Abstract
Purpose
The objective of this study was to compare the safety and efficacy of minimally invasive discectomy (MID) with standard discectomy (SD) and determine whether the use of the MID technique could decrease the recurrence of lumbar disc herniation (LDH) after the surgery.
Methods
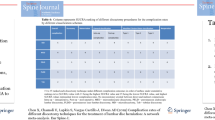
In February 2014, a comprehensive search was performed in PubMed, EMBASE, Web of Science, Cochrane Library and the Chinese Biological Medicine Database. Only randomised controlled trials (RCT) that compared MID with SD for the surgical management of LDH were included. These trials were carefully picked out following the inclusion and exclusion criteria. Using the Cochrane Collaboration guidelines, two authors independently extracted data and assessed these trials’ quality. The age of the patients, size of incision, surgical time, blood loss, visual analogue scale (VAS) score after the surgery, hospital stay, disc herniation recurrence, X-ray exposure and surgical costs in these studies were abstracted and synthesised by a meta-analysis with RevMan 5.2.0 software, and the main results (VAS score after the surgery and disc herniation recurrence) of publication bias were examined by Stata 12.0.
Results
Overall, 16 trials involving 2,139 patients meeting our criteria were included and analysed. Comparing MID and SD, the former was more likely to increase disc herniation recurrence [relative risk (RR) = 1.95, 95 % confidence interval (CI) 1.19–3.19, p = 0.008], and it involved a smaller size of incision [mean difference (MD) = −1.91, 95 % CI −3.33 to −0.50, p = 0.008], shorter hospital stay, longer operating time (MD = 11.03, 95 %C I 6.62–15.44, p < 0.00001) and less blood loss (MD = −13.56, 95 % CI −22.26 to −4.87, p = 0.002), while no statistical difference appeared with regard to the age of the patients, VAS score after the surgery, X-ray exposure, hospital stay and surgical costs.
Conclusions
Based on available evidence, MID results in less suffering for patients during the hospital course with a similar clinical efficacy compared to SD. This makes MID a promising procedure for patients with LDH; however, to popularise it greater effort is required to reduce disc herniation recurrence.










Similar content being viewed by others
References
Campbell P, Wynne-Jones G, Muller S, Dunn KM (2013) The influence of employment social support for risk and prognosis in nonspecific back pain: a systematic review and critical synthesis. Int Arch Occup Environ Health 86:119–137. doi:10.1007/s00420-012-0804-2
Hoy DG, Smith E, Cross M, Sanchez-Riera L, Buchbinder R, Blyth FM, Brooks P, Woolf AD, Osborne RH, Fransen M, Driscoll T, Vos T, Blore JD, Murray C, Johns N, Naghavi M, Carnahan E, March LM (2014) The global burden of musculoskeletal conditions for 2010: an overview of methods. Ann Rheum Dis. doi:10.1136/annrheumdis-2013-204344
Gautschi OP, Hildebrandt G, Cadosch D (2008) Acute low back pain–assessment and management. Praxis 97:58–68
Saleem S, Aslam HM, Rehmani MA, Raees A, Alvi AA, Ashraf J (2013) Lumbar disc degenerative disease: disc degeneration symptoms and magnetic resonance image findings. Asian Spine J 7:322–334. doi:10.4184/asj.2013.7.4.322
Schoenfeld AJ (2011) Historical contributions from the Harvard system to adult spine surgery. Spine 36:E1477–E1484. doi:10.1097/BRS.0b013e3181f2d52c
Koebbe CJ, Maroon JC, Abla A, El-Kadi H, Bost J (2002) Lumbar microdiscectomy: a historical perspective and current technical considerations. Neurosurg Focus 13:E3
Arts MP, Brand R, van den Akker ME, Koes BW, Bartels R, Peul WC, Leiden-The Hague Spine Intervention Prognostic Study Group (SIPS) (2009) Tubular diskectomy vs conventional microdiskectomy for sciatica: a randomized controlled trial. JAMA 302:149–158
Teli M, Lovi A, Brayda-Bruno M, Zagra A, Corriero A, Giudici F, Minoia L (2010) Higher risk of dural tears and recurrent herniation with lumbar micro-endoscopic discectomy. Eur Spine J 19:443–450. doi:10.1007/s00586-010-1290-4
van Tulder M, Furlan A, Bombardier C, Bouter L et al (2003) Updated method guidelines for systematic reviews in the Cochrane Collaboration Back Review Group. Spine 28:1290–1299. doi:10.1097/01.brs.0000065484.95996.af
