- Faculty of Medicine, Porto University, Porto, Portugal
- Department of Neurosurgery, Hospital São João, Porto, Portugal
- Neuroscience Unit, Hospital CUF Porto, Porto, Portugal
Correspondence Address:
Ana Rita Aleixo Laiginhas
Faculty of Medicine, Porto University, Porto, Portugal
Department of Neurosurgery, Hospital São João, Porto, Portugal
Neuroscience Unit, Hospital CUF Porto, Porto, Portugal
DOI:10.4103/2152-7806.167211
Copyright: © 2015 Surgical Neurology International This is an open access article distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 3.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Aleixo Laiginhas AR, Silva PA, Pereira P, Vaz R. Long-term clinical and radiological follow-up after laminectomy for cervical spondylotic myelopathy. Surg Neurol Int 13-Oct-2015;6:162
How to cite this URL: Aleixo Laiginhas AR, Silva PA, Pereira P, Vaz R. Long-term clinical and radiological follow-up after laminectomy for cervical spondylotic myelopathy. Surg Neurol Int 13-Oct-2015;6:162. Available from: http://surgicalneurologyint.com/surgicalint_articles/long%e2%80%91term-clinical-and-radiological-follow%e2%80%91up-after-laminectomy/
Abstract
Background:The role of laminectomy in the surgical treatment of cervical spondylotic myelopathy (CSM) is established even though postoperative cervical sagittal balance changes and a risk for long-term instability have been described. The aim of the present study is to investigate its clinical efficacy and the radiological outcome in the long-term.
Methods:The authors retrospectively reviewed consecutive cases of patients with CSM, who underwent cervical laminectomy between 1995 and 2010 at the Hospital São João (n = 106). Clinical files were consulted, and the patients reassessed in order to collect information on complaints, previous neurological deficits, surgery and its complications. Subjective and objective clinical evaluation (by three myelopathy scores) and imaging studies were undertaken in order to assess the long-term cervical sagittal curvature and presence of instability.
Results:After applying exclusion criteria, 57 patients were able to complete the follow-up. A favorable statistically significant difference was obtained when comparing clinical scores. Ninety-one percent of patients were satisfied with the outcome of the surgery. Only 1 patient developed kyphosis according to Ishihara index and none according to the method of Matsumoto. Four patients developed subclinical cervical instability. No clinical-imaging correlation was found.
Conclusions:If patients are properly selected cervical laminectomy without additional instrumentation is effective in offering a clinical improvement to patients with CSM with a low incidence of clinically significant radiological deterioration.
Keywords: Cervical laminectomy, cervical spondylotic myelopathy, kyphosis
INTRODUCTION
The aims of the present study are to investigate the long-term efficacy and safety of stand-alone cervical laminectomy in patients with cervical spondylotic myelopathy (CSM) and to investigate the radiological outcome related thereto.
Laminectomy has assumed an irreplaceable role in preventing symptomatic progression of CSM but emerging alternative procedures filed controversy among surgeons.[
MATERIALS AND METHODS
Study design
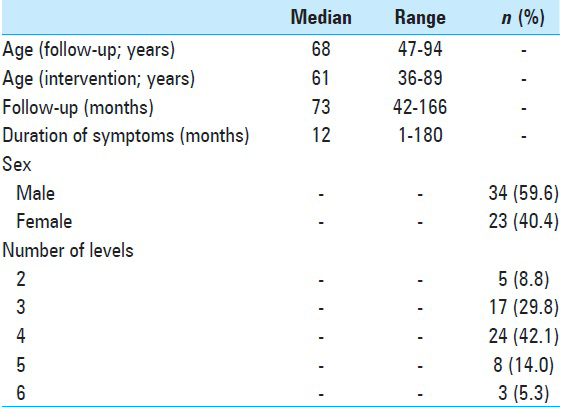
In this retrospective analysis consecutive patients with the diagnosis of CSM who underwent cervical laminectomy at the Department of Neurosurgery of the Hospital São João during a period from January 1st, 1995 to December 31st , 2010 were enrolled. Cases with the acute progression of myelopathy due to other causes, insufficient follow-up, posterior instrumentation and/or fusion in addition to laminectomy were excluded. A total of 106 were enrolled in the study. According to exclusion criteria 49 patients were ruled out; the remaining 57 were admitted to the protocol and 47 of these did long-term X-rays.
The preoperative evaluation relied on the revision of medical records and imaging on file. Patients were re-evaluated through a clinical interview at a minimum of 3 years after the surgery. The Ethics Committee of the Hospital approved the study protocol, and all patients signed an informed consent.
Clinical evaluation
Functional assessment was performed by applying the modified Japanese Orthopaedic Association (mJOA) Score, the European myelopathy score (EMS) and the myelopathy disability index (MDI).[
A subjective evaluation was additionally performed by asking the patient to grade groups of symptoms as comparatively better, stable or worse with regarding the preoperative status.
Variables that could be related to the outcome, as well as long-term clinical-imaging correlation, were also investigated in order to better understand the impact of the surgical procedure in different groups of patients.
Radiological evaluation
Both the Ishihara index and the angle of cervical lordosis according to the method of Matsumoto were calculated from pre- and post-operative X-rays.[
To avoid bias, all radiological measurements were performed blindly 3 times by the same investigator and averaged.
