Abstract
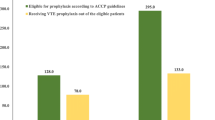
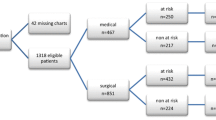
Venous thromboembolism (VTE) remains the number one preventable cause of hospital acquired mortality and morbidity. Each year, more than 12 million patients are at risk for VTE. The delivery of appropriate and timely VTE prophylaxis is still suboptimal in many healthcare institutions and can lead to increased readmissions, morbidity, as well as costs. To clarify this issue further, we performed a retrospective case control study at our institution to determine if poor adherence to the VTE prophylaxis guidelines could lead to an increase in VTE events. This was a retrospective case control study conducted at Winthrop-University Hospital from January 2007 to December 2011. Exclusion criteria were age < 18 and concurrent use of anticoagulant agents. Out of 322 cases of hospital acquired VTE or readmission with VTE within 30 days of discharge, 289 cases were selected for final analysis and paired with age and sex matched controls. Patients with a hospital acquired VTE or a readmission for VTE within 30 days of discharge had a significantly reduced rate of VTE prophylaxis when compared to the control group (54.0 vs. 79.2 %, p < 0.0001). The VTE risk assessment rate was also lower in the VTE group (77.2 vs. 85.5 %, p = 0.035). No difference was noted in the time to prophylaxis administration between the two groups (34.8 vs. 33.1 h, p = 0.34). Lastly, sequential compression device (SCD) documentation rate was not different: 68/116 (58.6 %) vs. 44/87 (50.6 %), p = 0.32, between the two arms. Low adherence to the American College of Chest Physician (ACCP) guidelines for VTE prophylaxis correlated with an increase in hospital acquired VTE. The decreased adherence may be linked to a lower VTE risk assessment rate, and other barriers including incorrect identification of contraindications to pharmacologic prophylaxis, and poor documentation of mechanical prophylaxis. There was no difference in SCD documentation rate and timeliness to administration of initial thromboprophylaxis between the two groups. Future studies are needed to reassess adherence and documentation rates after system-wide improvements.

Similar content being viewed by others
References
Heit JA, Melton LJ 3rd, Lohse CM et al (2001) Incidence of venous thromboembolism in hospitalized patients vs community residents. Mayo Clin Proc 76:1102–1110
Anderson FA Jr, Zayaruzny M, Heit JA et al (2007) Estimated annual numbers of US acute-care hospital patients at risk for venous thromboembolism. Am J Hematol 82:777–782
Ruppert A, Steinle, Lees M (2011) Economic burden of venous thromboembolism: a systematic review. J Med Econ 14:65–74
MacDougall DA, Feliu AL, Boccuzzi SJ et al (2006) Econonimc burden of deep vein thrombosis, pulmonary embolism, and post-thrombotic syndrome. Am J Health Syst Pharm 63(20 Suppl 6):S5–S15
Guanella R, Ducruet T, Johri M et al (2011) Economic burden and cost determinants of deep vein thrombosis during 2 years following diagnosis: a prospective evaluation. J Thromb Haemost 9:2397–2405
Guyatt GH, Akl EL, Crowther M et al (2012) Executive summary: antithrombotic therapy and prevention of thrombosis, 9th ed: American College of Chest Physicians evidence-based clinical practice guidelines. CHEST 141(2 Suppl):7S–47S
Languasco A, Galante M, Marín J et al (2011) Adherence to local guidelines for venous thromboprophylaxis: a cross-sectional study of medical inpatients in Argentina. Thromb J 15(9):18
Kahn SR, Panju A, Geerts W, CURVE study investigators (2007) Multicenter evaluation of the use of venous thromboembolism prophylaxis in acutely ill medical patients in Canada. Thromb Res 119(2):145–155
Tapson VF, Decousus H, Pini M et al (2007) Venous thromboembolism prophylaxis in acutely ill hospitalized medical patients: findings from the International Medical Prevention Registry on Venous Thromboembolism. CHEST 132:936–945
Cohen AT, Victor FT, Jean-Francois B et al (2008) Venous thromboembolism risk and prophylaxis in the acute hospital care setting (ENDORSE study): a multinational cross-sectional study. The Lancet 371:387–394
Anderson FA Jr, Spencer FA (2003) Risk factors for venous thromboembolism. Circulation 107:I9–I16
Geerts WH, Bergqvist D, Pineo GF et al (2008) Prevention of Venous Thromboembolism: American College of Chest Physicians Evidence-Based Clinical Practice Guidelines (8th Edition). Chest 133(6_suppl):381S–453S
Kakkar AK, Cimminiello C, Goldhaber SZ, LIFENOX Investigators (2011) Low-molecular-weight heparin and mortality in acutely ill medical patients. N Engl J Med 365(26):2463–2472
Schleyer AM, Schreuder AB, Jarman KM et al (2011) Adherence to guideline-directed venous thromboembolism prophylaxis among medical and surgical inpatients at 33 academic medical centers in the United States. Am J Med Qual 26(3):174–180
Cook D, Tkaczyk A, Lutz K et al (2009) Thromboprophylaxis for hospitalized medical patients: a multicenter qualitative study. J Hosp Med 4(5):269–275
Daniel D, Maund C, Butler K (2010) Community hospital participation in a pilot project for venous thromboembolism quality measures: learning, collaboration, and early improvement. Jt Comm J Qual Patient Saf 36(7):301–309
Piazza G, Goldhaber SZ (2009) Computerized decision support for the cardiovascular clinician: applications for venous thromboembolism prevention and beyond. Circulation 120(12):1133–1137
Bratzler DW, Hunt DR (2006) The surgical infection prevention and surgical care improvement projects: national initiatives to improve outcomes for patients having surgery. Clin Infect Dis 43:322–330
Kucher N, Koo S, Quiroz R et al (2005) Electronic alerts to prevent venous thromboembolism among hospitalized patients. N Engl J Med 352(10):969–977
Fiumara K, Piovella C, Hurwitz S et al (2010) Multi-screen electronic alerts to augment venous thromboembolism prophylaxis. Thromb Haemost 103(2):312–317
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
None.
Rights and permissions
About this article
Cite this article
Suh, J., Desai, A., Desai, A. et al. Adherence to thromboprophylaxis guidelines in elderly patients with hospital acquired venous thromboembolism: a case control study. J Thromb Thrombolysis 43, 172–178 (2017). https://doi.org/10.1007/s11239-016-1432-6
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11239-016-1432-6