Abstract
Purpose
In an effort to control postoperative pain more effectively in spinal fusion patients, intraoperative intrathecal morphine (ITM) administration is gaining popularity and acceptance with clinicians. This study seeks to determine the impact of intraoperative intrathecal opioid (ITO) administration following lumbar fusion surgery on postoperative pain and length of hospitalization as primary outcomes. Secondary outcomes will investigate postoperative opioid intake and side effects.
Methods
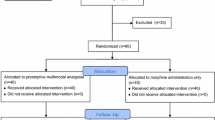
The retrospective analysis of collected data was performed. The study compared patients undergoing one- or two-level transforaminal interbody fusions between 2019 and 2021 who intraoperatively received two different ITO doses (n = 89) vs. the reference group (n = 48) that did not receive ITO. The patients in the ITO group received either 0.2 mg (n = 44) of duramorph or 0.2 mg duramorph + 50 mcg fentanyl (n = 45). The effect of ITO was evaluated for the first four postoperative days (POD) on pain scores (visual analog scale), length of stay (LOS, hours) and opioid requirement (MED, morphine equivalent dose).
Results
In the ITO group, a significant reduction of postoperative pain scores (t(99) = 4.3, p < 0.001) and opioid intake (t(70) = 2.49, p = 0.015) was noted on POD1. Cohen’s d effect sizes were 0.76 and 0.50, meaning that postoperative pain and MED intake were reduced by about ¾ to ½ standard deviations (SD) in the ITO group. Further, multivariate regression models revealed that ITO administration predicted lower postoperative pain scores for the two PODs (β = − 0.83, p < 0.001; β = − 0.63, p = 0.022) and MED intake for the first two PODs (β = − 20.8, p = 0.047; β = − 16.4, p = 0.030). Mean LOS was 15.4 h less in the ITO group (mean ± SD, 63.4 ± 37.1 vs. 78.8 ± 39.6, p = 0.10).
Conclusions
In conclusion, our study provides results in a large sample of patients undergoing transforaminal lumbar fusions. The results demonstrated that ITO administration is effective in reducing POD1 pain scores and POD1–2 opioid requirement while not increasing the risk of any opioid-related side effects.


Similar content being viewed by others
References
AraimoMorselli FSM, Zuccarini F, Caporlingua F, Scarpa I, Imperiale C, Caporlingua A, De Biase L, Tordiglione P (2017) Intrathecal versus intravenous morphine in minimally invasive posterior lumbar fusion: a blinded randomized comparative prospective study. Spine (Phila Pa 1976) 42:281–284. https://doi.org/10.1097/BRS.0000000000001733
Blacklock JB, Rea GL, Maxwell RE (1986) Intrathecal morphine during lumbar spine operation for postoperative pain control. Neurosurgery 18:341–344. https://doi.org/10.1227/00006123-198603000-00015
Boezaart AP, Eksteen JA, Spuy GV, Rossouw P, Knipe M (1999) Intrathecal morphine. Double-blind evaluation of optimal dosage for analgesia after major lumbar spinal surgery. Spine (Phila Pa 1976) 24:1131–1137. https://doi.org/10.1097/00007632-199906010-00013
Carr DB, Goudas LC (1999) Acute pain. Lancet 353:2051–2058. https://doi.org/10.1016/S0140-6736(99)03313-9
Chan JH, Heilpern GN, Packham I, Trehan RK, Marsh GD, Knibb AA (2006) A prospective randomized double-blind trial of the use of intrathecal fentanyl in patients undergoing lumbar spinal surgery. Spine (Phila Pa 1976) 31:2529–2533. https://doi.org/10.1097/01.brs.0000241135.79983.52
Cousins MJ, Mather LE, Glynn CJ, Wilson PR, Graham JR (1979) Selective spinal analgesia. Lancet 1:1141–1142. https://doi.org/10.1016/s0140-6736(79)91817-8
De Bie A, Siboni R, Smati MF, Ohl X, Bredin S (2020) Intrathecal morphine injections in lumbar fusion surgery: case-control study. Orthop Traumatol Surg Res 106:1187–1190. https://doi.org/10.1016/j.otsr.2020.02.024
Dhaliwal P, Yavin D, Whittaker T, Hawboldt GS, Jewett GAE, Casha S, du Plessis S (2019) Intrathecal morphine following lumbar fusion: a randomized, placebo-controlled trial. Neurosurgery 85:189–198. https://doi.org/10.1093/neuros/nyy384
Firouzian A, Gholipour Baradari A, Ehteshami S, Zamani Kiasari A, Shafizad M, Shafiei S, Younesi Rostami F, Alipour A, Ala S, Darvishi-Khezri H, Haddadi K (2020) The effect of ultra-low-dose intrathecal naloxone on pain intensity after lumbar laminectomy with spinal fusion: a randomized controlled trial. J Neurosurg Anesthesiol 32:70–76. https://doi.org/10.1097/ANA.0000000000000537
