Abstract
Purpose
Anterior cervical discectomy and fusion (ACDF) is a common surgical treatment for degenerative disease in the cervical spine. However, resultant biomechanical alterations may predispose to early-onset adjacent segment degeneration (EO-ASD), which may become symptomatic and require reoperation. This study aimed to develop and validate a machine learning (ML) model to predict EO-ASD following ACDF.
Methods
Retrospective review of prospectively collected data of patients undergoing ACDF at a quaternary referral medical center was performed. Patients > 18 years of age with > 6 months of follow-up and complete pre- and postoperative X-ray and MRI imaging were included. An ML-based algorithm was developed to predict EO-ASD based on preoperative demographic, clinical, and radiographic parameters, and model performance was evaluated according to discrimination and overall performance.
Results
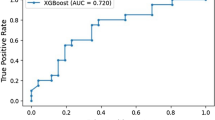
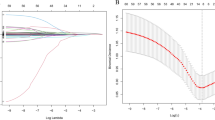
In total, 366 ACDF patients were included (50.8% male, mean age 51.4 ± 11.1 years). Over 18.7 ± 20.9 months of follow-up, 97 (26.5%) patients developed EO-ASD. The model demonstrated good discrimination and overall performance according to precision (EO-ASD: 0.70, non-ASD: 0.88), recall (EO-ASD: 0.73, non-ASD: 0.87), accuracy (0.82), F1-score (0.79), Brier score (0.203), and AUC (0.794), with C4/C5 posterior disc bulge, C4/C5 anterior disc bulge, C6 posterior superior osteophyte, presence of osteophytes, and C6/C7 anterior disc bulge identified as the most important predictive features.
Conclusions
Through an ML approach, the model identified risk factors and predicted development of EO-ASD following ACDF with good discrimination and overall performance. By addressing the shortcomings of traditional statistics, ML techniques can support discovery, clinical decision-making, and precision-based spine care.





Similar content being viewed by others
References
Samartzis D, Marco RA, Jenis LG, Khanna N, Banco RJ, Goldberg EJ, An HS (2007) Characterization of graft subsidence in anterior cervical discectomy and fusion with rigid anterior plate fixation. Am J Orthop (Belle Mead NJ) 36(8):421–427
Samartzis D, Shen FH, Goldberg EJ, An HS (2005) Is autograft the gold standard in achieving radiographic fusion in one-level anterior cervical discectomy and fusion with rigid anterior plate fixation? Spine (Phila Pa 1976) 30(15):1756–1761. https://doi.org/10.1097/01.brs.0000172148.86756.ce
Samartzis D, Shen FH, Lyon C, Phillips M, Goldberg EJ, An HS (2004) Does rigid instrumentation increase the fusion rate in one-level anterior cervical discectomy and fusion? Spine J 4(6):636–643. https://doi.org/10.1016/j.spinee.2004.04.010
Shen FH, Samartzis D, Khanna N, Goldberg EJ, An HS (2004) Comparison of clinical and radiographic outcome in instrumented anterior cervical discectomy and fusion with or without direct uncovertebral joint decompression. Spine J 4(6):629–635. https://doi.org/10.1016/j.spinee.2004.04.009
Samartzis D, Shen FH, Matthews DK, Yoon ST, Goldberg EJ, An HS (2003) Comparison of allograft to autograft in multilevel anterior cervical discectomy and fusion with rigid plate fixation. Spine J 3(6):451–459. https://doi.org/10.1016/s1529-9430(03)00173-6
Cloward RB (1958) The anterior approach for removal of ruptured cervical disks. J Neurosurg 15(6):602–617. https://doi.org/10.3171/jns.1958.15.6.0602
Smith GW, Robinson RA (1958) The treatment of certain cervical-spine disorders by anterior removal of the intervertebral disc and interbody fusion. J Bone Jt Surg Am 40(3):607–624. https://doi.org/10.2106/00004623-195840030-00009
Hong L, Kawaguchi Y (2011) Anterior cervical discectomy and fusion to treat cervical spondylosis with sympathetic symptoms. J Spinal Disord Tech 24(1):11–14. https://doi.org/10.1097/BSD.0b013e3181dd80f5
