Abstract
Background context
Preoperative (pre-op) identification of patients likely to achieve a clinically meaningful improvement following surgery for adult spinal deformity (ASD) is critical, especially given the substantial cost and comorbidity associated with surgery. Even though pain is a known indication for surgical ASD correction, we are not aware of established thresholds for baseline pain and function to guide which patients have a higher likelihood of improvement with corrective surgery.
Purpose
We aimed to establish pre-op patient-reported outcome measure (PROM) thresholds to identify patients likely to improve by at least one minimum clinically important difference (MCID) with surgery for ASD.
Study design
This is a retrospective cohort study using prospectively collected data.
Patient sample
We reviewed 172 adult patients’ charts who underwent corrective surgery for spinal deformity.
Outcome measures
Included measures were the Visual Analog Scale for pain (VAS), Oswestry Disability Index (ODI), and Scoliosis Research Society-22 (SRS-22). Our primary outcome of interest was improvement by at least one MCID on the ODI and SRS-22 at 2 years after surgery.
Methods
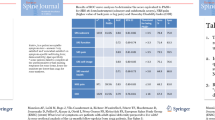
As part of usual care, the VAS, ODI, and SRS-22 were collected pre-op and re-administered at 1, 2, and 5 years after surgery. MCIDs were calculated using a distribution-based method. Determining significant predictors of MCID at two years was accomplished by Firth bias corrected logistic regression models. Significance of predictors was determined by Profile Likelihood Chi-square. We performed a Youden analysis to determine thresholds for the strongest pre-op predictors.
Results
At year two, 118 patients (83%) reached MCID for the SRS and 127 (75%) for the ODI. Lower pre-op SRS overall, lower pre-op SRS pain, and higher pre-op SRS function predicted a higher likelihood of reaching MCID on the overall SRS (p < 0.05). Higher pre-op ODI, lower SRS pain and self-image, and higher SRS overall predicted a higher likelihood of reaching MCID on the ODI (p < 0.05). An ODI threshold of 29 predicted reaching MCID with a sensitivity of 0.89 and a specificity of 0.64 (AUC = 0.7813). An SRS threshold of 3.89 predicted reaching MCID with a sensitivity of 0.93 and specificity of 0.68 (AUC = 0.8024).
Conclusions
We identified useful thresholds for ODI and SRS-22 with acceptable predictive ability for improvement with surgery for ASD. Pre-op ODI, SRS, and multiple SRS subscores are predictive of meaningful improvement on the ODI and/or SRS at 2 years following corrective surgery for spinal deformity. These results highlight the usefulness of PROMs in pre-op shared decision-making.





Similar content being viewed by others
References
Liu S, Ames CP, Mundis G, Hostin R, Kebaish K, Deviren V et al (2014) Likelihood of reaching minimal clinically important difference in adult spinal deformity: a comparison of operative and nonoperative treatment. Ochsner J 14:11
Youssef JA, Orndorff DO, Patty CA, Scott MA, Price HL, Hamlin LF et al (2013) Current status of adult spinal deformity. Glob Spine J 03:051–62. https://doi.org/10.1055/s-0032-1326950
Bridwell KH, Glassman S, Horton W, Shaffrey C, Schwab F, Zebala LP et al (2009) Does treatment (nonoperative and operative) improve the two-year quality of life in patients with adult symptomatic lumbar scoliosis: a prospective multicenter evidence-based medicine study. Spine 34:2171–2178. https://doi.org/10.1097/BRS.0b013e3181a8fdc8
Yadla S, Maltenfort MG, Ratliff JK, Harrop JS (2010) Adult scoliosis surgery outcomes: a systematic review. Neurosurg Focus 28:E3. https://doi.org/10.3171/2009.12.FOCUS09254
Moal B, Lafage V, Smith JS, Ames CP, Mundis G, Terran JS et al (2015) Clinical improvement through surgery for adult spinal deformity: What can be expected and who is likely to benefit most? Spine Deform 3:566–574. https://doi.org/10.1016/j.jspd.2015.04.004
Baumhauer JF, Bozic KJ (2016) Value-based healthcare: patient-reported outcomes in clinical decision making. Clin Orthop 474:1375–1378. https://doi.org/10.1007/s11999-016-4813-4
Rihn JA, Currier BL, Phillips FM, Glassman SD, Albert TJ (2013) Defining the value of spine care. J Am Acad Orthop Surg 21:419–426. https://doi.org/10.5435/JAAOS-21-07-419