Fitzpatrick GJ, Moriarty DC (1988) Intrathecal morphine in the management of pain following cardiac surgery. A comparison with morphine i.v. Br J Anaesth 60:639–644. https://doi.org/10.1093/bja/60.6.639
France JC, Jorgenson SS, Lowe TG, Dwyer AP (1997) The use of intrathecal morphine for analgesia after posterolateral lumbar fusion: a prospective, double-blind, randomized study. Spine (Phila Pa 1976) 22:2272–2277. https://doi.org/10.1097/00007632-199710010-00015
Gan TJ, Habib AS, Miller TE, White W, Apfelbaum JL (2014) Incidence, patient satisfaction, and perceptions of post-surgical pain: results from a US national survey. Curr Med Res Opin 30:149–160. https://doi.org/10.1185/03007995.2013.860019
Ganesh A, Kim A, Casale P, Cucchiaro G (2007) Low-dose intrathecal morphine for postoperative analgesia in children. Anesth Analg 104:271–276. https://doi.org/10.1213/01.ane.0000252418.05394.28
Giovannelli M, Bedforth N, Aitkenhead A (2008) Survey of intrathecal opioid usage in the UK. Eur J Anaesthesiol 25:118–122. https://doi.org/10.1017/S0265021507001305
Glare P, Aubrey KR, Myles PS (2019) Transition from acute to chronic pain after surgery. Lancet 393:1537–1546. https://doi.org/10.1016/S0140-6736(19)30352-6
Gwirtz KH, Young JV, Byers RS, Alley C, Levin K, Walker SG, Stoelting RK (1999) The safety and efficacy of intrathecal opioid analgesia for acute postoperative pain: seven years’ experience with 5969 surgical patients at Indiana University Hospital. Anesth Analg 88:599–604. https://doi.org/10.1097/00000539-199903000-00026
Hong RA, Gibbons KM, Li GY, Holman A, Voepel-Lewis T (2017) A retrospective comparison of intrathecal morphine and epidural hydromorphone for analgesia following posterior spinal fusion in adolescents with idiopathic scoliosis. Paediatr Anaesth 27:91–97. https://doi.org/10.1111/pan.13037
Ko S, Goldstein DH, VanDenKerkhof EG (2003) Definitions of “respiratory depression” with intrathecal morphine postoperative analgesia: a review of the literature. Can J Anaesth 50:679–688. https://doi.org/10.1007/BF03018710
Koning MV, Teunissen AJW, van der Harst E, Ruijgrok EJ, Stolker RJ (2018) Intrathecal morphine for laparoscopic segmental colonic resection as part of an enhanced recovery protocol: a randomized controlled trial. Reg Anesth Pain Med 43:166–173. https://doi.org/10.1097/AAP.0000000000000703
Lauretti GR, Righeti CC, Mattos AL (2013) Intrathecal ketorolac enhances intrathecal morphine analgesia following total knee arthroplasty. J Anaesthesiol Clin Pharmacol 29:503–508. https://doi.org/10.4103/0970-9185.119155
Li Y, Swallow J, Robbins C, Caird MS, Leis A, Hong RA (2021) Gabapentin and intrathecal morphine combination therapy results in decreased oral narcotic use and more consistent pain scores after posterior spinal fusion for adolescent idiopathic scoliosis. J Orthop Surg Res 16:672. https://doi.org/10.1186/s13018-021-02525-z
McGreevy K, Bottros MM, Raja SN (2011) Preventing chronic pain following acute pain: risk factors, preventive strategies, and their efficacy. Eur J Pain Suppl 5:365–372. https://doi.org/10.1016/j.eujps.2011.08.013
O’Neill P, Knickenberg C, Bogahalanda S, Booth AE (1985) Use of intrathecal morphine for postoperative pain relief following lumbar spine surgery. J Neurosurg 63:413–416. https://doi.org/10.3171/jns.1985.63.3.0413
Pendi A, Acosta FL, Tuchman A, Movahedi R, Sivasundaram L, Arif I, Gucev G (2017) Intrathecal morphine in spine surgery: a meta-analysis of randomized controlled trials. Spine (Phila Pa 1976) 42:E740–E747. https://doi.org/10.1097/BRS.0000000000002198
Rodanant O, Sirichotewithayakorn P, Sriprajittichai P, Charuluxananan S (2003) An optimal dose study of intrathecal morphine in gynecological patients. J Med Assoc Thai 86(Suppl 2):S331-337
Ross DA, Drasner K, Weinstein PR, Flaherty JF, Barbaro NM (1991) Use of intrathecally administered morphine in the treatment of postoperative pain after lumbar spinal surgery: a prospective, double-blind, placebo-controlled study. Neurosurgery 28:700–704. https://doi.org/10.1097/00006123-199105000-00010
