- 1Department of Orthopaedics, Tianjin Medical University General Hospital, Tianjin, China
- 2F.M. Kirby Neurobiology Center, Boston Children's Hospital and Department of Neurology, Harvard Medical School, Boston, MA, United States
Background: Spinal cord injury (SCI) is a severe condition that disrupts patients' physiological, mental, and social well-being state and exerts great financial burden on patients, their families and social healthcare system. This review intends to compile studies regarding epidemiological features of SCI in China.
Methods: Searches were conducted on PubMed, EMBASE, Web of Science and Cochrane Library for relevant studies published through January, 2018. Studies reported methodological and epidemiological data were collected by two authors independently.
Results: Seventeen studies met the inclusion criteria. Two studies reported incidence of SCI that is 60.6 in Beijing (2002) and 23.7 in Tianjin (2004–2008). All studies showed male had a larger percentage in SCI compared to female except Taiwan (2000–2003). The average male and female ratio was 3–4:1 in China and the highest male and female ratio was 5.74: 1 in Tianjin (2004–2007). Farmers, laborers and unemployed people accounted for more than half of the SCI patients in China. Fall was the primary causation with exception of Heilongjiang (2009–2013), Beijing (2001–2010), and Taiwan (2002–2003), where motor vehicle collision (MCVs) was the leading causation. Pulmonary infection, urinary tract infection and bedsore were common complications, accounting for approximately 70% of SCI patients in China.
Conclusion: This review shows that epidemiological features of SCI are various in different regions in China and prevention should be implemented by regions. The number of patients with SCI result from fall and MCVs may become a main public health problem because population aging and economic developing in China. However, because all included studies were retrospective and lacking a register system in China, some data were incomplete and some cases may be left out, so the conclusion may not be generalizable to the other regions.
Background
Spinal cord injury (SCI) is a devastating lesion, resulting in motor and sensory deficit and ultimately exerts impact on patient's physiological, mental and social well-being state (1, 2). Due to no effective treatment is available for SCI, unfortunately, SCI patients have to take substantial financial burden for their treatment and healthcare rehabilitation. Meanwhile, the incidence of SCI is rising worldwide with annual estimated incidence at 10.4–83 cases per million even though prevention measures have been taken to lower the occurrence (3, 4). The incidence of SCI range from 20.7 to 83.0 in North American and 8.0 to 130.6 in Europe per million annually (5, 6). Research have reported the incidence of SCI ranged between 10.6 and 22.6 per million in Québec, Canada (2000–2011) (7) and its annual costs was 2.67 billion dollars. In Denmark (1990–2012) (8) the incidence was 10.2 per million. And in Finland (2012–2013) (9) was 25.1–38.1 per million and 21.0–32.3 per million in Australia (1921–2011) (10). It has been estimated the costs of SCI in Australia annually to be almost 2 billion Australian dollars in total (11). In Japan, it has been reported the incidence of SCI was 121.4 per million in 2011 and 117.1 in 2012 (12). The financial burden of SCI includes rehabilitation services, expensive personal assistance, lost productivity for disability and social isolation. Studies have revealed the high incidence and heavy economic impact of SCI in developed countries.
As the largest developing country with approximately 25% of the global population, China has a large number of SCI patients. Unfortunately, little was known about the epidemiological features especially incidence and prevalence of SCI (13). Given the increasing life expectancy people with SCI are experiencing from 69 years in 1990 to nearly 75 years (14), prevention strategies and post-injury rehabilitation is crucial (15). Reliable epidemiological data and evidence of SCI in China are vital for estimating the number of patients, finding out the main causes, developing interventions, providing up-to-date information, and raising public awareness. Previous studies have reported the incidence of SCI in China increased significantly (16). Therefore, it is of great significance to review all the research data of SCI in China to attain a comprehensive understanding of its epidemiological features so as to improve management and reduce the financial burden on patients and healthcare system.
This review intends to compile the studies regarding epidemiological features of SCI published through January, 2018 in four directly governed cities–Beijing, Tianjin, Shanghai and Chongqing, and four provinces–Heilongjiang, Anhui, Guangdong and Taiwan. It will provide an updated overview for the epidemiological profile and give an insight into current situation of SCI in China. This can help us better carry out prevention strategies and effective allocate medical resources.
Methods
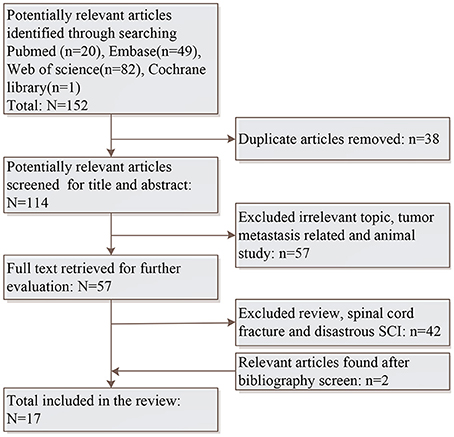
Searches were conducted on PubMed, EMBASE, Web of Science and Cochrane Library for potentially relevant studies without language and date restrictions. The keywords and phrases applied for this search were “spinal cord injury,” “traumatic spinal cord injury,” “epidemiology,” and “China.” Bibliographies of included studies were also systematically screened to identify further relevant studies which were not included in the searched electronic databases. Case reports and conference abstracts were excluded. Figure 1 displays the search strategy and screen procedure in details.
Titles and abstracts were identified by two independent reviewers and were categorized by the previous inclusion criteria. The eligible inclusion criteria were presented as follow: (1) original study concerning SCI or TSCI; (2) studies provide relevant epidemiological data; (3) original data were collected from hospital. Results extraction was also conducted by two independent reviewers and all discrepancy were settled by discussing with a third reviewer. From included studies, methodological information and epidemiological data were collected: region, source population, incidence period, case criteria, study type (prospective or retrospective), total number of patients, incidence, causation, male and female ratio, mean age, age with peak incidence, age span, patients' occupation, injury level, injury extent, America Spinal Injury Association Impairment Scale (AIS) grade. Additionally, complication and treatment were extracted.
