 155(2305–2312):2312. doi:10.1007/s00701-013-1859-x
Lyu J, Chen K, Tang Z, Chen Y, Li M, Zhang Q (2016) A comparison of three different surgical procedures in the treatment of type A thoracolumbar fractures: a randomized controlled trial. Int Orthop. doi:10.1007/s00264-016-3129-z
Zairi F, Court C, Tropiano P, Charles YP, Tonetti J, Fuentes S, Litrico S, Deramond H, Beaurain J, Orcel P, Delecrin J, Aebi M, Assaker R (2012) Minimally invasive management of thoraco-lumbar fractures: combined percutaneous fixation and balloon kyphoplasty. Orthop Traumatol Surg Res 98:S105–S111. doi:10.1016/j.otsr.2012.06.004
McAnany SJ, Overley SC, Kim JS, Baird EO, Qureshi SA, Anderson PA (2016) Open versus minimally invasive fixation techniques for thoracolumbar trauma: a meta-analysis. Global Spine J 6:186–194. doi:10.1055/s-0035-1554777
Phan K, Rao PJ, Mobbs RJ (2015) Percutaneous versus open pedicle screw fixation for treatment of thoracolumbar fractures: systematic review and meta-analysis of comparative studies. Clin Neurol Neurosurg 135:85–92. doi:10.1016/j.clineuro.2015.05.016
Wang H, Zhou Y, Li C, Liu J, Xiang L (2016) Comparison of open versus percutaneous pedicle screw fixation using the sextant system in the treatment of traumatic thoracolumbar fractures. Clin Spine Surg. doi:10.1097/BSD.0000000000000135
Cheng HQ, Li GQ, Sun SH, Ma WH, Ruan CY, Zhao HG, Xu RM (2015) Mini-open trans-spatium intermuscular versus percutaneous short-segment pedicle fixation for the treatment of thoracolumbar mono-segmental vertebral fractures. Zhongguo Gu Shang 28:1008–1012
Chi YL, Xu HZ, Lin Y, Huang QS, Mao FM, Ni WF (2004) Preliminary study of the technique of minimally invasive percutaneous pedicle screws osteosynthesis for treatment of thoraco-lumbar vertebra fracture. Zhonghua Wai Ke Za Zhi 42:1307–1311
Dong SH, Chen HN, Tian JW, Xia T, Wang L, Zhao QH, Liu CY (2013) Effects of minimally invasive percutaneous and trans-spatium intermuscular short-segment pedicle instrumentation on thoracolumbar mono-segmental vertebral fractures without neurological compromise. Orthop Traumatol Surg Res 99:405–411. doi:10.1016/j.otsr.2012.12.020
Grass R, Biewener A, Dickopf A, Rammelt S, Heineck J, Zwipp H (2006) Percutaneous dorsal versus open instrumentation for fractures of the thoracolumbar border. A comparative, prospective study. Unfallchirurg 109:297–305. doi:10.1007/s00113-005-1037-6
Grossbach AJ, Dahdaleh NS, Abel TJ, Woods GD, Dlouhy BJ, Hitchon PW (2013) Flexion-distraction injuries of the thoracolumbar spine: open fusion versus percutaneous pedicle screw fixation. Neurosurg Focus 35:E2. doi:10.3171/2013.6.FOCUS13176
Jiang XZ, Tian W, Liu B, Li Q, Zhang GL, Hu L, Li Z, He D (2012) Comparison of a paraspinal approach with a percutaneous approach in the treatment of thoracolumbar burst fractures with posterior ligamentous complex injury: a prospective randomized controlled trial. J Int Med Res 40:1343–1356
Ma YQ, Li XL, Dong J, Wang HR, Zhou XG, Li C (2012) Comparison of percutaneous versus open monosegment instrumentation in the treatment of incomplete thoracolumbar burst fracture. Zhonghua Yi Xue Za Zhi 92:904–908
Ming JH, Zheng HF, Zhao Q, Chen Q, Wang G (2014) Sextant percutaneous pedicle screw fixation for correcting single-segment thoracolumbar fractures. Chin J Tissue Eng Res 18:5654–5659
Nie FF, Zhang YH, Huang SG, Ju L, Chen B (2014) Minimally invasive percutaneous pedicle screw fixation versus open surgery for thoracolumbar fracture: Cobb’s angle and vertebral height. Chin J Tissue Eng Res 18:7094–7099