Sun J, Chen SR, Pan HL (2020) μ-Opioid receptors in primary sensory neurons are involved in supraspinal opioid analgesia. Brain Res 1729:146623. https://doi.org/10.1016/j.brainres.2019.146623
Techanivate A, Kiatgungwanglia P, Yingsakmongkol W (2003) Spinal morphine for post-operative analgesia after lumbar laminectomy with fusion. J Med Assoc Thai 86:262–269
Urban MK, Jules-Elysee K, Urquhart B, Cammisa FP, Boachie-Adjei O (2002) Reduction in postoperative pain after spinal fusion with instrumentation using intrathecal morphine. Spine (Phila Pa 1976) 27:535–537. https://doi.org/10.1097/00007632-200203010-00015
Wang JK, Nauss LA, Thomas JE (1979) Pain relief by intrathecally applied morphine in man. Anesthesiology 50:149–151. https://doi.org/10.1097/00000542-197902000-00013
Yaksh TL, Rudy TA (1976) Analgesia mediated by a direct spinal action of narcotics. Science 192:1357–1358. https://doi.org/10.1126/science.1273597
Yen D, Turner K, Mark D (2015) Is a single low dose of intrathecal morphine a useful adjunct to patient-controlled analgesia for postoperative pain control following lumbar spine surgery? A preliminary report. Pain Res Manag 20:129–132. https://doi.org/10.1155/2015/761390
Yörükoğlu D, Ateş Y, Temiz H, Yamali H, Kecik Y (2005) Comparison of low-dose intrathecal and epidural morphine and bupivacaine infiltration for postoperative pain control after surgery for lumbar disc disease. J Neurosurg Anesthesiol 17:129–133. https://doi.org/10.1097/01.ana.0000167146.13415.7c
Ziegeler S, Fritsch E, Bauer C, Mencke T, Müller BI, Soltesz S, Silomon M (2008) Therapeutic effect of intrathecal morphine after posterior lumbar interbody fusion surgery: a prospective, double-blind, randomized study. Spine (Phila Pa 1976) 33:2379–2386. https://doi.org/10.1097/BRS.0b013e3181844ef2
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Ethics approval
This is an observational study. The hospital’s Research Council has confirmed that no ethical approval is required.
Conflict of interest
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Comments
Nice well conducted study demonstrating that intrathecal opiod administration, reduces post operative pain on POD1 and need for opiods on POD2. None CSF leaks were noted in the current study, but this risk and the similar effect on pain and opiod consumption on POD3-4, will probably still cause some reluctance towards ITO in the spine community.
Carsten Reides Bjarkam.
Aalborg,Denmark.
The authors of this paper compared their institutional experience with intrathecal administration of different opioids at the end of uncomplicated lumbar fusion procedures—among three groups (morphine vs. morphine + fentanyl vs. none), there were no differences in side effects or complications, but the groups with intrathecal injection had less pain during first day or two after the surgery. The patients were not randomized, and only one- and two-level transforaminal interbody fusions were included in the review.
Although there were no technical or medication-related issues with intrathecal opioid administrations, one may expect them to occur at some point as both the dural penetration and the intrathecal morphine (known from decades of intrathecal morphine trialing for patients with chronic pain) can indeed results in various unpleasant problems, from CSF leaks and seromas, to meningitis and morphine-related itching and hyperalgesia.
Ultimately, recommendation on whether to accept this approach will be determined by prospective randomized studies, perhaps comparing intrathecal opioid administration with application of epidural paste, and then determining if addition of anti-inflammatory medications and/or local anesthetics would make effects more noticeable.
Konstantin Slavin,
Chicago, USA.
This article is part of the Topical Collection on Neurosurgery general.
Rights and permissions
Springer Nature or its licensor holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Villavicencio, A., Taha, H.B., Nelson, E.L. et al. The effect of intraoperative intrathecal opioid administration on the length of stay and postoperative pain control for patients undergoing lumbar interbody fusion. Acta Neurochir 164, 3061–3069 (2022). https://doi.org/10.1007/s00701-022-05359-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00701-022-05359-8