Return to work and recovery time analysis after outpatient endoscopic lumbar transforaminal decompression surgery
Introduction
The rising cost of health care has become a major concern for large self-insured employers. Annual productivity losses due to sick leave are simply staggering to the point where many large corporations have begun to internally study the feasibility of direct contracting with centers of excellence with reliably proven best clinical practices, excellent outcomes and a high return to work (RTW) rates and short recovery times (RT) of their employees. This trend is not only motivated by out-of-control increases in health insurance premiums, but also by the need for improved management of their human resources. Low back pain related missed workdays are at the top of the list costing an estimated $28 billion per year in the United States alone (1-3). Other causes of chronic disability include cardiovascular disease, mental health, and cancer (4-6). Work disability stemming from these chronic problems is expected to escalate with high labor participation rates among people anticipated to live longer (7). Therefore, the ability for employers to predict RTW at a highly functional level with medical interventions of these chronic diseases has become a significant focus of internal research in an attempt to more effectively allocate corporate resources to improved value-based health care delivery to their employees. The objective is simple—reducing the personal hardship to their employees, as well as the financial, and public health burden (8). In this context, surgical treatment of low back pain syndromes has seen some significant scrutiny as not only a costly, but a potentially career changing- or ending event putting the employers’ investment into valuable, highly trained and experienced employees at risk (9-12).
Minimally invasive and endoscopic lumbar spine decompression techniques have become popular in spinal surgery (13-16). There has been a substantial increase of endoscopic procedures being carried out in an ambulatory surgery center (ASC) at a reduced burden to patients (17,18). The advantages of endoscopic decompressions are obvious: Fewer postoperative complications, a shorter interval to social reintegration (19) and postoperative narcotic independence, and an overall reduced utilization of painkillers (20). While many of these advantages have been conclusively proven in the medical literature using standardized primary outcome measures, RTW is a “real-world” economic indicator highly relevant to employers trying to predict future work success (21).
Returning employees to work after spine surgery is a multifactorial problem of high complexity with many determinants beyond the disease going into the equation. Therefore, self-reported RTW analysis may be a less biased and perhaps more accurate assessment of the burden to the patient due to a surgical intervention. The purpose of this study was to correlate patient self-reported RTW and RT data with clinical outcomes of the lumbar endoscopic transforaminal decompression procedure in patients with a broad spectrum of health conditions, types of lifestyles and employment to establish useful benchmarks for patients, employers, payers, and surgeons. The authors did this by performing Kaplan-Meier survival analysis of the duration of the postoperative time interval before returning to work and to recovery from surgery to assist in the management of return-to-work expectations with the spinal endoscopy procedure.
Methods
Patient population
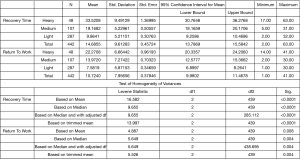
This retrospective study included 442 consecutive patients seen in our clinic who underwent outpatient lumbar endoscopic transforaminal foraminoplasty and discectomy between 2011 and 2016. The mean follow-up was 33.5 months ranging from 24 to 85 months with a standard deviation of 12.83 months at the time this study was concluded. The patients’ age ranged from 30 to 85 years with a mean age of 40.92 years (Figure 1). The inclusion and exclusion criteria for this study have been published elsewhere (22-25). All patients were treated for contained disc herniation with associated lateral recess and foraminal stenosis. This study by chance did not include any workman’s compensation (WC) patients.
Preoperative work up and surgical decision making
Patients were worked up with a thorough history, physical examination, and imaging studies. Patients were subjected to an interventional diagnostic workup with lidocaine containing transforaminal epidural steroid injection (TESI) under biplanar fluoroscopic image intensifier guidance using established protocols (26-28). A TESI was considered diagnostic if the patient reported an immediate (within 15 min) VAS scale reduction >50% (29,30). Patients with conclusive diagnostic workup with matching clinical symptoms, MRI findings, diagnostic TESI response, and supporting history and physical examination were ultimately deemed appropriate surgical candidates for the endoscopic transforaminal decompression procedure. A number of radiographic classifications of foraminal and lateral recess stenosis described elsewhere were employed by the authors (31-33) to grade the preoperative MRI scan (25) by defining the location of the offending pathology within the neuroforamen. The heights of the posterior intervertebral disc and lumbar foramina were evaluated according to Hasegawa (34), who described a lumbar neuroforaminal height of 15 mm or more as normal and reduced posterior intervertebral disc height of 3 to 4 mm as suggestive of spinal stenosis. Only patients with a neuroforaminal width of 3 mm or less on the sagittal MRI cuts or lateral recess height of 3 mm or less on the axial MRI cuts were considered “stenotic” and treated surgically.
Clinical follow-up
Primary clinical outcome measures were reductions in the VAS for leg pain ranging from no pain [0] to worst pain [10] (29) and the Macnab criteria (31). Briefly, follow-up results were classified as Excellent if the patient had little pain and returned to desired activities with few limitations. Outcomes were classified as Good if the patient reported occasional pain or dysesthesias with daily activities with minor restrictions, and did not need any pain medication. Patients were assigned to one of the two remaining categories if their pain improved somewhat but they continued to need pain medication (Fair), or if their function worsened or they needed additional surgery to address their symptoms (Poor). Patients were asked whether they went to an emergency room, or were admitted to a hospital for any postoperative complications or sequelae (unavoidable problems following an expertly executed surgery). Any kind of additional treatment or surgery within 90 days was recorded as “re-incisions” related to the index endoscopic decompression surgery.