Peng XZ, Xiao KK (2014) Minimally invasive versus open pedicle screw fixation for repair of thoracolumbar fractures. Chin J Tissue Eng Res 18:4212–4218
Fitschen-Oestern S, Scheuerlein F, Weuster M, Klueter T, Menzdorf L, Varoga D, Kopetsch C, Mueller M, van der Horst A, Seekamp A, Behrendt P, Lippross S (2015) Reduction and retention of thoracolumbar fractures by minimally invasive stabilisation versus open posterior instrumentation. Injury 46(Suppl 4):S63–S70. doi:10.1016/S0020-1383(15)30020-6
Tian W, Han X, He D, Liu B, Li Q, Li ZY, Liu YJ, Li N (2011) The comparison of computer assisted minimally invasive spine surgery and traditional open treatment for thoracolumbar fractures. Zhonghua Wai Ke Za Zhi 49:1061–1066
Vanek P, Bradac O, Konopkova R, de Lacy P, Lacman J, Benes V (2014) Treatment of thoracolumbar trauma by short-segment percutaneous transpedicular screw instrumentation: prospective comparative study with a minimum 2-year follow-up. J Neurosurg Spine 20:150–156. doi:10.3171/2013.11.SPINE13479
Wild MH, Glees M, Plieschnegger C, Wenda K (2007) Five-year follow-up examination after purely minimally invasive posterior stabilization of thoracolumbar fractures: a comparison of minimally invasive percutaneously and conventionally open treated patients. Arch Orthop Trauma Surg 127:335–343. doi:10.1007/s00402-006-0264-9
Xue F, Fu ZG, Zhang DY, Zhang PX, Zhou J, Jiang BG (2013) Minimal invasive internal fixation with U-shaped break-off pedicle screws for treatment of thoracolumbar fractures. Beijing Da Xue Xue Bao 45:728–731
Wiltse LL, Bateman JG, Hutchinson RH, Nelson WE (1968) The paraspinal sacrospinalis-splitting approach to the lumbar spine. J Bone Joint Surg Am 50:919–926
Pang W, Zhang GL, Tian W, Sun D, Li N, Yuan Q, Zhang B, Wang YQ, Liu W (2009) Surgical treatment of thoracolumbar fracture through an approach via the paravertebral muscle. Orthop Surg 1:184–188. doi:10.1111/j.1757-7861.2009.00032.x
Assaker R (2004) Minimal access spinal technologies: state-of-the-art, indications, and techniques. Joint Bone Spine 71:459–469. doi:10.1016/j.jbspin.2004.08.006
Palmisani M, Gasbarrini A, Brodano GB, De Iure F, Cappuccio M, Boriani L, Amendola L, Boriani S (2009) Minimally invasive percutaneous fixation in the treatment of thoracic and lumbar spine fractures. Eur Spine J 18(Suppl 1):71–74. doi:10.1007/s00586-009-0989-6
Tezer M, Erturer RE, Ozturk C, Ozturk I, Kuzgun U (2005) Conservative treatment of fractures of the thoracolumbar spine. Int Orthop 29:78–82. doi:10.1007/s00264-004-0619-1
Lehmann W, Ushmaev A, Ruecker A, Nuechtern J, Grossterlinden L, Begemann PG, Baeumer T, Rueger JM, Briem D (2008) Comparison of open versus percutaneous pedicle screw insertion in a sheep model. Eur Spine J 17:857–863. doi:10.1007/s00586-008-0652-7
Vaccaro AR, Lehman RJ, Hurlbert RJ, Anderson PA, Harris M, Hedlund R, Harrop J, Dvorak M, Wood K, Fehlings MG, Fisher C, Zeiller SC, Anderson DG, Bono CM, Stock GH, Brown AK, Kuklo T, Oner FC (2005) A new classification of thoracolumbar injuries: the importance of injury morphology, the integrity of the posterior ligamentous complex, and neurologic status. Spine (Phila Pa 1976) 30:2325–2333
Kumar A, Aujla R, Lee C (2015) The management of thoracolumbar burst fractures: a prospective study between conservative management, traditional open spinal surgery and minimally interventional spinal surgery. Springerplus 4:204. doi:10.1186/s40064-015-0960-4
Dai LY, Jiang LS, Jiang SD (2009) Posterior short-segment fixation with or without fusion for thoracolumbar burst fractures. a five to seven-year prospective randomized study. J Bone Joint Surg Am 91:1033–1041. doi:10.2106/JBJS.H.00510