Results
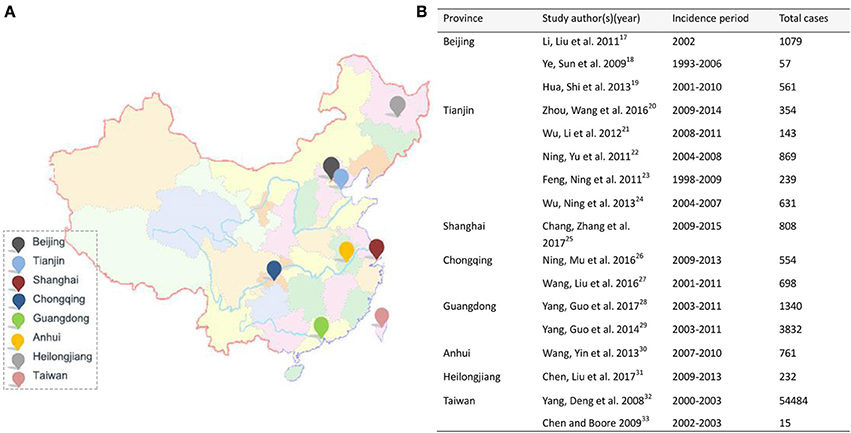
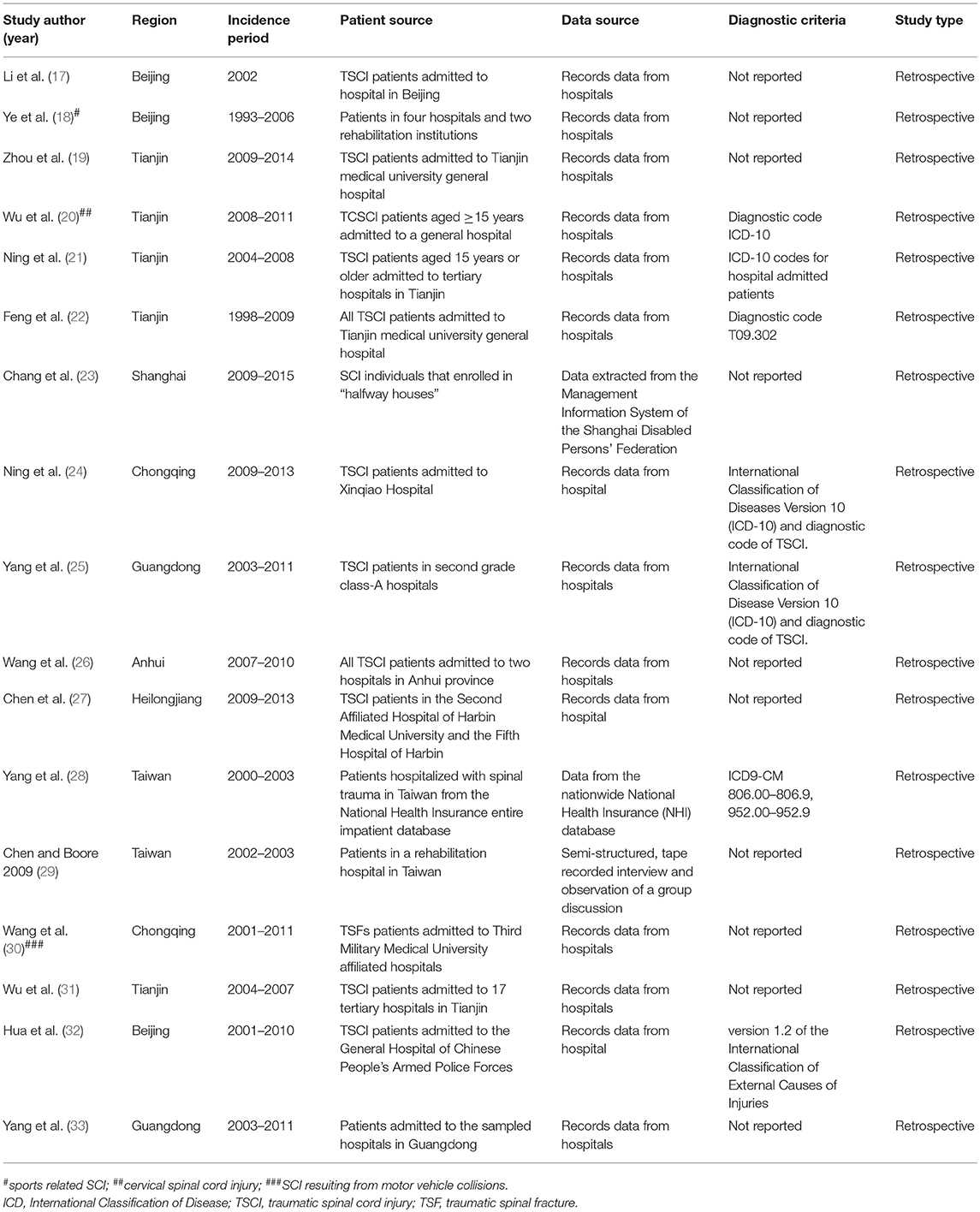
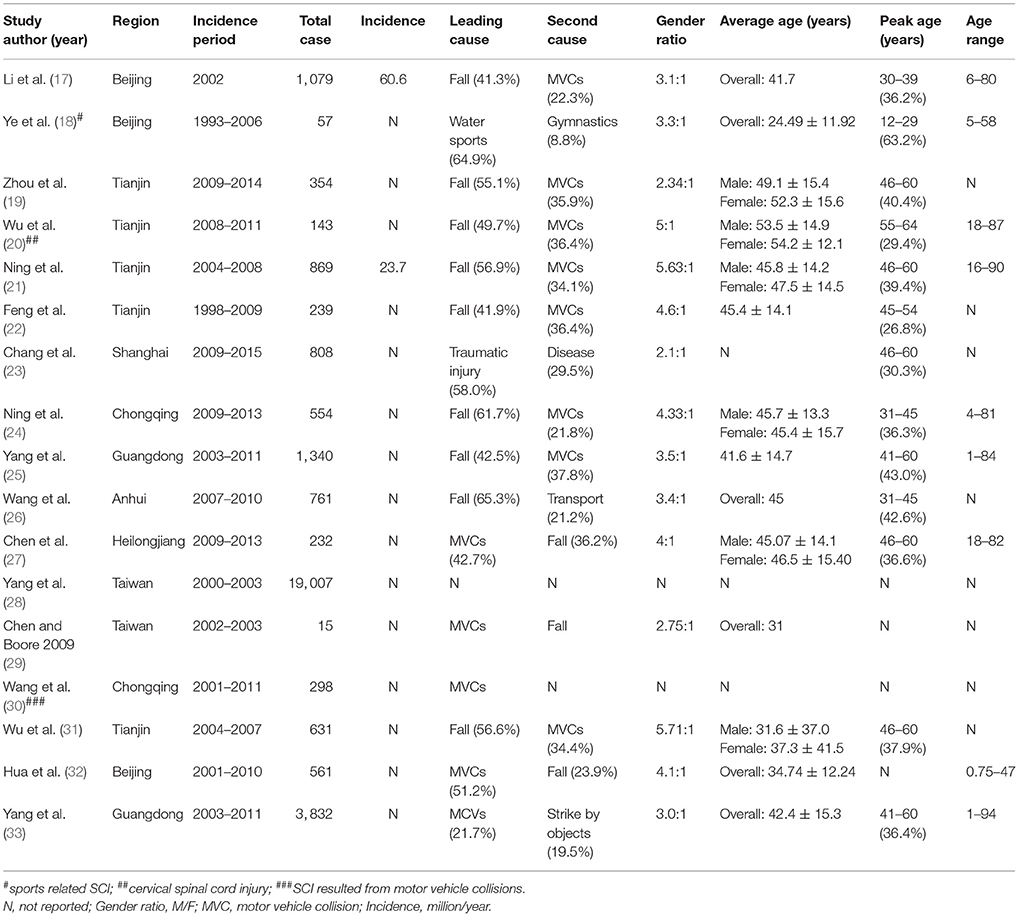
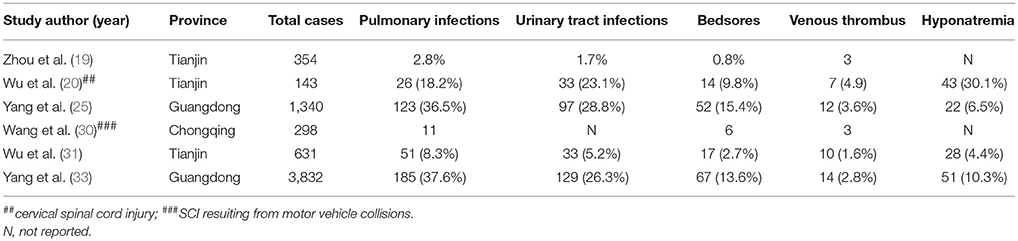
Total 152 potentially relevant studies were identified initially and 15 met the inclusion criteria. After systematically screening bibliographies of included studies, two additional were added. Therefore, a total of 17 studies were included finally. The epidemiological features of eight regions (Figure 2) were reported. Table 1 displays region, patient source, incidence periods, diagnostic criteria and study type, and number of patients, incidence, causation, male and female ratio, average age, peak incidence age and age span were listed in Table 2. Table 3 summarizes the occupation, causation, level of injury, ASI degree and treatment. Tables 4–8 present causation, occupation, segments, severity and complication, respectively.
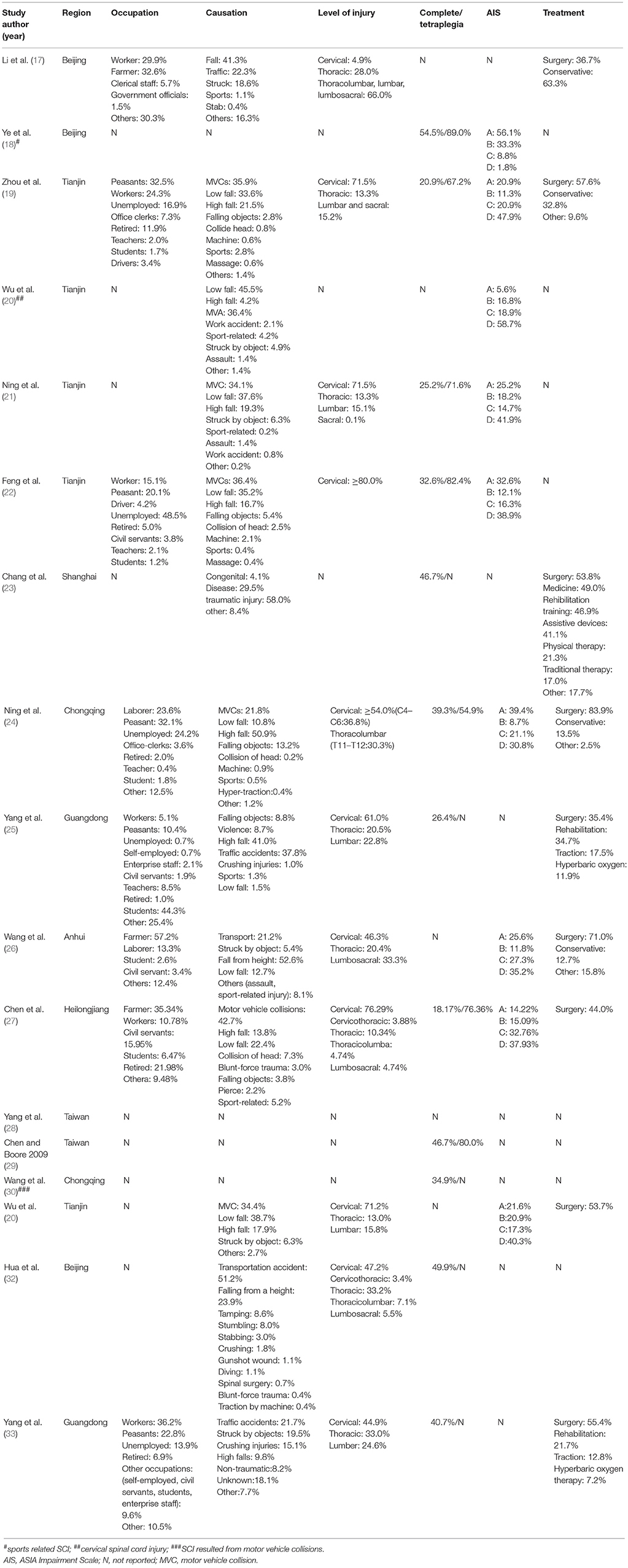
Table 3. Occupation, causation, level and extent of injury, AIS and treatment of spinal cord injury in China.
Incidence, Gender, and Age
In this review, only two studies reported incidence of SCI, in Beijing (2002) and Tianjin (2004–2008), which is 60.6 and 23.7 per million, respectively (17, 21). Totally 1,948 cases was included. We found incidence varied significantly, the highest was 60.6 in Beijing, which was approximately three times as much as Tianjin (2004–2008).
All studies showed male had a larger percentage of SCI compared to female The male and female ratio ranged significantly across regions, with the highest ratio was 5.71: 1 in Tianjin (2004–2007) (31). In Tianjin (2004–2008, 5.63:1; 2008–2011, 5:1), male and female ratio was high, while in Shanghai (2009–2015), male and female ratio was 2.1:1, which was ralitively lower than other regions. And in China the average male: female ratio was 3–4:1.