Dean CL, Gabriel JP, Cassinelli EH, Bolesta MJ, Bohlman HH (2009) Degenerative spondylolisthesis of the cervical spine: analysis of 58 patients treated with anterior cervical decompression and fusion. Spine J 9(6):439–446. https://doi.org/10.1016/j.spinee.2008.11.010
Hilibrand AS, Carlson GD, Palumbo MA, Jones PK, Bohlman HH (1999) Radiculopathy and myelopathy at segments adjacent to the site of a previous anterior cervical arthrodesis. J Bone Jt Surg Am 81(4):519–528. https://doi.org/10.2106/00004623-199904000-00009
Hilibrand AS, Robbins M (2004) Adjacent segment degeneration and adjacent segment disease: the consequences of spinal fusion? Spine J 4(6):190S-194S. https://doi.org/10.1016/j.spinee.2004.07.007
Zigler JE, Rogers RW, Ohnmeiss DD (2016) Comparison of 1-level versus 2-level anterior cervical discectomy and fusion: clinical and radiographic follow-up at 60 months. Spine 41(6):463–469. https://doi.org/10.1097/BRS.0000000000001263
Wirth FP, Dowd GC, Sanders HF, Wirth C (2000) Cervical discectomy. Surg Neurol 53(4):340–348. https://doi.org/10.1016/S0090-3019(00)00201-9
Saavedra-Pozo FM, Deusdara RA, Benzel EC (2014) Adjacent segment disease perspective and review of the literature. Ochsner J 14(1):78–83
Wong AYL, Harada G, Lee R et al (2021) Preoperative paraspinal neck muscle characteristics predict early onset adjacent segment degeneration in anterior cervical fusion patients: a machine-learning modeling analysis. J Orthop Res 39(8):1732–1744. https://doi.org/10.1002/jor.24829
Burch MB, Wiegers NW, Patil S, Nourbakhsh A (2020) Incidence and risk factors of reoperation in patients with adjacent segment disease: a meta-analysis. J Craniovertebral Jun Spine 11(1):9–16. https://doi.org/10.4103/jcvjs.JCVJS_10_20
Harada GK, Alter K, Nguyen AQ et al (2020) Cervical spine endplate abnormalities and association with pain, disability, and adjacent segment degeneration after anterior cervical discectomy and fusion. Spine (Phila Pa 1976) 45(15):E917–E926. https://doi.org/10.1097/BRS.0000000000003460
Katz AD, Mancini N, Karukonda T, Cote M, Moss IL (2019) Comparative and predictor analysis of 30-day readmission, reoperation, and morbidity in patients undergoing multilevel ACDF versus single and multilevel ACCF using the ACS-NSQIP dataset. Spine (Phila Pa 1976) 44(23):E1379–E1387. https://doi.org/10.1097/BRS.0000000000003167
Phan K, Wang N, Kim JS et al (2017) Effect of preoperative anemia on the outcomes of anterior cervical discectomy and fusion. Glob Spine J 7(5):441–447. https://doi.org/10.1177/2192568217699404
Wu JC, Chang HK, Huang WC, Chen YC (2019) Risk factors of second surgery for adjacent segment disease following anterior cervical discectomy and fusion: a 16-year cohort study. Int J Surg 68:48–55. https://doi.org/10.1016/j.ijsu.2019.06.002
Wilson LA, Zubizarreta N, Bekeris J et al (2020) Risk factors for reintubation after anterior cervical discectomy and fusion surgery: evaluation of three observational data sets. Can J Anaesth 67(1):42–56. https://doi.org/10.1007/s12630-019-01492-8
Bovonratwet P, Fu MC, Tyagi V et al (2019) Incidence, risk factors, and clinical implications of postoperative hematoma requiring reoperation following anterior cervical discectomy and fusion. Spine (Phila Pa 1976) 44(8):543–549. https://doi.org/10.1097/BRS.0000000000002885
Galbusera F, Casaroli G, Bassani T (2019) Artificial intelligence and machine learning in spine research. JOR Spine 2(1):e1044. https://doi.org/10.1002/jsp2.1044
Harada GK, Siyaji ZK, Younis S, Louie PK, Samartzis D, An HS (2020) Imaging in spine surgery: current concepts and future directions. Spine Surg Relat Res 4(2):99–110. https://doi.org/10.22603/ssrr.2020-0011
Chang M, Canseco JA, Nicholson KJ, Patel N, Vaccaro AR (2020) The role of machine learning in spine surgery: the future is now. Front Surg 7:54. https://doi.org/10.3389/fsurg.2020.00054
Senders JT, Staples PC, Karhade AV et al (2018) Machine learning and neurosurgical outcome prediction: a systematic review. World Neurosurg 109(476–486):e471. https://doi.org/10.1016/j.wneu.2017.09.149