Patrick DL, Guyatt GH, Acquadro C (2008) Patient-reported outcomes. Cochrane Handb Syst Rev Interv., Wiley-Blackwell; pp 531–45 https://doi.org/10.1002/9780470712184.ch17
Asher M, Min Lai S, Burton D, Manna B (2003) The Reliability and concurrent validity of the scoliosis research society-22 patient questionnaire for idiopathic scoliosis. Spine 28:63
Schwab F, Farcy J-P, Bridwell K, Berven S, Glassman S, Harrast J et al (2006) A clinical impact classification of scoliosis in the adult. Spine 31:2109. https://doi.org/10.1097/01.brs.0000231725.38943.ab
Little DG, MacDonald D (1994) The use of the percentage change in oswestry disability index score as an outcome measure in lumbar spinal surgery. Spine 19:2139–2142. https://doi.org/10.1097/00007632-199410000-00001
Fairbank JCT, Pynsent PB (2000) The oswestry disability index. Spine 25:2940
Zanoli G, Strömqvist B, Jönsson B (2001) Visual analog scales for interpretation of back and leg pain intensity in patients operated for degenerative lumbar spine disorders. Spine 26:2375
Singh JA, Gabriel S, Lewallen D (2008) The impact of gender, age, and preoperative pain severity on pain after TKA. Clin Orthop 466:2717–2723. https://doi.org/10.1007/s11999-008-0399-9
Ho B, Houck JR, Flemister AS, Ketz J, Oh I, DiGiovanni BF et al (2016) Preoperative PROMIS scores predict postoperative success in foot and ankle patients. Foot Ankle Int 37:911–918. https://doi.org/10.1177/1071100716665113
Carreon LY, Glassman SD, Djurasovic M, Dimar JR, Johnson JR, Puno RM et al (2009) Are preoperative health-related quality of life scores predictive of clinical outcomes after lumbar fusion? Spine 34:725. https://doi.org/10.1097/BRS.0b013e318198cae4
Khor S, Lavallee D, Cizik AM, Bellabarba C, Chapman JR, Howe CR et al (2018) Development and validation of a prediction model for pain and functional outcomes after lumbar spine surgery. JAMA Surg. https://doi.org/10.1001/jamasurg.2018.0072
McGirt MJ, Sivaganesan A, Asher AL, Devin CJ (2015) Prediction model for outcome after low-back surgery: individualized likelihood of complication, hospital readmission, return to work, and 12-month improvement in functional disability. Neurosurg Focus 39:E13. https://doi.org/10.3171/2015.8.FOCUS15338
Smith JS, Shaffrey CI, Glassman SD, Carreon LY, Schwab FJ, Lafage V et al (2013) Clinical and radiographic parameters that distinguish between the best and worst outcomes of scoliosis surgery for adults. Eur Spine J 22:402–410. https://doi.org/10.1007/s00586-012-2547-x
Smith JS, Shaffrey CI, Lafage V, Schwab F, Scheer JK, Protopsaltis T et al (2015) Comparison of best versus worst clinical outcomes for adult spinal deformity surgery: a retrospective review of a prospectively collected, multicenter database with 2-year follow-up: presented at the 2015 AANS/CNS joint section on disorders of the spine and peripheral nerves. J Neurosurg Spine 23:349–359. https://doi.org/10.3171/2014.12.SPINE14777
Berliner JL, Brodke DJ, Chan V, SooHoo NF, Bozic KJ (2017) Can preoperative patient-reported outcome measures be used to predict meaningful improvement in function after TKA? Clin Orthop Relat Res 475:149–157. https://doi.org/10.1007/s11999-016-4770-y
Berliner JL, Brodke DJ, Chan V, SooHoo NF, Bozic KJ (2016) John charnley award: preoperative patient-reported outcome measures predict clinically meaningful improvement in function after THA. Clin Orthop Relat Res 474:321–329. https://doi.org/10.1007/s11999-015-4350-6
Weinreb JH, Bianco KL, Lafage V, Schwab F (2014) Indications for Adult Spinal Deformity Surgery. Minim Invasive Spinal Deform Surg. Springer, Vienna; p. 21–31. https://doi.org/10.1007/978-3-7091-1407-0_3
Bess S, Boachie-Adjei O, Burton D, Cunningham M, Shaffrey C, Shelokov A et al (2009) Pain and disability determine treatment modality for older patients with adult scoliosis, while deformity guides treatment for younger patients. Spine 34:2186. https://doi.org/10.1097/BRS.0b013e3181b05146
Copay AG, Subach BR, Glassman SD et al (2007) Understanding the minimum clinical important difference (MCID). A review of concepts and methods. Spine J 7:541–546