As expected, the mean age was range from 30 to 50 typically, the average age of male was slightly younger than that of female among reported studies except Chongqing (2009–2013) (24), where male and female had an average age of 45.7 and 45.4, respectively. Age with peak incidence ranged from 40 to 60 years. However, Beijing (2002) had a relative lower age of peak incidence which was 30–39 years of age (17). Both Chongqing (2009–2013) and Anhui (2007–2010) had a peak incidence aged 31–45 years (24, 26). The age span ranged a broader spectrum, the youngest was 9 months in Beijing (2001–2010) while the oldest was 90 years in Tianjin (2004–2008) (21, 32).
Occupations
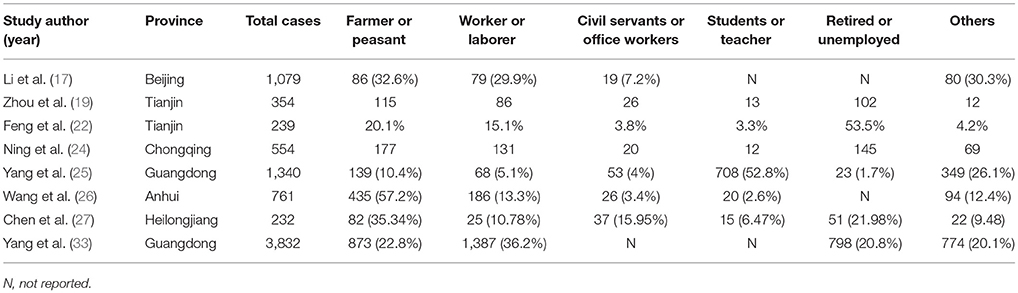
As shown in Table 5, the occupations of SCI patients varied including the farmers, laborers, civil servants, office clerks, students, teachers, retired, unemployed and others. Classification of their occupations on the basis of their workplace. It was evident that farmers, laborers and unemployed people had a higher risk of SCI. These three groups accounted for more than half of the patients with SCI. In Beijing (2002) and Anhui (2007–2010), manual workers like farmers and peasants have a high ricks than Guangdong (2003–2011) and Heilongjiang (2009–2013). Surprisingly, teachers (8.5%) and students (44.3%) with SCI in Guangdong (2003–2011) outnumbered peasants (10.4%) and workers (5.1%) (25). Additionally, retired people with SCI taken up a large percentage in Heilongjiang (2009–2013: 21.98%), which exceeded the number of workers (10.78%) (27).
Causes
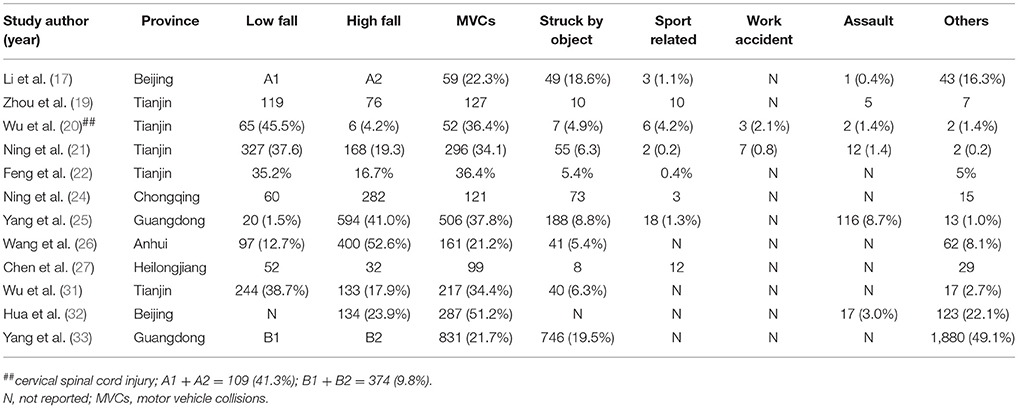
With respect to causes of SCI, this study summarized the common cause in Table 4. Motor vehicle collisions (MCVs), high and low fall, struck by falling object, sports related activities, violence such as gunshot and stab, work related accidents, crushing injuries and blunt force trauma, others such as massage and collision of head. Among all these causes, fall including high and low fall were the primary causation, with the exception of few regions, such as Heilongjiang (2009–2013), Beijing (2001–2010), and Taiwan (2002–2003), where MCVs was the leading causes typically (27, 29, 32). The percentage of spinal cord injuries caused by struck by falling object was relative high in Guangdong (2003–2011, 19.5%), Beijing (2002, 18.6%), and Chongqing (2009–2013, 13.2%) than other regions (17, 24, 33). In Guangdong, however, injuries caused by violence taken up a larger percentage (8.7%). Details of sports and work related SCI was only reported in a few studies.
Level and Severity
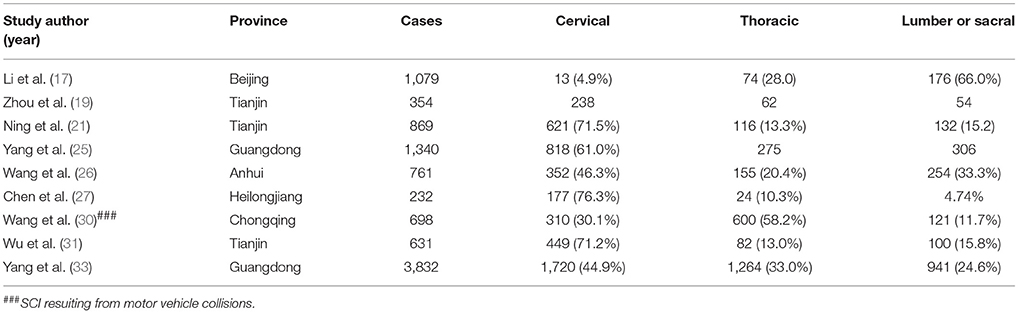
Tables 6,7 present the injury level of SCI. Cervical spinal cord injuries taken up 45–70% in most regions, with the exception of Beijing (2002, cervical: 4.9%) (17), and the most common anatomical level was C4–C6. In Beijing (2002), the proportion of low level SCI like thoracolumbar, lumbar and lumbosacral injury was 66.0%, which is much higher than cervical (4.9%) and thoracic (28.0%) injury.. In addition, some patients injuried more than one level of spinal cord in Heilongjiang (2009–2013), where people subjected to cervicothoracic (3.88%), thoracicolumbar (4.74%) and lumbosacral (4.74%) injury (27).