Surgical techniques & postoperative rehabilitation
All surgical procedures employed the endoscopic transforaminal approach using the “outside-in” technique (35,36) and employs a foraminoplasty in patients with or without lateral stenosis for the treatment of herniated disc. The author has published the details of the surgical decompression of this study group of patients elsewhere (22-24). Most patients did not require postoperative rehabilitation and supportive care requirements. Some patients were treated for postoperative irritation of the dorsal root ganglion with nonsteroidal anti-inflammatories, gabapentin, and TESI to treat any dysesthetic leg pain syndromes.
Return-to-work & RT analysis
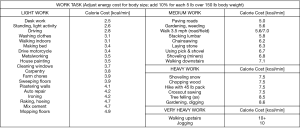
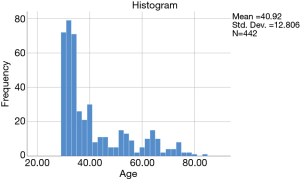
Only gainfully employed patients who were working leading up to the endoscopic decompression surgery were included in this study. The type of physical work was classified according to energy consumption per minute (Kcal/min) as Light, Medium, Heavy, and Very Heavy using guidelines adopted from U.S. Department of Labor published in the online Dictionary of Occupational Titles (Washington, D.C.: U.S. Government Printing Office; Table 1) (37,38). Patients were grouped into these categories by published energy requirements of common work tasks (Figure 2) (39,40). The postoperative RTW rate was calculated. The RT was recorded as a patient self-reported postoperative outcome measure (PROM) when patient considered themselves recovered from surgery and narcotic independence was achieved. Patients were also asked whether they had convalesced from the surgery defined as no incisional pain, and no residual anesthesia side effects, such as nausea or vomiting. The number of postoperative RTW and RT days was calculated as the difference between the date of the surgery and the postoperative visit date. Patients were asked during their postoperative visits—typically within three months after the endoscopic decompression procedure—whether they had returned to work at a functional level similar to their preoperative function. The authors intentionally did not further elaborate on the definition of RTW or RT to patients since a recent research on PROMs suggested that outcomes are reported differently by patients depending on how the question concerning the functional context—whose relevancy may differ from patient to patient—is asked (41). In an attempt to minimize the introduction of additional biases in the responses collected from patients, the RTW and RT inquiry was intentionally left as is to ask the question as directly as possible. In other words, RT (defined in this study as postoperative narcotic independence) was obtained as an additional gross estimate of the time elapsed to recuperation from the endoscopic transforaminal surgery independent from the plethora of other contributing factors that may influence RTW or RT decision on the patients’, employers’, or treating surgeons’ part. Additional objective patient data obtained included pre- and postoperative walking distance to the pain limit. The authors intentionally relied on these patient-reported outcome data (PROMs), which recently have been reported to be more reliable estimators of patient satisfaction, and return to function (41).
Full table
Correlative RTF analysis and surgical outcomes
For the clinical outcome, and RTW and RT analysis, descriptive statistics (mean and standard deviation), cross tabulation statistics and measures of association were computed for two-way tables using IBM SPSS Statistics software, Version 25.0. The Pearson χ2 and the likelihood-ratio χ2 tests were used as statistical measures of association. At final follow-up, primary clinical outcomes measures for patients who underwent the endoscopic transforaminal decompression procedure were assessed using modified Macnab criteria (31). The authors stratified patients towards Excellent and Good clinical outcomes by lessons learned with the intent of refining indications and patient selection criteria for endoscopic decompression under local anesthesia. In the case of Fair and Poor Macnab outcomes, patients’ postoperative imaging studies were scrutinized for instability, recurrent stenosis at the index level. Patients were also asked to select a score on the visual analog scale (VAS) preoperatively (Preop VAS), and at final follow-up (Postop F/U VAS) (29) For the detailed outcome analysis, two-tailed t-test, ANOVA testing, and cross-tabulation statistics and measures of association were computed for two-way tables using IBM SPSS Statistics software, Version 25.0. Descriptive statistic measures were used to calculate the mean, range, and standard deviation as well as percentages. Crosstabulation methods were used to assess for any statistically significant association between RTW/ RT data and clinical outcome data. Pearson Chi-Square and Fisher’s Exact Test were employed as statistical measures of association. Expected cell counts, continuity corrections, and likelihood ratios were calculated for some analyses.
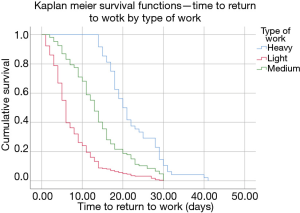
Kaplan-Meier (K-M) survival time (time to RTW and RT) probabilities and curves were constructed from tables containing: (I) patients’ serial time; (II) their status at serial time {Macnab outcome – Excellent [1], Good [2], Fair [3], and Poor [4]; 0=censored if the total survival time for a patient could not be accurately assessed}, and (III) study groups (type of work: Light. Medium, and Heavy). These tables were sorted in an ascending manner beginning with the shortest serial times for each group. Patients who would have been censored included patients who dropped out of the study, were lost to follow-up, or in whom required data was not available. In this study, this data was not missing. The cumulative probability of having returned to work and having recovered excluding censored events is seen on the Y-axis of the K-M plot allowing to analyze patient treatment intervals of varying duration. The difference between the type of work RTW & RT (K-M survival) curves was quantified for statistical significance using the log rank test which was used to calculated the chi-square (χ2) for each event time in the two treatment arms. The summed results for each group were added to derive the ultimate chi-square to compare the full K-M curves obtained for the RTW and RT analysis. The confidence intervals (95%) for the likelihood ratios were calculated using the “log rank method” according to Altman et al. (42).