Copay AG, Glassman SD, Subach BR et al (2008) Minimum clinically important difference in lumbar spine surgery patients: a choice of methods using the oswestry disability index, medical outcomes study questionnaires short form 36, and pain scales. Spine J 8:968–974
Crosby RD, Kolotkin RL, Williams GR (2003) Defining clinically meaningful change in health-related quality of life. J Clin Epidemiol 56:395–407
Hagg O, Fritzell P, Nordwall A (2003) The clinical importance of changes in outcome scores after treatment for chronic low back pain. Eur Spine J 12:12–20
Harris PA, Taylor R, Thielke R, Payne J, Gonzalez N, Conde JG (2009) Research electronic data capture (REDCap)—a metadata-driven methodology and workflow process for providing translational research informatics support. J Biomed Inform 42:377–381. https://doi.org/10.1016/j.jbi.2008.08.010
Haefeli M, Elfering A (2006) Pain assessment. Eur Spine J 15:S17–24. https://doi.org/10.1007/s00586-005-1044-x
Huskisson EC (1974) Measurement of pain. The Lancet 304:1127–1131. https://doi.org/10.1016/S0140-6736(74)90884-8
Asher MA, Lai SM, Burton DC (2000) Further development and validation of the scoliosis research society (srs) outcomes instrument. Spine 25:2381–2386
O’Brien MF, Kurklo TR, Blanke K, Lenke L (eds) (2005) Spinal deformity study group radiographic measurement manual. Medtronic Sofarmor Danek, Memphis
Ames CP, Smith JS, Scheer JK et al (2012) Impact of spinopelvic alignment on decision making in deformity surgery in adults: a review. J Neurosurg Spine 16(6):547–564
Wang X (2014) Firth logistic regression for rare variant association tests. Front Genet 5:187. https://www.frontiersin.org/article/10.3389/fgene.2014.00187
DeLong ER, DeLong DM, Clarke-Pearson DL (1988) Comparing the areas under two or more correlated receiver operating characteristic curves: a nonparametric approach. Biometrics 44:837–845. https://doi.org/10.2307/2531595
Parker SL, Mendenhall SK, Shau D, Adogwa O, Cheng JS, Anderson WN et al (2011) Determination of minimum clinically important difference in pain, disability, and quality of life after extension of fusion for adjacent-segment disease. J Neurosurg Spine 16:61–67. https://doi.org/10.3171/2011.8.SPINE1194
Revicki D, Hays RD, Cella D, Sloan J (2008) Recommended methods for determining responsiveness and minimally important differences for patient-reported outcomes. J Clin Epidemiol 61:102–109. https://doi.org/10.1016/j.jclinepi.2007.03.012
Schwind J, Learman K, O’Halloran B, Showalter C (2013) Cook C (2013) Different minimally important clinical difference (MCID) scores lead to different clinical prediction rules for the Oswestry disability index for the same sample of patients. J Man Manip Ther 21(2):71–78. https://doi.org/10.1179/2042618613Y.0000000028
Copay AG, Glassman SD, Subach BR, Berven S, Schuler TC, Carreon LY (2008) Minimum clinically important difference in lumbar spine surgery patients: a choice of methods using the oswestry disability index, medical outcomes study questionnaire short form 36, and pain scales. Spine J 8:968–974. https://doi.org/10.1016/j.spinee.2007.11.006
Crawford CH, Glassman SD, Bridwell KH, Berven SH, Carreon LY (2015) The minimum clinically important difference in SRS-22R total score, appearance, activity and pain domains after surgical treatment of adult spinal deformity. Spine 40:377–381. https://doi.org/10.1097/BRS.0000000000000761
Carreon LY, Sanders JO, Diab M, Sucato DJ, Sturm PF, Glassman SD et al (2010) The minimum clinically important difference in Scoliosis Research society-22 appearance, activity, and pain domains after surgical correction of adolescent idiopathic scoliosis. Spine 35:2079–2083. https://doi.org/10.1097/BRS.0b013e3181c61fd7
Djurasovic M, Glassman SD, Sucato DJ, Lenke LG, Crawford CH, Carreon LY (2018) Improvement in scoliosis research society-22R pain scores after surgery for adolescent idiopathic scoliosis. Spine 43:127–132. https://doi.org/10.1097/BRS.0000000000001978
Sanders JO, Carreon LY, Sucato DJ, Sturm PF, Diab M, Group SDS (2010) Preoperative and perioperative factors effect on adolescent idiopathic scoliosis surgical outcomes. Spine 35:1867. https://doi.org/10.1097/BRS.0b013e3181efa6f5