The severity of SCI is measured by neurological degree (tetraplegia and paraplegia) and extent (complete and incomplete). In the present review, 6 studies reported degree and 11 studies reported extent. Tetraplegia injury had a large proportion than paraplegia in all included studies and the proportion of tetraplegia patients ranged between 54.9 and 89.0%. The largest proportion was in Beijing (1993–2006) and smallest in Chongqing (2009–2013), respectively (18, 24). Regarding extent of injuries, the proportion of complete injuries varied from 18.17 to 54.5% and the percentage of incomplete injuries great than complete injuries. In Beijing (1993–2006), the occurrence of tetraplegia and complete injury was much higher than Chongqing (2009–2013), Guangdong (2003–2011) and Heilongjiang (2009–2013).
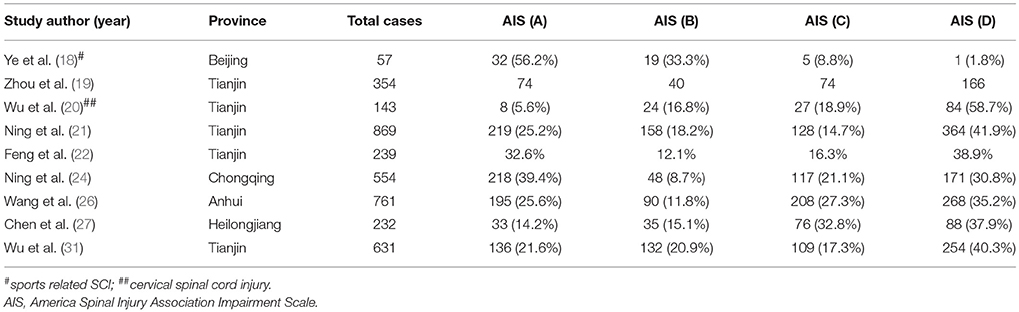
The AIS grade was reported in 9 studies. In included studies, most patients were grade D except Beijing (1993–2006) and Chongqing (2009–2013) (18, 24), which grade A was the most. In Beijing (1993–2006), grade A patients accounted for 56.1%, which was higher than that in Chongqing (2009–2013). Patients of grade B and grade C maintained a middle position, constituted approximately 10–40% combined.
Seven studies reported the number of death. Tianjin (2008–2011) had high death rate (4.2%) among all regions (20). Patients aged over 60 and with complications are more vulnerable to death during their hospitalization.
Clinical Complications and Treatment
In this review, six studies reported clinical complications in Table 8. Pulmonary infection, urinary tract infection and bedsore are the most common complications which was approximately 70%, followed by deep venous thrombosis and electrolyte disturbance. Surprisingly, patient with hyponatremia in Tianjin (2008–2011) was 30.1%, which was nearly twice as much as patients with respiratory infection (18.2%) (20). In Guangdong (2003–2011), rare complications were reported, such as urinary calculus (0.3%), spasms (0.3%), and autonomic dysreflexia (0.9%) (25).
The main treatment for SCI was surgery, including decompression and internal fixation or fuse. In the included studies, more than half of the SCI patients received surgery. Nevertheless, a larger proportion of patients (63.3%) in Beijing (2002) received conservative treatment than surgery (36.7%) (17). In addition, a much larger percentage of patients in Guangdong (2003–2011, 34.7%) received rehabilitation than other regions in China (25). Rehabilitation strategy including braces can be used to practice standing and walking, and other special tools, such as walking aids, can be provided to compensate for the lack of moter funcion.
Discussion
SCI impairs the physical, metal, and social well-being state of patients and exerts heavy financial burden on national healthcare system, patients and their families. A thorough understanding of SCI epidemiological profile helps national healthcare system carry out preventative strategies better and allocate medical resource reasonablely. Also, a comparison between different cities and provinces can shed light on how to effectively tackle these issues in the process of implementing prevention measures.
Many studies of SCI were carried out in developed nations, especially in America, Canada and Australia. Developing countries, however, with approximately 80% population throughout the world, lack related data because a national register system for SCI has not been established yet. To the best of our knowledge, several reviews of SCI in China have been reported. In China, it is difficult to estimate incidence because universal diagnostic criteria and national register system were not established. In this study, only 2 studies reported estimated incidence. In 2002, the incidence in Beijing was 60.6 per million, while it was 23.7 per million in Tianjin (2004–2008) (21, 28). Studies in China used various inclusion criteria, so the incidence varied significantly. In developed countries, the annual incidence was 20.7–83 per million in America and 8.0–130.6 in Europe (34). This indicate the incidence of SCI in China was similar with developed countries. And other studies have reported developing regions had lower incidence compared to developed countries (35) and such difference might due to the development level of society and economy. In Europe and American, people are more likely to participate in risky activities like housing riding, rugby and skiing and these are high risk factors of SCI. In China, ages with peak incidence is different from other countries. Ages with peak incidence was varied from 30 to 60 years, while it was 20–29 in Aragon, Spain (1972–2008) and 16–31 in Thessaloniki, Greece in 2006 (36, 37). In Beijing (1993–2006), peak age of patient was 12–29, which is younger than other studies because it focud on sports related SCI and most athletes were young people. In addition, the mean age of SCI in North America was range from 32 to 55.4 years (38), and it was between 37 and 47.9 in Europe (39). This was in consistence with mean age in China, which is from 30 to 50. Demographic structure is a main factor to explain varied ages with peak incidence across different countries. In China, the ratio of old people is increasing dramatically. It has been predicted individual aged over 60 could be 438 million by 2050 (40). Old people are more vulnerable to SCI due to degeneration of vertebrae and deterioration of physical conditions, so prevention is of great importance. The elderly should aware of the potential risks and take precautionary measures, such as do not do strenuous exercise and go to hospital regularly for physical examinations.
Most studies showed that male were at higher risk of SCI than female (41, 42), these results were in accordance with present study in China. The ratio up to 5.71:1 in Tianjin (2004–2207). This was ascribed to the Chinese traditional cultural backgrounds. Male are major sources of household income and take the responsibility to support their families while female have to stay at home and take care of children. Meanwhile, male are the main labor resources and productive group of society and many engage in manual work. Thus, a large number of male work on high risk industry and thay are more likely to be exposed to risky environment, such as industrial construction sites. However, with the progress of society, more female are taking high risk occupation, it could cause a slightly increase of female patients with SCI. In Beijing and Shanghai, the ratio was relatively lower because male and female nearly have equal access to various jobs in big cities. It was reported in Yang et al. (25) that the mean age of SCI patients was 41.6 (14.7) and age group of 41–60 had most injuries, but this was inconsistent with the high percentage of students (44.3%), which was much higher than worker (5.1%), and we can not explain this inconsistency.