Results
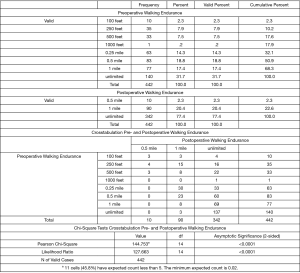
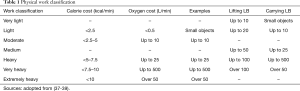
Excellent (237/442) and Good (133/442) results according to the Macnab criteria, were obtained in 83.7% (370/442) of patients following the endoscopic transforaminal decompression procedure. Fair results were reported by 43 patients (9.7%), and Poor results by 29 (6.6%), respectively. The mean preoperative VAS was 8.08 (Min 6, Max 10; STD 1.45). The mean postoperative VAS was reduced to 2.55 (Min 0, Max 6; STD 1.52) at a statistically significant level on two-tailed paired t-test (P<0.0001). The preoperative work was characterized as Heavy in 10.9% (48/442) of patients, as Medium in 24.1% (107/442) of patients, as Light in another 64.9% (287/442) of patients, respectively. The overall RTW rate was 92.5% (409/442). As expected, patients performing Heavy (RTW rate =87.5%) and Medium (RTW rate =86.0%) work had a lower RTW rate than patients who were performing Light (95.8%) jobs (Table 2). ANOVA testing showed no statistically significant difference in the mean preoperative VAS between the type of work (Heavy, Medium, and Light) groups. There was a statistically significant difference in postoperative VAS between the Light-work type group (2.4) on the one hand, and the Medium (2.81)- and Heavy (2.89) type workgroup on the other hand on posthoc analysis with Turkey’s B calculation (P=0.015). Crosstabulation of outcomes versus radiographic indicators of advanced disc degeneration including posterior disc height of less than 3 mm, or the size of the disc herniation did not have any statistically significant association with the type of work, RTW, or RT data on chi-square testing. As an additional objective measure of patient outcomes, the preoperative walking endurance was compared to the postoperative walking endurance (Figure 3). Preoperatively, only 31.7% (140/442) had unlimited walking endurance. Another 17.4% (77/442) could walk up to 1 mile preoperatively until they had to stop. The remaining 50.9% (225/442) had significant restrictions of their ability to walk to the pain limit with their walking endurance limited to less than 0.5 miles. Crosstabulation of pre- and postoperative walking endurance and chi-square testing showed statistically significant improvement (P<0.0001) of walking endurance with 77.4% (342/442) of patients having unlimited walking endurance and another 20.4% (90/442) of patients having pain-free walking endurance up to one mile (Figure 3).
Full table
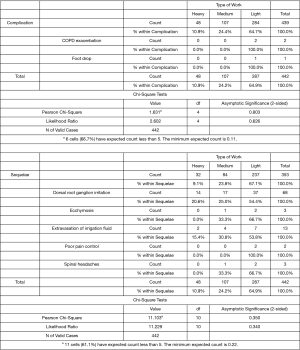
There were no major approach or anesthesia-related problems but a few clinical complications (Figure 4). There were no re-incisions within three months from the endoscopic index surgery. Neither was RTW or RT data affected at a statistically significant level by complications (3/442), postoperative visits to the emergency room (4/442) for management of postoperative dysesthesias due to irritation of the dorsal root ganglion (DRG). The complication rate was 0.7% due to 2 patients with Light duty jobs (0.5%) that were admitted to the hospital for management of their acute COPD exacerbation postoperatively. One additional patient with a Light-duty job suffered from a postoperative foot drop with transitory 3/5 weakness in the extensor hallucis longus following an L4/5 transforaminal endoscopic decompression for severe foraminal stenosis. The latter patient’s RTW was unaffected by the transitory foot drop, which fully recovered with supportive care measures (Figure 4). There were no reherniations in the study population. Postoperative sequelae defined as unavoidable side effects of an otherwise expertly executed surgery occurred in an additional 20.14% (89/442) patients (Figure 4). The sequelae in these 89 patients included extravasation of irrigation fluid into the subcutaneous tissues in 13 patients (2.94% of n=442), poorly controlled postoperative incisional pain in 4 patients (0.9% of n=442), spinal headaches in 3 patients (0.68%; n=442). There was no statistically significant difference in the distribution of these sequelae between the Heavy, Medium, and Light workgroup patients (Figure 4) and RTW and RT were not affected by the occurrence of these sequelae at a statistically significant level. In comparison, postoperative DRG irritation, which occurred in another 68 patients (15.38%; n=442), delayed RTW to a mean of 18.94 days (P<0.0001) and RT (P<0.001) to 15.31 days on ANOVA testing at a statistically significant level.
