Abstract
Background
The objective of this study was to correlate various radiological parameters with clinical outcome in patients who had undergone lumbar total disc replacement (TDR). Lumbar TDR is one possible treatment option in patients with low back pain (LBP), offering an alternative to lumbar fusion. Favourable clinical outcome hinges on a number of radiological parameters, such as mobility, sintering, and—most importantly—accurate positioning of the implant.
Methods
A total of 46 patients received a prosthetic disc because of degenerative lumbar disc disorders. Follow-up evaluation included analysis of radiographs and subjective rating of the clinical status by the patient using the North American Spine Society (NASS) patient questionnaire, visual analogue scale (VAS) for pain and state of health, and the EuroQol EQ-5D. Radiological follow-up took place after 2 years. Coronal and sagittal positions of the prosthesis, intervertebral disc height, facet joint pressure, mobility, sintering, and calcification were evaluated. Optimal positioning of the prosthesis was defined as a central coronal position and a most dorsal position in the sagittal plane. Based on the radiologically determined placement of the prosthesis, the patient population was divided into three groups, i.e., prosthesis ideally placed (<2 mm), discretely shifted (2–3 mm), or suboptimally placed (>3 mm).
Results
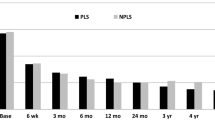
Overall, 81 % of patients stated that they would undergo the operation again. Health status was stable at a VAS score of 7.04 points 2 years after TDR, compared to 3.97 points before TDR. Mean working capacity had increased from 53 % preoperatively to 88 % 2 years after TDR. Overall, 39 % of the prostheses were rated as ideally positioned, while 13 % were discretely shifted and 48 % were suboptimally placed with respect to one of the radiological criteria. In 80.4 % of patients, follow-up assessment after ≥2 years indicated good mobility at the operated segment, while calcification was noted in 4 % and sintering was detected in 15 % of the implants.
Conclusions
Our data indicate poor correlation between clinical outcome and position of the prosthesis. Although 48 % of the implants were suboptimally placed in either the coronal or sagittal plane, most of the patients reached a very good clinical outcome. However, suboptimally placed devices appeared to cause significantly more neurological symptoms in long-term follow-up.






Similar content being viewed by others
References
Bertagnoli R, Kumar S (2002) Indications for full prosthetic disc arthroplasty: a correlation of clinical outcome against a variety ofindications. Eur Spine J 11(Suppl 2):S131–S136
Boss O, Bäurle B, Sgier F, Hausmann O (2011) Lumbar total disc replacement: correlation of clinical outcome and radiological parameters. Eur Spine J 20:2054
Brodsky AE (1976) Post-laminectomy and post-fusion stenosis of the lumbar spine. Clin Orthop Relat Res 130–139
Cassidy JD, Carroll LJ, Cote P (1998) The Saskatchewan health and back pain survey. The prevalence of low back pain and related disability in Saskatchewan adults. Spine (Phila Pa 1976) 23:1860–1866, discussion 1867
Cunningham BW, Dmitriev AE, Hu N, McAfee PC (2003) General principles of total disc replacement arthroplasty: seventeen cases in a nonhuman primate model. Spine (Phila Pa 1976) 28:S118–S124
Daltroy LH, Cats-Baril WL, Katz JN, Fossel AH, Liang MH (1996) The North American spine society lumbar spine outcome assessment instrument: reliability and validity tests. Spine (Phila Pa 1976) 21:741–749
Deyo RA, Tsui-Wu YJ (1987) Descriptive epidemiology of low-back pain and its related medical care in the United States. Spine (Phila Pa 1976) 12:264–268
Gould D, Kelly D, Goldstone L, Gammon J (2001) Examining the validity of pressure ulcer risk assessment scales: developing and using illustrated patient simulations to collect the data. J Clin Nurs 10:697–706
Guyer RD, McAfee PC, Hochschuler SH, Blumenthal SL, Fedder IL, Ohnmeiss DD, Cunningham BW (2004) Prospective randomized study of the Charite artificial disc: data from two investigational centers. Spine J 4:252S–259S
Harris RI, Wiley JJ (1963) Acquired spondylolysis as a sequel to spine fusion. J Bone Joint Surg Am 45:1159–1170