Traffic accidents and falls are main causes of SCI in developed countries (43–45). People in these countries usually have a private car and this cause a high rate of car accidents. Old people living alone are prone to fall when walking up and down stairs. Similarly, MVCs and fall were the two leading cause in different regions in China (40). With the development of economy in China, most people had a private car and this led to the significant increase of car accidents, and disabilities caused by traffic accidences can be reduced through improve vehicle safety, driver behavior and road conditions (46). MCVs in Heilongjiang, Taiwan, Chongqing (2001–2011), Beijing (2001–2010), Guangdong (2003–2011) is the most common cause, while fall is the leading cause in Beijing (2002), Tianjin (2009–2014, 2008–2011, 2004–2008, 1998–2009, 2004–2007), Chongqing (2009–2013), Guangdong (2003–2011) and Anhui (2007–2010). In Beijing (2002), the study reported fall was the leading cause, while in 2001–2010, in 10-year-period, Beijing had development a lot and increasingly number of people owned their private car. Rate of car accident increased and MCVs became the leading cause. In Chongqing (2001–2011), the study was focused on SCI resulted from MCVs, while in 2009–2013, the leading cause was fall. Chongqing is called “mountain city” in China and the city is in mountains, so the incidence of fall was high. In Guangdong, Yang et al. (25) reported fall was leading cause, while Yang et al. (33) reported MCVs was the most common cause. These 2 studies based on different populations, so they got different conclusion. In Yang et al. (25) included 1340 cases, while 3,832 cases in Yang et al. (33). Low fall resulted in a large proportion of SCI as people aging. With social progresses and lifestyle changes, increasing number of old people pay more attention to their health conditions and engage in various activities, lacking of protective measures and experiences could increase risks of SCI. In some Western Asia countries, gunshots and violent conflicts account for a large proportion of SCI because people are accessible to firearms (47–49).
SCI can cause sensory or motor deficit and bladder dysfunction, so patients have high risks of complications. Pulmonary infection, urinary tract infection (UTIs) and bedsore are common complications, accounting for approximately 70%. Pulmonary infection in Guangdong (2003–2011) was high, which (33) and nearly twice as high as Tianjin (2008–2011). This because patients with high leval cervical SCI require mechanical ventilation but poor management will develop ventilator associated pneumonia. Besides, ability to cough is impaired due to paralysis of breathing muscles and it can cause pulmonary infections. UTIs in SCI patient are high both in high-income countries and less developed countries (50, 51) because patients who have bladder dysfunction have to use catheterization as a management method. The incidence of UTIs was high in Tianjin (2008–2011) and Guangdong (2003–2011). Evidences have shown that the methods of bladder management and different catheter material might relavant to UTIs (50). Other factors such as personal hygiene and long-term apply of indwelling catheter are associated with UTIs. Education on catheterization techniques and care can reduce and avoid UTIs. In addition, patients with SCI are more likely to suffering from bedsore due to sensation and mobility impair. Patients with bedsores were high in Guangdong (2003–2011, 15.4%) and Tianjin (2008–2011, 9.8%) (20, 25). Hospitals and rehabilitation centers should provide patients with careful management to prevent it, such as turn over frequently and skin checks on daily basis. Meanwhile, patients and their family members need training for nursing techniques to avoid bedsore. Furthermore, patients with SCI easily develop deep venous thrombosis (DVT). The percentage of DVT was reported in Tianjin (2008–2011) and in Guangdong (2003–2011), which needs rapid antithrombotic therapy to prevent potential pulmonary embolism. Electrolyte disturbance can be caused by methylprednisolone administration. It is controversial to use methylprednisolone currently but high dose use within 8 h after SCI is considered as a treatment option in China (52).
Studies have showed that surgery is the main treatment especially for complete injuries because it can prevent further injuries and improve spinal cord conditions (17, 19, 23, 25–27, 33). But weather perform surgery was depend on the severity and extent of injuries. Moreover, some patients chose conservative therapy while others against medical advice and left. Importantly, long term rehabilitation therapy is necessary for further functional recovery. Physical therapy is the main rehabilitation therapy and it based on functional training like standing and walking practice. Nursing and medication are also used to prevent complications in rehabilitation centers. Rehabilitation center was advanced in high income countries, whereas it is not well built in China.
Despite increasing number of literature was published, it was little research that summarize all the studies so as to further investigate the epidemiological features of SCI in China. This review tries to provide a more detailed epidemiological profile of SCI in China, but challenges should not be neglected. First, there is no standard diagnosis criteria in China, so most patients in studies are diagnosed by clinical and image criteria. Second, all studies were retrospective. Therefore, some data were incomplete or inaccurate. Third, lacking a register system in China, some cases meet the included criteria may not be included. Forth, conclusion may not be generalizable to the other regions.
Conclusion
Overall, this review summarizes studies and provides a up-to-date epidemiological features of SCI in China. Because the existence of limitations, it is challenging to obtain exact epidemiological data of SCI. Thus, more studies are needed to provide large amount of data and evidence. In addition, it is impeative to establish a national register system for SCI patients in the next few years and it will be helpful for throughtly understanding the epidemiological features of SCI in China.
Author Contributions
SY and ZS: study design, data analysis, original draft writing and editing. SY, ZS, FC, and JL: data collection, data analysis. SF: study design and supervision.
Funding
This work was supported by the State Key Program of the National Natural Science Foundation of China (81330042), the International Cooperation Program of National Natural Science Foundation of China (81620108018), the Special Program for Sino-Russian Joint Research Sponsored by the Ministry of Science and Technology, China (2014DFR31210), the Key Program Sponsored by the Tianjin Science and Technology Committee, China (13RCGFSY19000, 14ZCZDSY00044).