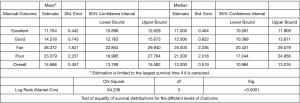
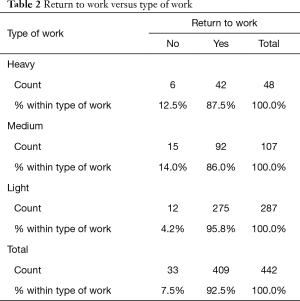
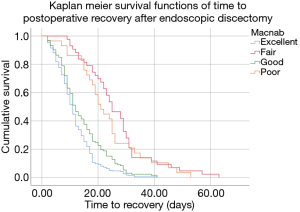
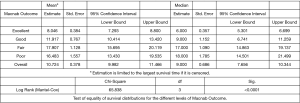
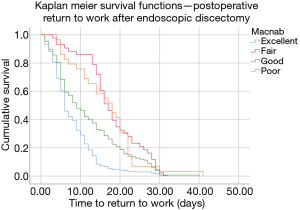
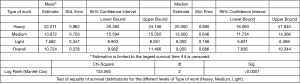
Kaplan Meier (K-M) analysis showed estimated median (50% percentile) RT of 11 days for Excellent, 12 days for Good, 25 days for Fair, and 21 days for Poor Macnab outcomes. The respective estimated RT means are listed in Figure 5. The corresponding K-M survival curves are shown in Figure 6 with the event being patient reporting recovery with narcotic independence and the serial time being the number of days until the event. K-M analysis showed estimated median (50% percentile) RTW of 6 days for Excellent, 9 days for Good, 17 days for Fair, and 18 days for Poor Macnab outcomes. The respective estimated means are listed in Figure 7. The corresponding K-M survival curves are shown in Figure 8 with the event being patient reporting RTW and the serial time being the number of days until the event. K-M analysis of RTW by the type of work (Heavy, Medium, or Light), showed estimated median (50% percentile) RTW of 20 days for in the Heavy, 13 days in the Medium, and 6 days in the Light workgroup. The respective means are listed in Figure 9. The corresponding K-M survival curves are shown in Figure 10 with the event being patient reporting RTW and the serial time being the number of days until the event broken down by the Heavy, Medium, or Light workgroup. The overall estimated median (50% percentile) RTW across all workgroups was 9 days with an overall mean of 10.72 days. One-way ANOVA testing of the RTW and RT times listed in Figure 11 showed statistically significant differences in the mean RT between the Heavy (33.52 days), the Medium (19.17 days), and the Light (9.86 days) workgroups (P<0.0001; Figure 11). A similar analysis of RTW showed statistically significant differences in the mean RTW between the Heavy (22.27 days; P=0.008), the Medium (13.97 days; P=0.004), and the Light (7.58 days; P=0.004) workgroups.
Discussion
Managing preoperative expectations for RT and RTW following spine surgery may be difficult for surgeons who often know little about the actual functional demands required of their patients in the modern workplace. For patients, being able to predict the postoperative course of recuperation is highly relevant to plan for time-off and resources required for rehabilitation, healing, and social reintegration. For employers, accurate estimates of days off work for their employees are essential in reallocating their human resources, to plan for workarounds, and to forecast any potential productivity losses. Traditionally, spine surgery has been associated with long RTs, and cumulative long-term disability with frequent need for additional surgery. The health information provided to patients by the US National Library of Medicine (MedlinePlus) indicates to expect an improvement of symptoms after discectomy or foraminotomy within a few weeks versus 3 to 4 months of recovery after laminectomy and fusion surgery with some symptoms persisting even longer for up to a year (43). This US government website tells patients to expect to be off work after spinal fusion for 4 to 6 weeks if young and healthy and if their job is not very strenuous. Older patients with more extensive spinal fusion surgery are advised that they may have to take 4 to 6 months off before they can get back to work (43). Minimally invasive spinal surgery techniques (MISST) have substantially decreased the burden to patients with faster recovery, less incisional pain, and fewer days to narcotic independence (44).
The authors used RTW and RT as the primary PROM and correlated it with standard clinical outcome measures including the VAS, the Macnab criteria, and postoperative improvement of walking endurance with the expectations that patients would reflect primarily on how they improved from the transforaminal endoscopic decompression surgery in the context of their overall functional demands rather than limiting it to whether or not they returned to work. While the RTW is the most tangible prognosticator of successful clinical outcome (45), it is also the most complex multifactorial problem which is difficult to investigate, particularly if a WC claim is involved. Many of the associated psychosocial factors including inactivity and social isolation from the workplace (46), and financial strain may lead to increased anxiety (47), depression and amplify the negative experience with a physical ailment and thereby produce a lower self-reported health and quality of life assessment unrelated to surgery (48,49).
In the authors’ opinion, reporting RT in addition to RTW time was important to add another accurate measure of disease- and surgery-related recovery since the RTW was reported to be heavily impacted by the preoperative sick leave time (50). The presence of one additional medical co-morbidity was also found to make patients less likely to RTW after surgery. However, co-morbidities were less relevant in our study and did not impact RTW data since the average age was 40.92 years, and the majority of patients were under 40 years of age (Figure 1). Socioeconomic, demographic, and surgical complications were not found to impact RTW data at a statistical significance level (51). One of the strongest positive predictors of RTW after surgery was preoperative work status (51), which was corroborated in our study with the RTW rate for all working patients being 92.5% (409/442). This high RTW rate compared favorably to reported numbers for return to duty in active service members after open decompression (66%) and fusion of 63% (52). Another study including 4694 patients analyzed RTW after traditional open lumbar spine surgery for herniated disc (n=2,437; 52%), lumbar stenosis (n=1,062; 23%), lumbar spondylolisthesis (n=720; 15%), recurrent disc herniation (n=339; 7%), adjacent-segment disease (n=96; 2%), and symptomatic mechanical disc collapse (n=30; 0.6%) (51). The overall RTW three months postoperatively among the 3855 patients who provided RTW information was 82%. An additional work-related factor predictive of lower three-month patient RTW rates is the type of occupation (51). Our results corroborated findings of a previous study (53) reporting statistically significantly lower RTW rates in patients in the Heavy (87.5%) and the Medium (86.0%) workgroups compared to patients in Light (95.8%) workgroups (Table 2).