Sterne JA, Egger M, Smith GD (2001) Systematic reviews in health care: investigating and dealing with publication and other biases in meta-analysis. BMJ 323:101–105
Tullberg T, Isacson J, Weidenhielm L (1993) Does microscopic removal of lumbar disc herniation lead to better results than the standard procedure? Results of a one-year randomized study. Spine 18:24–27
Henriksen L, Schmidt K, Eskesen V, Jantzen E (1996) A controlled study of microsurgical versus standard lumbar discectomy. Br J Neurosurg 10:289–293
Hermantin FU, Peters T, Quartararo L, Kambin P (1999) A prospective, randomized study comparing the results of open discectomy with those of video-assisted arthroscopic microdiscectomy. J Bone Joint Surg Am 81:958–965
Türeyen K (2003) One-level one-sided lumbar disc surgery with and without microscopic assistance: 1-year outcome in 114 consecutive patients. J Neurosurg 99:247–250
Huang TJ, Hsu RW, Li YY, Cheng CC (2005) Less systemic cytokine response in patients following microendoscopic versus open lumbar discectomy. J Orthop Res 23:406–411
Katayama Y, Matsuyama Y, Yoshihara H, Sakai Y, Nakamura H, Nakashima S, Ito Z, Ishiguro N (2006) Comparison of surgical outcomes between macro discectomy and micro discectomy for lumbar disc herniation: a prospective randomized study with surgery performed by the same spine surgeon. J Spinal Disord Tech 19:344–347
Righesso O, Falavigna A, Avanzi O (2007) Comparison of open discectomy with microendoscopic discectomy in lumbar disc herniations: results of a randomized controlled trial. Neurosurgery 61:545–549
Ryang YM, Oertel MF, Mayfrank L, Gilsbach JM, Rohde V (2008) Standard open microdiscectomy versus minimal access trocar microdiscectomy: results of a prospective randomized study. Neurosurgery 62:174–181. doi:10.1227/01.neu.0000311075.56486.c5, discussion 181–172
Arts M, Brand R, van der Kallen B, Lycklama à Nijeholt G, Peul W (2011) Does minimally invasive lumbar disc surgery result in less muscle injury than conventional surgery? A randomized controlled trial. Eur Spine J 20:51–57. doi:10.1007/s00586-010-1482-y
Arts MP, Brand R, van den Akker ME, Koes BW, Bartels RHA, Tan W, Peul WC (2011) Tubular diskectomy vs conventional microdiskectomy for the treatment of lumbar disk herniation: 2-year results of a double-blind randomized controlled trial. Neurosurgery 69:135–144
Garg B, Nagraja UB, Jayaswal A (2011) Microendoscopic versus open discectomy for lumbar disc herniation: a prospective randomised study. J Orthop Surg (Hong Kong) 19:30–34
Mariscalco MW, Yamashita T, Steinmetz MP, Krishnaney AA, Lieberman IH, Mroz TE (2011) Radiation exposure to the surgeon during open lumbar microdiscectomy and minimally invasive microdiscectomy: a prospective, controlled trial. Spine 36:255–260
van den Akker ME, Arts MP, van den Hout WB, Brand R, Koes BW, Peul WC (2011) Tubular diskectomy vs conventional microdiskectomy for the treatment of lumbar disk-related sciatica: cost utility analysis alongside a double-blind randomized controlled trial. Neurosurgery 69:829–835
Wang HL, Lü FZ, Jiang JY, Ma X, Xia XL, Wang LX (2011) Minimally invasive lumbar interbody fusion via MAST quadrant retractor versus open surgery: a prospective randomized clinical trial. Chin Med J 124:3868–3874
Arts MP, Peul WC, Brand R, Koes BW, Thomeer RTWM (2006) Cost-effectiveness of microendoscopic discectomy versus conventional open discectomy in the treatment of lumbar disc herniation: a prospective randomised controlled trial [ISRCTN51857546]. BMC Musculoskelet Disord 7:42
Suk KS, Lee HM, Moon SH, Kim NH (2001) Recurrent lumbar disc herniation: results of operative management. Spine 26:672–676
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Chang, X., Chen, B., Li, Hy. et al. The safety and efficacy of minimally invasive discectomy: a meta-analysis of prospective randomised controlled trials. International Orthopaedics (SICOT) 38, 1225–1234 (2014). https://doi.org/10.1007/s00264-014-2331-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00264-014-2331-0