Theologis AA, Ailon T, Scheer JK, Smith JS, Shaffrey CI, Bess S et al (2016) Impact of preoperative depression on 2-year clinical outcomes following adult spinal deformity surgery: the importance of risk stratification based on type of psychological distress. J Neurosurg Spine 25:477–485. https://doi.org/10.3171/2016.2.SPINE15980
Bakhsheshian J, Scheer JK, Gum JL, Hostin R, Lafage V, Bess S et al (2017) Impact of poor mental health in adult spinal deformity patients with poor physical function: a retrospective analysis with a 2-year follow-up. J Neurosurg Spine 26(1):116–124. https://doi.org/10.3171/2016.5.SPINE151428
Bridwell KH, Glassman S, Horton W, Shaffrey C, Schwab F, Zebala LP et al (2009) Does treatment (nonoperative and operative) improve the two-year quality of life in patients with adult symptomatic lumbar scoliosis: a prospective multicenter evidence-based medicine study. Spine (Phila Pa 1976) 34:2171–2178
Smith JS, Shaffrey CI, Lafage V, Schwab F, Scheer JK et al (2015) Comparison of best versus worst clinical outcomes for adult spinal deformity surgery: a retrospective review of a prospectively collected, multicenter database with a 2-year follow-up. J Neurosurg Spine 23:349–359
Glassman SD, Hamill CL, Bridwell KH, Schwab FJ, Dimar JR, Lowe TG (2007) The impact of perioperative complications on clinical outcome in adult deformity surgery. Spine (Phila Pa 1976) 32:2764–2770
Smith JS, Shaffrey CI, Glassman SD, Berven SH, Schwab FJ, Hamill CL et al (2011) Risk-benefit assessment of surgery for adult scoliosis: an analysis based on patient age. Spine (Phila Pa 1976) 36:817–824
van Hooff ML, Mannion AF, Staub LP, Ostelo RW, Fairbank JC (2016) Determination of the Oswestry Disability Index score equivalent to a "satisfactory symptom state" in patients undergoing surgery for degenerative disorders of the lumbar spine-a Spine Tango registry-based study. Spine J16(10):1221–1230. https://doi.org/10.1016/j.spinee.2016.06.010
Funding
No external funding source.
Author information
Authors and Affiliations
Contributions
AL-M BA: Study design, manuscript daft, review, final approval and accountable for the work to be published. ET MD: Design, manuscript preparation, review, final approval, overall study management and accountable for the work to be published. KJB, MD: Study conception, manuscript draft, review, final approval and accountable for the work to be published. DS, PhD: Study design, data collection, manuscript preparation, review, final approval and accountable for the work to be published. TCL MD: Study conception, data analysis, manuscript preparation, review, final approval and accountable for the work to be published. JKS, MD: Study conception, manuscript preparation, review, final approval and accountable for the work to be published. MJM, PhD: Study conception, data analysis, manuscript preparation, review, final approval and accountable for the work to be published.
Corresponding author
Ethics declarations
Conflict of interest
Andrea Leyton-Mange, Devender Singh, Tiffany C Liu, Michael J Mahometa: None; Eeric Truumees: Stryker spine (royalty); Doctoral research group (stock); Relievant Medsystems, Stryker, Medtronic, KUROS, Seikagau Corporation (research support); North American Spine Society (board member); Kevin Bozic: Agency for Healthcare Research and Quality (research support); Harvard business school institute for strategy and competitiveness (consultant-unpaid); Carrum Health (stock options); Centers for Medicare and Medicaid Services and Cardinal Analytx (consultant-paid); John K Stokes: Genesys spine (royalty); Difusion and Summit Medventures (stock); Matthew J Geck: Difusion (stock), SpineHope (Board member:unpaid).
Ethical approval (IRB)
Approved by Institutional review board.
Informed consent
Not applicable.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Appendix
Rights and permissions
About this article
Cite this article
Leyton-Mange, A., Truumees, E., Bozic, K.J. et al. Preoperative patient-reported outcome score thresholds predict the likelihood of reaching MCID with surgical correction of adult spinal deformity. Spine Deform 9, 207–219 (2021). https://doi.org/10.1007/s43390-020-00171-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s43390-020-00171-9