On the employer’s side, a strong commitment to health and safety, work accommodation, support for the returning worker without disadvantaging other co-workers and supervisors, inclusion of supervisors trained in prevention of work disability during the reintegration of the employee into the workforce (49), contacting the convalescing patient and coordinating RTW (54), and communication of workplace demands by employers with healthcare providers is associated with earlier RTW (45,55). Of the patient- and diagnosis-related factors, preoperative symptom duration of fewer than three months for herniated disc (56) and less than 12 months for spinal stenosis (53) were predictors of better outcomes and earlier RTW (49), compared to the preoperative history of diabetes and higher ASA scores negatively impacting RTW (57). Racial disparities partly related to educational barriers were also reported as relevant (57,58). Of the surgery-related factors, the addition of fusion to the decompression was reported as the most influential predictor of lower RTW rates at three months postoperatively (51). While investigating the impact of this patient-, work-, or diagnosis-related factors was beyond the scope of this study; it is clear that RTW and RT data with the outpatient lumbar endoscopic transforaminal decompression procedures compare favorably to three-months data reported for open or other types of minimally invasive translaminar surgeries (45). The overall RTW rate among the working patients of this study of 92.5% is a testament to the simpler recovery for patients with the outpatient small-incision endoscopic spine surgery. In part, this may be due to fewer postoperative complications (24) and less need for treatment during poorly managed transitions of care episodes due to decompensation of underlying medical co-morbidities which are more likely to lead to readmission (22) and unintended aftercare than surgical site complications (24).
The combined complication rate of 0.7% with the endoscopic transforaminal decompression procedure in this study population was low and approximately one magnitude lower than with microdiscectomy surgeries (24). There were no reherniations causing radiculopathy and was, hence, lower than reported in the literature (16,18,20). Only four patients (0.9%) presented for unintended aftercare due to an emergency room. The readmission rate of 0.45% (22) was low compared to microdiscectomy studies (18), and there were no re-incisions for any follow-up surgeries within 90 days. Failure to cure with Poor Macnab outcomes and without improvement of postoperative walking endurance occurred in 6.6% (29/442) of patients with bony stenosis in the central canal, lateral recess, and entry zone of the foramen. In these failed patients, the endoscopic decompression technology may have been inadequate to deal with the extent of the stenosis or the underlying disease process was most likely too advanced. The most common postoperative sequela (15.38%) by far was irritation of the DRG which delayed RTW to a mean of 18.94 days (P<0.0001) and RT (P<0.001) to 15.31 days with statistical significance in patients with Heavy jobs. Most postoperative problems, whether complication or sequelae, were handled on an outpatient basis in an office setting (24).
The Kaplan-Meier analysis of the time to RTW and RT was in the authors’ opinion more appropriate for graphically illustrating the RTW and RT dynamic in patients who underwent the endoscopic transforaminal decompression procedure than merely reporting the mean RTW and RT times. The non-continuous nature of the K-M survival plots provide step-wise survival estimates until the event which in the case of the authors’ study was the number of days when the patient reported either RTW or complete recovery as defined by narcotic independence. K-M curves are not a smooth function. Calculating exact survival points for the RTW and RT is actually quite tricky and depends on the number of positive and negative factors leading to the censoring of study patients with an event throughout the study or at its end without event. Since the author had no way to include additional workplace-related data into crosstabulation statistics, the K-M curves graphically represent the real postoperative RTW and RT dynamic reported by patients. For the vast majority of patients who were in the Light workgroup the K-M curve demonstrate that many patients returned much sooner to work left to the 50% percentile (median six days) than to the right of it (Figure 10). The vast majority of patients had Excellent and Good Macnab outcomes (83.7%; 370/442). K-M curves indicate very favorable RTW and RT times with 50% of patients (left to the 50% percentile median point) having achieved narcotic independence and returned to work within six days (Excellent Macnab outcome), or nine days (Good Macnab outcomes). However, K-M curves have to be cautiously evaluated since they become an estimate after the first patient has been censored. Therefore, the K-M curves showed an accurate graphic representation of the RTW and RT times until the first patient was censored. At that point, it is an estimation and extrapolations on future RTW, RT, and patient outcomes should be avoided. Based on the K-M analysis, this team of authors concluded that surgical treatment of sciatica symptoms due to contained lumbar herniated disc with the transforaminal endoscopic decompression allows the vast majority (83.7%) to RTW and achieve narcotic dependence in less than ten days postoperatively.
This study had several limitations. Many variables previously reported to impact RTW (51) (i.e., marital status, family support, preoperative disposition of wanting to work, working conditions, employer-employee relationship, work-related stress) were not recorded and, hence, are missing in this RTW and RT discussion after endoscopic spine surgery for symptomatic lumbar contained herniated disc with or without associated spinal stenosis. In comparison to predictive RTW model reports (59,60), the authors of this study did not intend to perform an in-depth RTW analysis but to illustrate shorter RTW and RT times in the immediate three-months postoperative recovery period following the outpatient lumbar endoscopic transforaminal decompression procedure with simple PROMs such as VAS, Macnab, and walking endurance to the pain limit. Additional limitations may have existed since the authors did not attempt to ascertain whether RTW reported by patients postoperatively were at the same work- or functional capacity level. However, the latter problem may be of lesser relevance to employers who are predominately interested in knowing when their employees are returning to the same job duties they held before their spine surgery.
