Abstract
Introduction
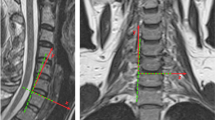
We investigated a new metric for assessing the quality of motion of the cervical segments over the arc of extension-to-flexion motion after cervical disc arthroplasty (CDA). We quantified: (1) the amount of motion contributed by individual spinal segments to the total cervical spine motion, termed segmental motion fraction, and its variation throughout the arc of extension-to-flexion motion and (2) how cervical disc arthroplasty using two distinct prosthesis designs may influence the segmental motion contributions.
Materials and methods
We tested 16 human C3–T1 spine specimens under physiologic loads; first intact, after CDA at C5–C6, and then at C5–C6 and C6–C7. The M6-C (Orthofix, USA) and Mobi-C (Zimmer, USA) disc prostheses were used in eight specimens each.
Results and conclusions
The designs of the cervical disc prostheses tested significantly influenced the variation in segmental motion fraction as the spine underwent motion between the endpoints of extension and flexion. While the mean segmental motion contribution to the total cervical motion was not influenced by prosthesis design, the way the motion took place between the extension and flexion endpoints was significantly influenced. The M6-C artificial disc restored physiologic motion quality such that implanted segments continued to function in harmony with other segments of the cervical spine as measured before arthroplasty. Conversely, the Mobi-C prosthesis, while maintaining average motion contributions similar to the pre-implantation values, demonstrated large deviations in motion contribution over the extension-to-flexion arc motion in ten of 16 implanted segments. Such non-physiologic implant kinematics could cause excessive prosthesis wear and motion and stress shielding at adjacent segments.
Graphical abstract
These slides can be retrieved under Electronic Supplementary Material.








Similar content being viewed by others
Change history
22 February 2021
A Correction to this paper has been published: https://doi.org/10.1007/s00586-020-06569-3
References
Sasso R, Anderson P, Riew K et al (2011) Results of cervical arthroplasty compared with anterior discectomy and fusion: four-year clinical outcomes in a prospective, randomized, controlled trial. J Bone Joint Surg Am 93:1684–1692
Coric D, Nunley PD, Guyer RD, Musante D, Carmody CN, Gordon CR et al (2011) Prospective, randomized, multicenter study of cervical arthroplasty: 269 patients from the Kineflex C artificial disc investigational device exemption study with a minimum 2-year follow-up. J Neurosurg Spine 15(4):348–358
Zigler JE, Delamarter R, Murrey D, Spivak J, Janssen M (2013) ProDisc-C and anterior cervical discectomy and fusion as surgical treatment for single-level cervical symptomatic degenerative disc disease: five-year results of a Food and Drug Administration study. Spine 38(3):203–209
Davis RJ, Kim KD, Hisey MS, Hoffman GA, Bae HW, Gaede SE et al (2013) Cervical total disc replacement with the Mobi-C cervical artificial disc compared with anterior discectomy and fusion for treatment of 2-level symptomatic degenerative disc disease: a prospective, randomized, controlled multicenter clinical trial. J Neurosurg Spine 19(5):532–545
Gornet MF, Burkus JK, Shaffrey ME, Argires PJ, Nian H, Harrell FE (2015) Cervical disc arthroplasty with PRESTIGE LP disc versus anterior cervical discectomy and fusion: a prospective, multicenter investigational device exemption study. J Neurosurg Spine 23(5):558–573
Hisey MS, Zigler JE, Jackson R, Nunley PD, Bae HW, Kim KD, Ohnmeiss DD (2016) Prospective, randomized comparison of one-level Mobi-C cervical total disc replacement vs. anterior cervical discectomy and fusion: results at 5-year follow-up. Int J Spine Surg 10:10
Hipp JA, Wharton ND (2008) Quantitative motion analysis (QMA) of motion-preserving and fusion technologies for the spine. In: Motion preservation surgery of the spine. Philadeplhia, Saunders, pp 85–96
Puttlitz CM, Rousseau MA, Xu Z, Hu S, Tay BK, Lotz JC (2004) Intervertebral disc replacement maintains cervical spine kinetics. Spine (Phila Pa 1976) 29:2809–2814
Patwardhan AG, Voronov L, Havey RM, Tzermiadianos M, Carandang G, McIntosh B et al (2009) P152. Limited restoration of primary and coupled motions in lateral bending and axial rotation after total disc replacement: a common finding in cervical disc prostheses. Spine J 9(10):192S–193S (Abstract)
Finn MA, Brodke DS, Daubs M, Patel A, Bachus KN (2009) Local and global subaxial cervical spine biomechanics after single-level fusion or cervical arthroplasty. Eur Spine J 18:1520–1527. https://doi.org/10.1007/s00586-009-1085-7
Patwardhan AG, Tzermiadianos MN, Tsitsopoulos PP, Voronov LI, Renner SM, Reo ML et al (2012) Primary and coupled motions after cervical total disc replacement using a compressible six-degree-of-freedom prosthesis. Eur Spine J 21(5):618–629
Lee MJ, Dumonski M, Phillips FM, Voronov LI, Renner SM, Carandang G et al (2011) Disc replacement adjacent to cervical fusion: a biomechanical comparison of hybrid construct versus two-level fusion. Spine 36(23):1932–1939
Martin S, Ghanayem AJ, Tzermiadianos MN, Voronov LI, Havey RM, Renner SM et al (2011) Kinematics of cervical total disc replacement adjacent to a two-level, straight versus lordotic fusion. Spine 36(17):1359–1366
Havey RM, Khayatzadeh S, Voronov LI, Blank KR, Carandang G, Harding DP, Patwardhan AG (2019) Motion response of a polycrystalline diamond adaptive axis of rotation cervical total disc arthroplasty. Clin Biomech 62:34–41
Anderst WJ, Donaldson WF III, Lee JY, Kang JD (2013) Cervical motion segment percent contributions to flexion-extension during continuous functional movement in control subjects and arthrodesis patients. Spine 38(9):E533
Patwardhan AG, Havey RM, Ghanayem AJ, Diener H, Meade KP, Dunlap B, Hodges SD (2000) Load carrying capacity of the human cervical spine in compression is increased under a follower load. Spine 25(12):1548–1554
Beaurain J, Bernard P, Dufour T, Fuentes JM, Hovorka I, Huppert J et al (2008) Mobi-C. Motion preservation surgery of the spine: advanced techniques and controversies (Part III), pp 231–237
Reyes-Sanchez A, Patwardhan AG, Block JE (2008) The M6 artificial cervical disc. Motion preservation surgery of the spine, Saunders Elsevier, Philadelphia
Panjabi MM (1992) The stabilizing system of the spine. Part II. Neutral zone and instability hypothesis. J Spinal Disord 5:390–396
Acknowledgements
This work was supported in part by research funding from the Department of Veterans Affairs and Chicago Association for Research and Education in Science, Hines, Illinois.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
AG. Patwardhan is a consultant to Orthofix Inc., Lewisville TX, USA. RM. Havey has no conflict of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Patwardhan, A.G., Havey, R.M. Prosthesis design influences segmental contribution to total cervical motion after cervical disc arthroplasty. Eur Spine J 29, 2713–2721 (2020). https://doi.org/10.1007/s00586-019-06064-4
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00586-019-06064-4