Conflict of Interest Statement
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
References
1. Ackery A, Tator C, Krassioukov A. A global perspective on spinal cord injury epidemiology. J Neurotrauma (2004) 21:1355–70. doi: 10.1089/neu.2004.21.1355
2. McCammon JR, Ethans K. Spinal cord injury in Manitoba: a provincial epidemiological study. J Spinal Cord Med. (2011) 34:6–10. doi: 10.1179/107902610X12923394765733
3. Jackson AB, Dijkers M, Devivo MJ, Poczatek RB. A demographic profile of new traumatic spinal cord injuries: change and stability over 30 years. Arch Phys Med Rehab. (2004) 85:1740–8. doi: 10.1016/j.apmr.2004.04.035
4. Jazayeri SB, Beygi S, Shokraneh F, Hagen EM, Rahimi-Movaghar V. Incidence of traumatic spinal cord injury worldwide: a systematic review. Eur Spine J. (2015) 24:905–18. doi: 10.1007/s00586-014-3424-6
5. Cripps RA, Lee BB, Wing P, Weerts E, Mackay J, Brown D. A global map for traumatic spinal cord injury epidemiology: towards a living data repository for injury prevention. Spinal Cord (2011) 49:493–501. doi: 10.1038/sc.2010.146
6. Wyndaele M, Wyndaele JJ. Incidence, prevalence and epidemiology of spinal cord injury: what learns a worldwide literature survey? Spinal Cord (2006) 44:523–9. doi: 10.1038/sj.sc.3101893
7. Thompson C, Mutch J, Parent S, Mac-Thiong JM. The changing demographics of traumatic spinal cord injury: an 11-year study of 831 patients. J Spinal Cord Med. (2015) 38:214–23. doi: 10.1179/2045772314Y.0000000233
8. Bjornshave Noe B, Mikkelsen EM, Hansen RM, Thygesen M, Hagen EM. Incidence of traumatic spinal cord injury in Denmark, 1990–2012: a hospital-based study. Spinal Cord (2015) 53:436–40. doi: 10.1038/sc.2014.181
9. Koskinen EA, Alen M, Vaarala EM, Rellman J, Kallinen M, Vainionpaa A. Centralized spinal cord injury care in Finland: unveiling the hidden incidence of traumatic injuries. Spinal Cord (2014) 52:779–84. doi: 10.1038/sc.2014.131
10. New PW, Baxter D, Farry A, Noonan VK. Estimating the incidence and prevalence of traumatic spinal cord injury in Australia. Arch Phys Med Rehab. (2015) 96:76–83. doi: 10.1016/j.apmr.2014.08.013
11. Ren YM, Wang XS, Wei ZJ, Fan BY, Lin W, Zhou XH, et al. Efficacy, safety, and cost of surgical versus nonsurgical treatment for carpal tunnel syndrome: a systematic review and meta-analysis. Medicine (Baltimore) (2016) 95:e4857. doi: 10.1097/MD.0000000000004857
12. Katoh S, Enishi T, Sato N, Sairyo K. High incidence of acute traumatic spinal cord injury in a rural population in Japan in 2011 and 2012: an epidemiological study. Spinal Cord (2014) 52:264–7. doi: 10.1038/sc.2014.13
13. Ning GZ, Wu Q, Li YL, Feng SQ. Epidemiology of traumatic spinal cord injury in Asia: a systematic review. J Spinal Cord Med. (2012) 35:229–39. doi: 10.1179/2045772312Y.0000000021
14. Wang Y, Xue Y, Zong Y, Ding H, Li Z, He D, et al. Treatment of atypical central cord injury without fracture or dislocation. Orthopedics (2015) 38:e524–8. doi: 10.3928/01477447-20150603-62
15. DeVivo MJ, Chen Y. Trends in new injuries, prevalent cases, and aging with spinal cord injury. Arch Phys Med Rehab. (2011) 92:332–8. doi: 10.1016/j.apmr.2010.08.031
16. Reinhardt JD, Zheng Y, Xu G, Lu X, Yin Y, Liu S, et al. People with spinal cord injury in China. Am J Phys Med Rehabil. (2017) 96:S61–5. doi: 10.1097/PHM.0000000000000680
17. Li J, Liu G, Zheng Y, Hao C, Zhang Y, Wei B, et al. The epidemiological survey of acute traumatic spinal cord injury (ATSCI) of 2002 in Beijing municipality. Spinal Cord (2011) 49:777–82. doi: 10.1038/sc.2011.8
18. Ye C, Sun T, Li J, Zhang F. Pattern of sports- and recreation-related spinal cord injuries in Beijing. Spinal Cord (2009) 47:857–60. doi: 10.1038/sc.2009.49
19. Zhou Y, Wang XB, Kan SL, Ning GZ, Li YL, Yang B, et al. Traumatic spinal cord injury in Tianjin, China: a single-center report of 354 cases. Spinal Cord (2016) 54:670–4. doi: 10.1038/sc.2015.173
20. Wu Q, Li YL, Ning GZ, Feng SQ, Chu TC, Li Y, et al. Epidemiology of traumatic cervical spinal cord injury in Tianjin, China. Spinal Cord (2012) 50:740–4. doi: 10.1038/sc.2012.42
21. Ning GZ, Yu TQ, Feng SQ, Zhou XH, Ban DX, Liu Y, et al. Epidemiology of traumatic spinal cord injury in Tianjin, China. Spinal Cord (2011) 49:386–90. doi: 10.1038/sc.2010.130
22. Feng HY, Ning GZ, Feng SQ, Yu TQ, Zhou HX. Epidemiological profile of 239 traumatic spinal cord injury cases over a period of 12 years in Tianjin, China. J Spinal Cord Med. (2011) 34:388–94. doi: 10.1179/2045772311Y.0000000017
23. Chang FS, Zhang Q, Sun M, Yu HJ, Hu LJ, Wu JH, et al. Epidemiological study of spinal cord injury individuals from halfway houses in Shanghai, China. J Spinal Cord Med. (2017) 41:450–8. doi: 10.1080/10790268.2017.1367357
24. Ning GZ, Mu ZP, Shangguan L, Tang Y, Li CQ, Zhang ZF, et al. Epidemiological features of traumatic spinal cord injury in Chongqing, China. J Spinal Cord Med. (2016) 39:455–60. doi: 10.1080/10790268.2015.1101982
25. Yang R, Guo L, Huang L, Wang P, Tang Y, Ye J, et al. Epidemiological characteristics of traumatic spinal cord injury in Guangdong, China. Spine (2017) 42:E555–61. doi: 10.1097/BRS.0000000000001896
26. Wang HF, Yin ZS, Chen Y, Duan ZH, Hou S, He J. Epidemiological features of traumatic spinal cord injury in Anhui Province, China. Spinal Cord (2013) 51:20–2. doi: 10.1038/sc.2012.92
27. Chen R, Liu X, Han S, Dong D, Wang Y, Zhang H, et al. Current epidemiological profile and features of traumatic spinal cord injury in Heilongjiang province, Northeast China: implications for monitoring and control. Spinal Cord (2017) 55:399–404. doi: 10.1038/sc.2016.92