Conclusions
RTW and RT with narcotic independence following an endoscopic transforaminal decompression surgery for sciatica-type low back, and leg pain due to contained lumbar herniated disc is on the order of 10 days or less in the vast majority of patients. The most relevant surgical predictor of delayed RTW and RT is a postoperative DRG irritation which predominantly affects patients in the Medium and Heavy workgroups. Low complication-, readmission-, and re-incision rates indicated that this outpatient surgery is associated with more straightforward recovery for the patient and with fewer postoperative unintended aftercare than with traditional translaminar open spine surgery. RTW rates (92.5%) are higher than those reported with traditional open and other types of minimally invasive translaminar decompression surgeries. Surgical translational outcome research should focus on analyzing the effectiveness of state-of-the-art endoscopic surgery interventions for herniated disc and stenosis in the lumbar spine to further determine how they impact the prognosis of RTW and RT in the surgical treatment of neurogenic claudication and lumbar radiculopathy.
Acknowledgments
None.
Footnote
Conflicts of Interest: The authors have no direct (employment, stock ownership, grants, patents), or indirect conflicts of interest (honoraria, consultancies to sponsoring organizations, mutual fund ownership, paid expert testimony). The authors are not currently affiliated with or under any consulting agreement with any vendor that the clinical research data conclusion could directly enrich. This manuscript is not meant for or intended to endorse any products or push any other agenda other than to report the return to work data and the associated clinical outcomes. The motive for compiling this clinically relevant information is by no means created and/or correlated to directly enrich anyone due to its publication. This publication was intended to substantiate contemporary endoscopic spinal surgery concepts to facilitate technology advancements.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. IRB approval was obtained for this study (CEIFUS 106-19). Written informed consent was obtained from the patient for publication of this Original Study and any accompanying images. A copy of the written consent is available for review by the Editor-in-Chief of this journal.
References
- Campbell P, Wynne-Jones G, Muller S, et al. The influence of employment social support for risk and prognosis in nonspecific back pain: a systematic review and critical synthesis. Int Arch Occup Environ Health 2013;86:119-37. [Crossref] [PubMed]
- Carroll C, Rick J, Pilgrim H, et al. Workplace involvement improves return to work rates among employees with back pain on long-term sick leave: a systematic review of the effectiveness and cost-effectiveness of interventions. Disabil Rehabil 2010;32:607-21. [Crossref] [PubMed]
- Clay FJ, Newstead SV, McClure RJ. A systematic review of early prognostic factors for return to work following acute orthopaedic trauma. Injury 2010;41:787-803. [Crossref] [PubMed]
- Dick FD, Graveling RA, Munro W, et al. Workplace management of upper limb disorders: a systematic review. Occup Med (Oxf) 2011;61:19-25. [Crossref] [PubMed]
- Franche RL, Cullen K, Clarke J, et al. Workplace-based return-to-work interventions: a systematic review of the quantitative literature. J Occup Rehabil 2005;15:607-31. [Crossref] [PubMed]
- Hansson T, Jensen I. Swedish Council on Technology Assessment in Health Care (SBU). Chapter 6. Sickness absence due to back and neck disorders. Scand J Public Health Suppl 2004;63:109-51. [Crossref] [PubMed]
- Heymans MW, van Tulder MW, Esmail R, et al. Back schools for nonspecific low back pain: a systematic review within the framework of the Cochrane Collaboration Back Review Group. Spine 2005;30:2153-63. [Crossref] [PubMed]
- Hlobil H, Staal JB, Spoelstra M, et al. Effectiveness of a return-to-work intervention for subacute low-back pain. Scand J Work Environ Health 2005;31:249-57. [Crossref] [PubMed]
- Anderson JT, Tye EY, Haas AR, et al. Multilevel Lumbar Fusion Is a Risk Factor for Lower Return to Work Rates Among Workers' Compensation Subjects With Degenerative Disc Disease. J Surg Orthop Adv 2018;27:209-18. [PubMed]
- Liow MHL, Goh GS, Yeo W, et al. Time Taken to Return to Work Does Not Influence Outcomes of Minimally Invasive Transforaminal Lumbar Interbody Fusion: A 5-Year Follow-Up Study. Spine (Phila Pa 1976) 2019;44:503-9. [Crossref] [PubMed]
- Huysmans E, Goudman L, Van Belleghem G, et al. Return to work following surgery for lumbar radiculopathy: a systematic review. Spine J 2018;18:1694-714. [Crossref] [PubMed]
- Anderson JT, O'Donnell JA, Haas AR, et al. Lumbar Discography Is Associated With Poor Return to Work Status Following Lumbar Fusion Surgery in a Workers' Compensation Setting. J Surg Orthop Adv 2018;27:25-32. [PubMed]
- Lewandrowski KU. “Outside-in” technique, clinical results, and indications with transforaminal lumbar endoscopic surgery: a retrospective study on 220 patients on applied radiographic classification of foraminal spinal stenosis. Int J Spine Surg 2014. [Crossref] [PubMed]