Cimatti M, Forcato S, Polli F, Miscusi M, Frati A, Raco A (2013) Pure percutaneous pedicle screw fixation without arthrodesis of 32 thoraco-lumbar fractures: clinical and radiological outcome with 36-month follow-up. Eur Spine J 22(Suppl 6):S925–S932. doi:10.1007/s00586-013-3016-x
Pishnamaz M, Oikonomidis S, Knobe M, Horst K, Pape HC, Kobbe P (2015) Open versus percutaneous stabilization of thoracolumbar spine fractures: a short-term functional and radiological follow-up. Acta Chir Orthop Traumatol Cech 82:274–281
Park Y, Ha JW, Lee YT, Sung NY (2011) Percutaneous placement of pedicle screws in overweight and obese patients. Spine J 11:919–924. doi:10.1016/j.spinee.2011.07.029
Youkilis AS, Quint DJ, McGillicuddy JE, Papadopoulos SM (2001) Stereotactic navigation for placement of pedicle screws in the thoracic spine. Neurosurgery 48(771–778):778–779
Fraser J, Gebhard H, Irie D, Parikh K, Hartl R (2010) Iso-C/3-dimensional neuronavigation versus conventional fluoroscopy for minimally invasive pedicle screw placement in lumbar fusion. Minim Invasive Neurosurg 53:184–190. doi:10.1055/s-0030-1267926
Tenney JH, Vlahov D, Salcman M, Ducker TB (1985) Wide variation in risk of wound infection following clean neurosurgery. Implications for perioperative antibiotic prophylaxis. J Neurosurg 62:243–247. doi:10.3171/jns.1985.62.2.0243
Milstone AM, Maragakis LL, Townsend T, Speck K, Sponseller P, Song X, Perl TM (2008) Timing of preoperative antibiotic prophylaxis: a modifiable risk factor for deep surgical site infections after pediatric spinal fusion. Pediatr Infect Dis J 27:704–708. doi:10.1097/INF.0b013e31816fca72
Picada R, Winter RB, Lonstein JE, Denis F, Pinto MR, Smith MD, Perra JH (2000) Postoperative deep wound infection in adults after posterior lumbosacral spine fusion with instrumentation: incidence and management. J Spinal Disord 13:42–45
Kuo CH, Wang ST, Yu WK, Chang MC, Liu CL, Chen TH (2004) Postoperative spinal deep wound infection: a six-year review of 3230 selective procedures. J Chin Med Assoc 67:398–402
Abt NB, De la Garza-Ramos R, Olorundare IO, McCutcheon BA, Bydon A, Fogelson J, Nassr A, Bydon M (2016) Thirty day postoperative outcomes following anterior lumbar interbody fusion using the National Surgical Quality Improvement Program database. Clin Neurol Neurosurg 143:126–131. doi:10.1016/j.clineuro.2016.02.024
Kang DG, Holekamp TF, Wagner SC, Lehman RJ (2015) Intrasite vancomycin powder for the prevention of surgical site infection in spine surgery: a systematic literature review. Spine J 15:762–770. doi:10.1016/j.spinee.2015.01.030
Tian NF, Wu YS, Zhang XL, Wu XL, Chi YL, Mao FM (2013) Fusion versus nonfusion for surgically treated thoracolumbar burst fractures: a meta-analysis. PLoS One 8:e63995. doi:10.1371/journal.pone.0063995
Acknowledgments
The authors would like to thank Professor Yong Hai and Xiang-Yao Sun who provided data support and corrected some mistakes.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Funding
There is no funding source.
Ethical approval
This article does not contain any studies with human participants or animals performed by any of the authors.
Informed consent
Informed consent was obtained from all researches included in the study.
Rights and permissions
About this article
Cite this article
Sun, XY., Zhang, XN. & Hai, Y. Percutaneous versus traditional and paraspinal posterior open approaches for treatment of thoracolumbar fractures without neurologic deficit: a meta-analysis. Eur Spine J 26, 1418–1431 (2017). https://doi.org/10.1007/s00586-016-4818-4
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00586-016-4818-4