28. Yang NP, Deng CY, Lee YH, Lin CH, Kao CH, Chou P. The incidence and characterisation of hospitalised acute spinal trauma in Taiwan–a population-based study. Injury (2008) 39:443–50. doi: 10.1016/j.injury.2007.12.007
29. Chen HY, Boore JR. Living with a relative who has a spinal cord injury: a grounded theory approach. J Clin Nurs. (2009) 18:174–82. doi: 10.1111/j.1365-2702.2008.02355.x
30. Wang H, Liu X, Zhao Y, Ou L, Zhou Y, Li C, et al. Incidence and pattern of traumatic spinal fractures and associated spinal cord injury resulting from motor vehicle collisions in China over 11 years: an observational study. Medicine (Baltimore). (2016) 95:e5220. doi: 10.1097/MD.0000000000005220
31. Wu Q, Ning GZ, Li YL, Feng HY, Feng SQ. Factors affecting the length of stay of patients with traumatic spinal cord injury in Tianjin, China. J Spinal Cord Med. (2013) 36:237–42. doi: 10.1179/2045772313Y.0000000090
32. Hua R, Shi J, Wang X, Yang J, Zheng P, Cheng H, et al. Analysis of the causes and types of traumatic spinal cord injury based on 561 cases in China from 2001 to 2010. Spinal Cord (2013) 51:218–21. doi: 10.1038/sc.2012.133
33. Yang R, Guo L, Wang P, Huang L, Tang Y, Wang W, et al. Epidemiology of spinal cord injuries and risk factors for complete injuries in Guangdong, China: a retrospective study. PLoS ONE (2014) 9:e84733. doi: 10.1371/journal.pone.0084733
34. Furlan JC, Sakakibara BM, Miller WC, Krassioukov AV. Global incidence and prevalence of traumatic spinal cord injury. Can J Neurol Sci. (2013) 40:456–64. doi: 10.1017/S0317167100014530
35. Chiu WT, Lin HC, Lam C, Chu SF, Chiang YH, Tsai SH. Review paper: epidemiology of traumatic spinal cord injury: comparisons between developed and developing countries. Asia-Pac J Public Health (2010) 22:9–18. doi: 10.1177/1010539509355470
36. Van Den Berg M, Castellote JM, Mahillo-Fernandez I, de Pedro-Cuesta J. Incidence of traumatic spinal cord injury in Aragon, Spain (1972–2008). J Neurotrauma (2011) 28:469–77. doi: 10.1089/neu.2010.1608
37. Divanoglou A, Levi R. Incidence of traumatic spinal cord injury in Thessaloniki, Greece and Stockholm, Sweden: a prospective population-based study. Spinal Cord (2009) 47:796–801. doi: 10.1038/sc.2009.28
38. McColl MA, Charlifue S, Glass C, Savic G, Meehan M. International differences in ageing and spinal cord injury. Spinal Cord (2002) 40:128–36. doi: 10.1038/sj.sc.3101264
39. Knutsdottir S, Thorisdottir H, Sigvaldason K, Jonsson H Jr., Bjornsson A, Ingvarsson P. Epidemiology of traumatic spinal cord injuries in Iceland from 1975 to 2009. Spinal Cord (2012) 50:123–6. doi: 10.1038/sc.2011.105
40. Liu P, Yao Y, Liu MY, Fan WL, Chao R, Wang ZG, et al. Spinal trauma in mainland China from 2001 to 2007: an epidemiological study based on a nationwide database. Spine (2012) 37:1310–5. doi: 10.1097/BRS.0b013e3182474d8b
41. O'Connor PJ. Forecasting of spinal cord injury annual case numbers in Australia. Arch Phys Med Rehab. (2005) 86:48–51. doi: 10.1016/j.apmr.2004.07.346
42. Obalum DC, Giwa SO, Adekoya-Cole TO, Enweluzo GO. Profile of spinal injuries in Lagos, Nigeria. Spinal Cord (2009) 47:134–7. doi: 10.1038/sc.2008.93
43. Dryden DM, Saunders LD, Rowe BH, May LA, Yiannakoulias N, Svenson LW, et al. The epidemiology of traumatic spinal cord injury in Alberta, Canada. Can J Neurol Sci. (2003) 30:113–21. doi: 10.1017/S0317167100053373
44. Lenehan B, Street J, Kwon BK, Noonan V, Zhang H, Fisher CG, et al. The epidemiology of traumatic spinal cord injury in British Columbia, Canada. Spine (2012) 37:321–9. doi: 10.1097/BRS.0b013e31822e5ff8
45. Pickett GE, Campos-Benitez M, Keller JL, Duggal N. Epidemiology of traumatic spinal cord injury in Canada. Spine (2006) 31:799–805. doi: 10.1097/01.brs.0000207258.80129.03
46. WHO. Road Traffic Injuries. World Health Organization (2017). Available online at: http://www.who.int/mediacentre/factsheets/fs358/en
47. Deconinck H. The health condition of spinal cord injuries in two Afghan towns. Spinal Cord (2003) 41:303–9. doi: 10.1038/sj.sc.3101443
48. Karamehmetoglu SS, Nas K, Karacan I, Sarac AJ, Koyuncu H, Ataoglu S, et al. Traumatic spinal cord injuries in southeast Turkey: an epidemiological study. Spinal Cord (1997) 35:531–3. doi: 10.1038/sj.sc.3100404
49. Otom AS, Doughan AM, Kawar JS, Hattar EZ. Traumatic spinal cord injuries in Jordan–an epidemiological study. Spinal Cord (1997) 35:253–5. doi: 10.1038/sj.sc.3100402
50. Cardenas DD, Hoffman JM, Kelly E, Mayo ME. Impact of a urinary tract infection educational program in persons with spinal cord injury. J Spinal Cord Med. (2004) 27:47–54. doi: 10.1080/10790268.2004.11753730
51. Dalton Wolfe JTH, McIntyre A, Iruthayarajah J, Loh E, Ethans K, Mehta S, et al. Bladder Management Following Spinal Cord Injury Spinal Cord Injury Rehabilitation Evidence. Version 5.0. Available online at: http://www.scireproject.com/
Keywords: spinal cord injury, SCI, epidemiology, China, incidence
Citation: Yuan S, Shi Z, Cao F, Li J and Feng S (2018) Epidemiological Features of Spinal Cord Injury in China: A Systematic Review. Front. Neurol. 9:683. doi: 10.3389/fneur.2018.00683
Received: 06 May 2018; Accepted: 30 July 2018;
Published: 22 August 2018.
Edited by:
Mattias K. Sköld, Uppsala University, SwedenReviewed by:
Corrado Iaccarino, Ospedale di Parma, ItalyFrancisco Capani, University of Buenos Aires, Argentina
Copyright © 2018 Yuan, Shi, Cao, Li and Feng. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Shiqing Feng, sqfeng@tmu.edu.cn
†These authors have contributed equally to this work
 Shiyang Yuan
Shiyang Yuan Zhongju Shi1,2†
Zhongju Shi1,2†