- Yeung AT, Yeung CA. Minimally invasive techniques for the management of lumbar disc herniation. Orthop Clin North Am 2007;38:363-72. [Crossref] [PubMed]
- Tsou PM, Alan Yeung C, Yeung AT. Posterolateral transforaminal selective endoscopic discectomy and thermal annuloplasty for chronic lumbar discogenic pain: a minimal access visualized intradiscal surgical procedure. Spine J 2004;4:564-73. [Crossref] [PubMed]
- Tsou PM, Yeung AT. Transforaminal endoscopic decompression for radiculopathy secondary to intracanal noncontained lumbar disc herniations: outcome and technique. Spine J 2002;2:41-8. [Crossref] [PubMed]
- Yeung AT, Yeung CA. Advances in endoscopic disc and spine surgery: foraminal approach. Surg Technol Int 2003;11:255-63. [PubMed]
- Debono B, Sabatier P, Garnault V, et al. Outpatient Lumbar Microdiscectomy in France: From an Economic Imperative to a Clinical Standard—An Observational Study of 201 Cases. World Neurosurg 2017;106:891-97. [Crossref] [PubMed]
- Yeung AT. Lessons Learned from 27 Years’ Experience and Focus Operating on Symptomatic Conditions of the Spine under Local Anesthesia: The Role and Future of Endoscopic Spine Surgery as a “Disruptive Technique” for Evidenced Based Medicine. J Spine 2018;7:413. [Crossref]
- Hersht M, Massicotte EM, Bernstein M. Patient satisfaction with outpatient lumbar microsurgical discectomy: a qualitative study. Can J Surg 2007;50:445-9. [PubMed]
- Brox JI, Storheim K, Grotle M, et al. Systematic review of back schools, brief education, and fear-avoidance training for chronic low back pain. Spine J 2008;8:948-58. [Crossref] [PubMed]
- Lewandrowski KU. Readmissions After Outpatient Transforaminal Decompression for Lumbar Foraminal and Lateral Recess Stenosis. Int J Spine Surg 2018;12:342-51. [Crossref] [PubMed]
- Lewandrowski KU. Successful outcome after outpatient transforaminal decompression for lumbar foraminal and lateral recess stenosis: The positive predictive value of diagnostic epidural steroid injection. Clin Neurol Neurosurg 2018;173:38-45. [Crossref] [PubMed]
- Lewandrowski KU. Incidence, Cost, and Management of Complications After Transforaminal Endoscopic Decompression Surgery For Lumbar Foraminal And Lateral Recess Stenosis: A Value Proposition For Outpatient Ambulatory Surgery. Int J Spine Surg 2019;13:53-67. [Crossref] [PubMed]
- Lewandrowski KU. Retrospective analysis of accuracy and positive predictive value of preoperative lumbar MRI grading after successful outcome following outpatient endoscopic decompression for lumbar foraminal and lateral recess stenosis. Clin Neurol Neurosurg 2019;179:74-80. [Crossref] [PubMed]
- Botwin KP, Gruber RD, Bouchlas CG, et al. Fluoroscopically guided lumbar transformational epidural steroid injections in degenerative lumbar stenosis: an outcome study. Am J Phys Med Rehabil 2002;81:898-905. [Crossref] [PubMed]
- el-Khoury GY, Ehara S, Weinstein JN, et al. Epidural steroid injection: a procedure ideally performed with fluoroscopic control. Radiology 1988;168:554-7. [Crossref] [PubMed]
- Bogduk N, Aprill C, Derby R. Epidural spinal injections. In: White AH, Schollerman J. editors. Spinal Care: Diagnosis and Treatment. Mosby, 1995:322-43.
- Huskisson EC, Jones J, Scott PJ. Application of visual-analogue scales to the measurement of functional capacity. Rheumatol Rehabil 1976;15:185-7. [Crossref] [PubMed]
- Lee IS, Kim SH, Lee JW, et al. Comparison of the temporary diagnostic relief of transforaminal epidural steroid injection approaches: conventional versus posterolateral technique. AJNR Am J Neuroradiol 2007;28:204-8. [PubMed]
- Macnab I. Negative disc exploration. An analysis of the causes of nerve-root involvement in sixty-eight patients. J Bone Joint Surg Am 1971;53:891-903. [Crossref] [PubMed]
- Lee CK, Rauschning W, Glenn W. Lateral lumbar spinal canal stenosis: classification, pathologic anatomy, and surgical decompression. Spine (Phila Pa 1976) 1988;13:313-20. [Crossref] [PubMed]
- Lee S, Kim SK, Lee SH, et al. Percutaneous endoscopic lumbar discectomy for migrated disc herniation: classification of disc migration and surgical approaches. Eur Spine J 2007;16:431-7. [Crossref] [PubMed]
- Hasegawa T, An HS, Haughton VM, et al. Lumbar foraminal stenosis: critical heights of the intervertebral discs and foramina. A cryomicrotome study in cadavera. J Bone Joint Surg Am 1995;77:32-8. [Crossref] [PubMed]
- Hoogland T, Schubert M, Miklitz B, et al. Transforaminal posterolateral endoscopic discectomy with or without the combination of a low-dose chymopapain: a prospective randomized study in 280 consecutive cases. Spine (Phila Pa 1976) 2006;31:E890-7. [Crossref] [PubMed]
- Schubert M, Hoogland T. Endoscopic transforaminal nucleotomy with foraminoplasty for lumbar disk herniation. Oper Orthop Traumatol 2005;17:641-61. [Crossref] [PubMed]
- Adopted from U.S. Department of Labor, Dictionary of occupational titles (Washington, D.C.: U.S. Government Printing Office), 2019.