Statistical analysis
For statistical analysis, paired and independent t-tests were used when comparing a binomial categorical variable with a numeric variable. When studying two numerical variables Spearman correlation was used (namely to ascertain clinical-radiological relationship). Levene test was used to assess the homogeneity of variances. A P value below 0.05 was considered significant. Box plots and error bar graphs were used. Data was processed using SPSS Statistics® version 22.0 (Armonk, NY: IBM Corp.) software on Microsoft Windows® .
RESULTS
All applied scores indicate a significantly improved long-term functional status – higher mJOA (13.0 vs. 14.7; P < 0.001) and EMS (13.6 vs. 15.4; P < 0.001) scores and lower MDI score (9.3 vs. 5.7; P < 0.001). After long-term follow-up (mean: 6.3 years) 91% of patients (n = 52) reported being satisfied with the outcome of surgery and 93% (n = 53) said that if they could go back in time they would again go through it. The mean imaging follow-up was 6.4 years (standard deviation 3.1). The mean postoperative Ishihara index was 19.3 (lordotic). According to this method, only 1 patient (2%) had kyphosis at long-term follow-up (−4.6). The mean long-term lordosis estimated by the method of Matsumoto was 19.4°. According to this method, no patient developed a kyphotic angle. Subclinical segmental instability was found in 7% of patients after long-term follow-up (n = 4). Among patients who had preoperative exams data was not conclusive regarding a progressive tendency towards kyphosis (according to Ishihara index, variation was −0.37 versus Matsumoto angle, a variation of + 0.94).
Complications
Only 9% of patients experienced surgical complications (n = 5): Two cases of superficial surgical wound infection (handled under conservative management) and three transient postoperative C5 radiculopathies. No patient was re-operated due to iatrogenic deformity.
Correlations
Duration of symptoms correlated with higher functional outcome according to mJOA, EMS, and MDI scores. Patients with symptoms for over 12 months reach lower long-term score values when comparing with patients with symptoms for <1-year (13.7 vs. 15.4). However, there was no significant difference in the variation of functional status. No correlation could be established between other studied variables and clinical/radiological outcome.
DISCUSSION
This retrospective study evaluated long-term (minimum of 3 years) results of patients who underwent cervical laminectomy for CSM. All functional outcome scales used yielded a significant improvement in clinical status after an average of over 6 years of follow-up that is in favor of the long-term effectiveness of the procedure. Furthermore, over 90% of patients were satisfied with the outcome that favors the effect of the surgery on their daily lives. The effectiveness of cervical laminectomy as a decompressive technique has been documented repeatedly; in literature clinical improvement after cervical laminectomy ranges from 42% to 92% which is in agreement with our results.[
We found no clinical-radiological correlation that is in accordance with the previous literature.[
Regarding complications we identified a rate of 9% comprising postoperative C5 radiculopathy and superficial wound infection that is, consistent with the literature;[
An insurmountable limitation of this study relates to its retrospective character although we tried to overcome the risk of collecting biased information by comparing multiple records. Prospective controlled studies are likely to give more strength to our conclusions, yet these findings may be helpful in substantiating surgical decisions.
CONCLUSIONS
Given an adequate preoperative selection of patients with CSM it does not appear necessary to routinely adjunct instrumentation to laminectomy in order to achieve clinical improvement or appropriate radiological outcomes in the long-term. However, prospective controlled studies are needed to support this conclusion.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
1. Guidetti B, Fortuna A. Long-term results of surgical treatment of myelopathy due to cervical spondylosis. J Neurosurg. 1969. 30: 714-21
2. Hamanishi C, Tanaka S. Bilateral multilevel laminectomy with or without posterolateral fusion for cervical spondylotic myelopathy: Relationship to type of onset and time until operation. J Neurosurg. 1996. 85: 447-51
3. Hsu L. Cervical laminectomy: Overview and management. J Pain Palliat Care Pharmacother. 2012. 26: 371-2
4. Kaptain GJ, Simmons NE, Replogle RE, Pobereskin L. Incidence and outcome of kyphotic deformity following laminectomy for cervical spondylotic myelopathy. J Neurosurg. 2000. 93: S199-204
5. Lad SP, Babu R, Ugiliweneza B, Patil CG, Boakye M. Surgery for spinal stenosis: Long-term reoperation rates, health care cost, and impact of instrumentation. Spine (Phila Pa 1976). 2014. 39: 978-87
6. McAllister BD, Rebholz BJ, Wang JC. Is posterior fusion necessary with laminectomy in the cervical spine?. Surg Neurol Int. 2012. 3: S225-31
7. Ryken TC, Heary RF, Matz PG, Anderson PA, Groff MW, Holly LT. Cervical laminectomy for the treatment of cervical degenerative myelopathy. J Neurosurg Spine. 2009. 11: 142-9
8. van Geest S, de Vormer AM, Arts MP, Peul WC, Vleggeert-Lankamp CL. Long-term follow-up of clinical and radiological outcome after cervical laminectomy. Eur Spine J. 2015. 24: 229-35
9. Ishihara A. Roentgenographic studies on the normal pattern of the cervical curvature. J Jpn Orthop Assoc. 1968. 42: 1033-44