Karhade AV, Thio Q, Ogink P et al (2018) Development of machine learning algorithms for prediction of 5-year spinal chordoma survival. World Neurosurg 119:e842–e847. https://doi.org/10.1016/j.wneu.2018.07.276
Karhade AV, Thio Q, Ogink PT et al (2019) Predicting 90-day and 1-year mortality in spinal metastatic disease: development and internal validation. Neurosurgery 85(4):E671–E681. https://doi.org/10.1093/neuros/nyz070
Smith JS, Shaffrey CI, Bess S et al (2017) Recent and emerging advances in spinal deformity. Neurosurgery 80(3S):S70–S85. https://doi.org/10.1093/neuros/nyw048
Joshi RS, Haddad AF, Lau D, Ames CP (2019) Artificial intelligence for adult spinal deformity. Neurospine 16(4):686–694. https://doi.org/10.14245/ns.1938414.207
Samartzis D, Alini M, An HS et al (2018) Precision spine care: a new era of discovery, innovation, and global impact. Global Spine J 8(4):321–322. https://doi.org/10.1177/2192568218774044
Samartzis D, Borthakur A, Belfer I et al (2015) Novel diagnostic and prognostic methods for disc degeneration and low back pain. Spine J 15(9):1919–1932. https://doi.org/10.1016/j.spinee.2014.09.010
Harada GK, Siyaji ZK, Mallow GM et al (2021) Artificial intelligence predicts disk re-herniation following lumbar microdiscectomy: development of the “RAD” risk profile. Eur Spine J 30(8):2167–2175. https://doi.org/10.1007/s00586-021-06866-5
Mallow GM, Siyaji ZK, Galbusera F et al (2021) Intelligence-based spine care model: a new era of research and clinical decision-making. Glob Spine J 11(2):135–145. https://doi.org/10.1177/2192568220973984
Harada GK, Tao Y, Louie PK et al (2021) Cervical spine MRI phenotypes and prediction of pain, disability and adjacent segment degeneration/disease after ACDF. J Orthop Res 39(3):657–670. https://doi.org/10.1002/jor.24658
Alhashash M, Shousha M, Boehm H (2018) Adjacent segment disease after cervical spine fusion: evaluation of a 70 patient long-term follow-up. Spine (Phila Pa 1976) 43(9):605–609. https://doi.org/10.1097/BRS.0000000000002377
Ishihara H, Kanamori M, Kawaguchi Y, Nakamura H, Kimura T (2004) Adjacent segment disease after anterior cervical interbody fusion. Spine J 4(6):624–628. https://doi.org/10.1016/j.spinee.2004.04.011
Lawrence BD, Hilibrand AS, Brodt ED, Dettori JR, Brodke DS (2012) Predicting the risk of adjacent segment pathology in the cervical spine: a systematic review. Spine (Phila Pa 1976) 37:S52–S64. https://doi.org/10.1097/BRS.0b013e31826d60fb
Collins GS, Reitsma JB, Altman DG, Moons KG (2015) Transparent reporting of a multivariable prediction model for individual prognosis or diagnosis (TRIPOD): the TRIPOD statement. Br J Surg 102(3):148–158. https://doi.org/10.1002/bjs.9736
Luo W, Phung D, Tran T et al (2016) Guidelines for developing and reporting machine learning predictive models in biomedical research: a multidisciplinary view. J Med Internet Res 18(12):e323. https://doi.org/10.2196/jmir.5870
Basques BA, Louie PK, Mormol J et al (2018) Multi- versus single-level anterior cervical discectomy and fusion: comparing sagittal alignment, early adjacent segment degeneration, and clinical outcomes. Eur Spine J 27(11):2745–2753. https://doi.org/10.1007/s00586-018-5677-y
Kraemer P, Fehlings MG, Hashimoto R et al (2012) A systematic review of definitions and classification systems of adjacent segment pathology. Spine (Phila Pa 1976) 37:S31–S39. https://doi.org/10.1097/BRS.0b013e31826d7dd6
Hardt J, Herke M, Leonhart R (2012) Auxiliary variables in multiple imputation in regression with missing X: a warning against including too many in small sample research. BMC Med Res Methodol 12(1):1–13. https://doi.org/10.1186/1471-2288-12-184
Chen T, Guestrin C (2016) XGBoost: a scalable tree boosting system. In: Proceedings of the 22nd ACM SIGKDD international conference on knowledge discovery and data mining. pp 785–794
Pedregosa FV, Varoquaux G, Gramfort A, Michel V, Thirion B, Grisel O, Blondel M, Prettenhofer P, Weiss R, Dubourg V, Vanderplas J, Passos A, Cournapeau D, Brucher M, Perrot M, Duchesnay E (2011) Scikit-learn: machine learning in python. J Mach Learn Res 12:2825–2830