Harrop JS, Youssef JA, Maltenfort M, Vorwald P, Jabbour P, Bono CM, Goldfarb N, Vaccaro AR, Hilibrand AS (2008) Lumbar adjacent segment degeneration and disease after arthrodesis and total disc arthroplasty. Spine (Phila Pa 1976) 33:1701–1707
Kotsenas AL (2012) Imaging of posterior element axial pain generators facet joints, pedicles, spinous processes, sacroiliac joints, and transitional segments. Radiol Clin N Am 50:705–730
Le Huec JC, Mathews H, Basso Y, Aunoble S, Hoste D, Bley B, Friesem T (2005) Clinical results of Maverick lumbar total disc replacement: two-year prospective follow-up. Orthop Clin N Am 36:315–322
Lee CK (1988) Accelerated degeneration of the segment adjacent to a lumbar fusion. Spine (Phila Pa 1976) 13:375–377
Lemaire JP, Carrier H, el Sariali H, Skalli W, Lavaste F (2005) Clinical and radiological outcomes with the Charite artificial disc: a 10-year minimum follow-up. J Spinal Disord Tech 18:353–359
Link HD (2002) History, design and biomechanics of the LINK SB Charite artificial disc. Eur Spine J 11(Suppl 2):S98–S105
Mathews HH, Lehuec JC, Friesem T, Zdeblick T, Eisermann L (2004) Design rationale and biomechanics of Maverick Total Disc arthroplasty with early clinical results. Spine J 4:268S–275S
McAfee PC, Cunningham B, Holsapple G, Adams K, Blumenthal S, Guyer RD, Dmietriev A, Maxwell JH, Regan JJ, Isaza J (2005) A prospective, randomized, multicenter Food and Drug Administration investigational device exemption study of lumbar total disc replacement with the CHARITE artificial disc versus lumbar fusion: part II: evaluation of radiographic outcomes and correlation of surgical technique accuracy with clinical outcomes. Spine (Phila Pa 1976) 30:1576–1583, discussion E1388–1590
McAfee PC, Fedder IL, Saiedy S, Shucosky EM, Cunningham BW (2003) SB Charite disc replacement: report of 60 prospective randomized cases in a US center. J Spinal Disord Tech 16:424–433
Pose B, Sangha O, Peters A, Wildner M (1999) Validation of the North American Spine Society Instrument for assessment of health status in patients with chronic backache. Z Orthop Ihre Grenzgeb 137:437–441
Putzier M, Funk JF, Schneider SV, Gross C, Tohtz SW, Khodadadyan-Klostermann C, Perka C, Kandziora F (2006) Charite total disc replacement—clinical and radiographical results after an average follow-up of 17 years. Eur Spine J 15:183–195
Quirno M, Goldstein J, Bendo J, Yong K, Spivak J (2011) The incidence of potential candidates for total disc replacement among lumbar and cervical fusion patient populations. Asian Spine J 5(4):213–219
Sangha O, Wildner M, Peters A (2000) Evaluation of the North American Spine Society Instrument for assessment of health status in patients with chronic backache. Z Orthop Ihre Grenzgeb 138:447–451
Schluessmann E, Diel P, Aghayev E, Zweig T, Moulin P, Röder C (2009) SWISSspine: a nationwide registry for health technology assessment of lumbar disc prostheses. Eur Spine J 18:851–861
Schmidt R, Obertacke U, Nothwang J, Ulrich C, Nowicki J, Reichel H, Cakir B (2010) The impact of implantation technique on frontal and sagittal alignment in total lumbar disc replacement: a comparison of anterior versus oblique implantation. Eur Spine J 19:1534–1539
Siepe CJ, Mayer HM, Wiechert K, Korge A (2006) Clinical results of total lumbar disc replacement with ProDisc II: three-year results for different indications. Spine (Phila Pa 1976) 31:1923–1932
Tournier C, Aunoble S, Le Huec JC, Lemaire JP, Tropiano P, Lafage V, Skalli W (2007) Total disc arthroplasty: consequences for sagittal balance and lumbar spine movement. Eur Spine J 16:411–421
Yajun W, Yue Z, Xiuxin H, Cui C (2010) A meta-analysis of artificial total disc replacement versus fusion for lumbar degenerative disc disease. Eur Spine J 19:1250–1261
Zigler JE, Burd TA, Vialle EN, Sachs BL, Rashbaum RF, Ohnmeiss DD (2003) Lumbar spine arthroplasty: early results using the ProDisc II: a prospective randomized trial of arthroplasty versus fusion. J Spinal Disord Tech 16:352–361
Conflicts of interest
None.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Boss, O.L., Tomasi, S.O., Bäurle, B. et al. Lumbar total disc replacement: correlation of clinical outcome and radiological parameters. Acta Neurochir 155, 1923–1930 (2013). https://doi.org/10.1007/s00701-013-1774-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00701-013-1774-1