- Åstrand PO, Rodahl K, Dahl HA, et al. Textbook of Work Physiology: Physiological Bases of Exercise, Human Kinetics. 1970, MacGraw-Hill.
- Sharkey BJ, Davis PO. Hard work; defining physical work performance requirements. Human Kinetics Pub 2008, pp 3-11. ISBN-13: 978-0736065368, ISBN-10: 0736065369.
- Passmore RR, Durnin JVGA. Human Energy Expenditure 01 OCT 1955. Available online: https://doi.org/ [Crossref]
- Roos EM, Boyle E, Frobell RB, et al. It is good to feel better, but better to feel good: whether a patient finds treatment ‘successful’ or not depends on the questions researchers ask. Br J Sports Med 2019. [Epub ahead of print]. [Crossref] [PubMed]
- Altman DG, Machin D, Bryant TN, et al. 2000. Statistics with Confidence: Confidence Intervals and Statistical Guidelines, 2nd ed. BMJ Books. Available online: https://www.wiley.com/en-us/Statistics+with+Confidence%3A+Confidence+Intervals+and+Statistical+Guidelines%2C+2nd+Edition-p-9780727913753
- Spine surgery - discharge. US National Library of Medicine. MedlinePlus. Trusted Health Information for You. Available online: .https://medlineplus.gov/ency/patientinstructions/000313.htm
- Wang X, Borgman B, Vertuani S, et al. A systematic literature review of time to return to work and narcotic use after lumbar spinal fusion using minimal invasive and open surgery techniques. BMC Health Serv Res 2017;17:446. [Crossref] [PubMed]
- Cancelliere C, Donovan J, Stochkendahl MJ, et al. Factors affecting return to work after injury or illness: best evidence synthesis of systematic reviews. Chiropractic & Manual Therapies 2016;24:32. [Crossref] [PubMed]
- Hoffman BM, Papas RK, Chatkoff DK, et al. Meta-analysis of psychological interventions for chronic low back pain. Health Psychol 2007;26:1-9. [Crossref] [PubMed]
- Iles RA, Davidson M, Taylor NF. Psychosocial predictors of failure to return to work in non-chronic non-specific low back pain: a systematic review. Occup Environ Med 2008;65:507-17. [Crossref] [PubMed]
- Kent PM, Keating JL. Can we predict poor recovery from recent-onset nonspecific low back pain? A systematic review. Man Ther 2008;13:12-28. [Crossref] [PubMed]
- Lee YP, Farhan SD, Kiester D, et al. Variables Affecting Return to Work After Spinal Surgery in a Non-workers' Compensation Population: A Retrospective Cohort Study. J Am Acad Orthop Surg 2017;25:e282-8. [Crossref] [PubMed]
- Andersen MØ, Ernst C, Rasmussen J, et al. Return to work after lumbar disc surgery is related to the length of preoperative sick leave. Dan Med J 2017;64:A5392. [PubMed]
- Asher AL, Devin CJ, Archer KR, et al. An analysis from the Quality Outcomes Database, Part 2. Predictive model for return to work after elective surgery for lumbar degenerative disease. J Neurosurg Spine 2017;27:370-81. [Crossref] [PubMed]
- Lunsford JG, Lawson BK, Johnson AE, et al. Return to Duty Rates in Active Duty Service Members After Elective Surgery of the Lumbar Spine. Mil Med 2016;181:572-6. [Crossref] [PubMed]
- Radcliff KE, Rihn J, Hilibrand A, et al. Does the duration of symptoms in patients with spinal stenosis and degenerative spondylolisthesis affect outcomes?: analysis of the Spine Outcomes Research Trial. Spine (Phila Pa 1976) 2011;36:2197-210. [Crossref] [PubMed]
- Charles C, Gafni A, Whelan T. Shared decision-making in the medical encounter: what does it mean? (or it takes at least two to tango). Soc Sci Med 1997;44:681-92. [Crossref] [PubMed]
- Kuijer W, Groothoff JW, Brouwer S, et al. Prediction of sickness absence in patients with chronic low back pain: a systematic review. J Occup Rehabil 2006;16:439-67. [Crossref] [PubMed]
- Grøvle L, Haugen AJ, Keller A, et al. Prognostic factors for return to work in patients with sciatica. Spine J 2013;13:1849-57. [Crossref] [PubMed]
- Graver V, Ljunggren AE, Loeb M, et al. Background variables (medical history, anthropometric and biological factors) in relation to the outcome of lumbar disc surgery. Scand J Rehabil Med 1998;30:221-5. [Crossref] [PubMed]
- Skinner J, Weinstein JN, Sporer SM, et al. Racial, ethnic, and geographic disparities in rates of knee arthroplasty among Medicare patients. N Engl J Med 2003;349:1350-9. [Crossref] [PubMed]
- Papić M, Brdar S, Papić V, et al. Return to Work After Lumbar Microdiscectomy - Personalizing Approach Through Predictive Modeling. Stud Health Technol Inform 2016;224:181-3. [PubMed]
- Than KD, Curran JN, Resnick DK, et al. How to predict return to work after lumbar discectomy: answers from the NeuroPoint-SD registry. J Neurosurg Spine 2016;25:181-6. [Crossref] [PubMed]