Chawla NV, Bowyer KW, Hall LO, Kegelmeyer WP (2002) SMOTE: synthetic minority over-sampling technique. J Artif Intell Res 16:321–357. https://doi.org/10.1613/jair.953
Lipton ZC, Elkan C (2014) Thresholding classifiers to maximize F1 score. http://arxiv.org/abs/1402.1892. Published 2014. Accessed
Bradley AP (1993) The use of the area under the roc curve in the evaluation of machine learning algorithms. Pattern Recogn 30(7):1145–1159
Hastie T, Tibshirani R, Friedman JH, Friedman JH (2009) The elements of statistical learning: data mining, inference, and prediction. Springer Science & Business Media, New York
Komura S, Miyamoto K, Hosoe H, Iinuma N, Shimizu K (2012) Lower incidence of adjacent segment Degeneration after anterior cervical fusion found with those fusing C5–6 and C6–7 than those leaving C5–6 or C6–7 as an adjacent level. J Spinal Disord Tech 25(1):23–29. https://doi.org/10.1097/BSD.0b013e31820bb1f8
Katsuura A, Hukuda S, Saruhashi Y, Mori K (2001) Kyphotic malalignment after anterior cervical fusion is one of the factors promoting the degenerative process in adjacent intervertebral levels. Eur Spine J 10(4):320–324. https://doi.org/10.1007/s005860000243
Matsumoto M, Okada E, Ichihara D et al (2010) Anterior cervical decompression and fusion accelerates adjacent segment degeneration: comparison with asymptomatic volunteers in a ten-year magnetic resonance imaging follow-up study. Spine (Phila Pa 1976) 35(1):36–43. https://doi.org/10.1097/BRS.0b013e3181b8a80d
Battié MC, Videman T, Parent E (2004) Lumbar disc degeneration: epidemiology and genetic influences. Spine (Phila Pa 1976) 29(23):2679–2690. https://doi.org/10.1097/01.brs.0000146457.83240.eb
Battie MC, Videman T, Kaprio J et al (2009) The twin spine study: contributions to a changing view of disc degeneration. Spine J 9(1):47–59. https://doi.org/10.1016/j.spinee.2008.11.011
Battie MC, Videman T, Levalahti E, Gill K, Kaprio J (2007) Heritability of low back pain and the role of disc degeneration. Pain 131(3):272–280. https://doi.org/10.1016/j.pain.2007.01.010
Battié MC, Videman T, Levälahti E, Gill K, Kaprio J (2008) Genetic and environmental effects on disc degeneration by phenotype and spinal level: a multivariate twin study. Spine (Phila Pa 1976) 33(25):2801–2808. https://doi.org/10.1097/BRS.0b013e31818043b7
Videman T, Battié MC, Parent E, Gibbons LE, Vainio P, Kaprio J (2008) Progression and determinants of quantitative magnetic resonance imaging measures of lumbar disc degeneration: a five-year follow-up of adult male monozygotic twins. Spine (Phila Pa 1976) 33(13):1484–1490. https://doi.org/10.1097/BRS.0b013e3181753bb1
Williams FM, Sambrook PN (2011) Neck and back pain and intervertebral disc degeneration: role of occupational factors. Best Pract Res Clin Rheumatol 25(1):69–79. https://doi.org/10.1016/j.berh.2011.01.007
COVENTRY MB (1970) Calcification in a cervical disc with anterior protrusion and dysphagia: a case report. J Bone Jt Surg Am 52(7):1463–1466
Picus D, McClennan BL, Balfe DM, Roper CL, Berrigan T (1984) “Discphagia”: a case report. Gastrointest Radiol 9(1):5–7. https://doi.org/10.1007/BF01887791
Bernardo KL, Grubb RL, Coxe WS, Roper CL (1988) Anterior cervical disc herniation. Case report. J Neurosurg 69(1):134–136. https://doi.org/10.3171/jns.1988.69.1.0134
Andersen PM, Fagerlund M (2000) Vertebrogenic dysphagia and gait disturbance mimicking motor neuron disease. J Neurol Neurosurg Psychiatry 69(4):560–561. https://doi.org/10.1136/jnnp.69.4.560
Lipson SJ, Muir H (1980) Vertebral osteophyte formation in experimental disc degeneration. Arthritis Rheum 23(3):319–324. https://doi.org/10.1002/art.1780230309
Rao RD, Gore DR, Tang SJ, Rebholz BJ, Yoganandan N, Wang M (2016) Radiographic Changes in the Cervical Spine Following Anterior Arthrodesis: A Long-Term Analysis of 166 Patients. J Bone Jt Surg Am 98(19):1606–1613. https://doi.org/10.2106/JBJS.15.01061
Gore DR, Sepic SB, Gardner GM, Murray MP (1987) Neck pain: a long-term follow-up of 205 patients. Spine (Phila Pa 1976) 12(1):1–5. https://doi.org/10.1097/00007632-198701000-00001
Okada E, Matsumoto M, Ichihara D et al (2009) Aging of the cervical spine in healthy volunteers: a 10-year longitudinal magnetic resonance imaging study. Spine (Phila Pa 1976) 34(7):706–712. https://doi.org/10.1097/BRS.0b013e31819c2003
Wong SH, Chiu KY, Yan CH (2016) Review article: osteophytes. J Orthop Surg (Hong Kong) 24(3):403–410. https://doi.org/10.1177/1602400327
Lundine KM, Davis G, Rogers M, Staples M, Quan G (2014) Prevalence of adjacent segment disc degeneration in patients undergoing anterior cervical discectomy and fusion based on pre-operative MRI findings. J Clin Neurosci 21(1):82–85. https://doi.org/10.1016/j.jocn.2013.02.039
Park JY, Kim KH, Kuh SU, Chin DK, Kim KS, Cho YE (2013) What are the associative factors of adjacent segment degeneration after anterior cervical spine surgery? Comparative study between anterior cervical fusion and arthroplasty with 5-year follow-up MRI and CT. Eur Spine J 22(5):1078–1089. https://doi.org/10.1007/s00586-012-2613-4
Rao RD, Wang M, McGrady LM, Perlewitz TJ, David KS (2005) Does anterior plating of the cervical spine predispose to adjacent segment changes? Spine (Phila Pa 1976) 30(24):2788–2792. https://doi.org/10.1097/01.brs.0000190453.46472.08
Cheng JS, Liu F, Komistek RD, Mahfouz MR, Sharma A, Glaser D (2007) Comparison of cervical spine kinematics using a fluoroscopic model for adjacent segment degeneration: invited submission from the joint section on disorders of the Spine and Peripheral Nerves, March 2007. J Neurosurg Spine 7(5):509–513. https://doi.org/10.3171/SPI-07/11/509
Eck JC, Humphreys SC, Lim TH et al (2002) Biomechanical study on the effect of cervical spine fusion on adjacent-level intradiscal pressure and segmental motion. Spine (Phila Pa 1976) 27(22):2431–2434. https://doi.org/10.1097/00007632-200211150-00003
van Eck CF, Regan C, Donaldson WF, Kang JD, Lee JY (2014) The revision rate and occurrence of adjacent segment disease after anterior cervical discectomy and fusion: a study of 672 consecutive patients. Spine (Phila Pa 1976) 39(26):2143–2147. https://doi.org/10.1097/BRS.0000000000000636
Yu C, Mu X, Wei J, Chu Y, Liang B (2016) In-depth analysis on influencing factors of adjacent segment degeneration after cervical fusion. Med Sci Monit 22:4902–4910. https://doi.org/10.12659/msm.902179
Loumeau TP, Darden BV, Kesman TJ et al (2016) A RCT comparing 7-year clinical outcomes of one level symptomatic cervical disc disease (SCDD) following ProDisc-C total disc arthroplasty (TDA) versus anterior cervical discectomy and fusion (ACDF). Eur Spine J 25(7):2263–2270. https://doi.org/10.1007/s00586-016-4431-6
Muheremu A, Niu X, Wu Z, Muhanmode Y, Tian W (2015) Comparison of the short- and long-term treatment effect of cervical disk replacement and anterior cervical disk fusion: a meta-analysis. Eur J Orthop Surg Traumatol 25(Suppl 1):S87-100. https://doi.org/10.1007/s00590-014-1469-1
Nabhan A, Steudel WI, Nabhan A, Pape D, Ishak B (2007) Segmental kinematics and adjacent level degeneration following disc replacement versus fusion: RCT with three years of follow-up. J Long Term Eff Med Implants 17(3):229–236. https://doi.org/10.1615/jlongtermeffmedimplants.v17.i3.60
Acknowledgements
The authors wish to thank Zakariah Siyaji and Remi Lee for their insights toward this topic.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors have no conflicts of interest to disclose.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Rudisill, S.S., Hornung, A.L., Barajas, J.N. et al. Artificial intelligence in predicting early-onset adjacent segment degeneration following anterior cervical discectomy and fusion. Eur Spine J 31, 2104–2114 (2022). https://doi.org/10.1007/s00586-022-07238-3
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00586-022-07238-3