Abstract
Objective
The purpose of this study is to compare the effectiveness and safety of artificial total disc replacement (TDR) with fusion for the treatment of lumbar degenerative disc disease (DDD).
Summary of background data
Spinal fusion is the conventional surgical treatment for lumbar DDD. Recently, TDR has been developed to avoid the negative effects of the fusion by preserving function of the motion segment. Controversy still surrounds regarding whether TDR is better.
Methods
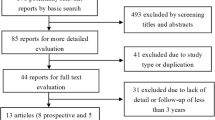
We systematically searched six electronic databases (Medline, Embase, Clinical, Ovid, BIOSIS and Cochrane registry of controlled clinical trials) to identify randomized controlled trials (RCTs) published up to March 2013 in which TDR was compared with the fusion for the treatment of lumbar DDD. Effective data were extracted after the assessment of methodological quality of the trials. Then, we performed the meta-analysis.
Results
Seven relevant RCTs with a total of 1,584 patients were included. TDR was more effective in ODI (MD −5.09; 95 % CI [−7.33, −2.84]; P < 0.00001), VAS score (MD −5.31; 95 % CI [−8.35, −2.28]; P = 0.0006), shorter duration of hospitalization (MD −0.82; 95 % CI [−1.38, −0.26]; P = 0.004) and a greater proportion of willing to choose the same operation again (OR 2.32; 95 % CI [1.69, 3.20]; P < 0.00001). There were no significant differences between the two treatment methods regarding operating time (MD −44.16; 95 % CI [−94.84, 6.52]; P = 0.09), blood loss (MD −29.14; 95 % CI [−173.22, 114.94]; P = 0.69), complications (OR 0.72; 95 % CI [0.45, 1.14]; P = 0.16), reoperation rate (OR 0.83; 95 % CI [0.39, 1.77]; P = 0.63) and the proportion of patients who returned to full-time/part-time work (OR 1.10; 95 % CI [0.86, 1.41]; P = 0.47).
Conclusion
TDR showed significant safety and efficacy comparable to lumbar fusion at 2 year follow-up. TDR demonstrated superiorities in improved physical function, reduced pain and shortened duration of hospitalization. The benefits of operating time, blood loss, motion preservation and the long-term complications are still unable to be proved.










Similar content being viewed by others
References
Berg S, Tropp HT, Leivseth G (2011) Disc height and motion patterns in the lumbar spine in patients operated with total disc replacement or fusion for discogenic back pain. Results from a randomized controlled trial. Spine J 11:991–998
Kumar A, Beastall J, Hughes J et al (2008) Disc changes in the bridged and adjacent segments after Dynesys dynamic stabilization system after two years. Spine (Phila Pa 1976) 33:2909–2914
Bono CM, Kadaba M, Vaccaro AR (2009) Posterior pedicle fixation-based dynamic stabilization devices for the treatment of degenerative diseases of the lumbar spine. J Spinal Disord Tech 22:376–383
Kalanithi PS, Patil CG, Boakye M (2009) National complication rates and disposition after posterior lumbar fusion for acquired spondylolisthesis. Spine (Phila Pa 1976) 34:1963–1969
Lee SE, Park SB, Jahng TA, Chung CK, Kim HJ (2008) Clinical experience of the dynamic stabilization system for the degenerative spine disease. J Korean Neurosurg Soc 43:221–226
Reyes-Sanchez A, Zarate-Kalfopulos B, Ramirez-Mora I, Rosales-Olivarez LM, Alpizar-Aguirre A, Sanchez-Bringas G (2010) Posterior dynamic stabilization of the lumbar spine with the Accuflex rod system as a stand-alone device: experience in 20 patients with 2-year follow-up. Eur Spine J 19:2164–2170
Auerbach JD, Jones KJ, Milby AH, Anakwenze OA, Balderston RA (2009) Segmental contribution toward total lumbar range of motion in disc replacement and fusions: a comparison of operative and adjacent levels. Spine (Phila Pa 1976) 34:2510–2517
Gamradt SC, Wang JC (2005) Lumbar disc arthroplasty. Spine J 5:95–103
Yajun W, Yue Z, Xiuxin H, Cui C (2010) A meta-analysis of artificial total disc replacement versus fusion for lumbar degenerative disc disease. Eur Spine J 19:1250–1261
Oremus M, Wolfson C, Perrault A, Demers L, Momoli F, Moride Y (2001) Interrater reliability of the modified Jadad quality scale for systematic reviews of Alzheimer’s disease drug trials. Dement Geriatr Cogn Disord 12:232–236
van Tulder M, Furlan A, Bombardier C, Bouter L (2003) Updated method guidelines for systematic reviews in the Cochrane collaboration back review group. Spine (Phila Pa 1976) 28:1290–1299
Ostelo RW, de Vet HC (2005) Clinically important outcomes in low back pain. Best Pract Res Clin Rheumatol 19:593–607
Lauridsen HH, Hartvigsen J, Manniche C, Korsholm L, Grunnet-Nilsson N (2006) Responsiveness and minimal clinically important difference for pain and disability instruments in low back pain patients. BMC Musculoskelet Disord 7:82
Higgins JP, Thompson SG (2002) Quantifying heterogeneity in a meta-analysis. Stat Med 21:1539–1558
Higgins JP, Thompson SG, Deeks JJ, Altman DG (2003) Measuring inconsistency in meta-analyses. BMJ 327:557–560
Furlan AD, Pennick V, Bombardier C, van Tulder M (2009) updated method guidelines for systematic reviews in the Cochrane Back Review Group. Spine (Phila Pa 1976) 34:1929–1941
Blumenthal S, McAfee PC, Guyer RD et al (2005) A prospective, randomized, multicenter food and drug administration investigational device exemptions study of lumbar total disc replacement with the CHARITE artificial disc versus lumbar fusion: part I: evaluation of clinical outcomes. Spine (Phila Pa 1976) 30(1565–1575):E387–E391
Sasso RC, Foulk DM, Hahn M (2008) Prospective, randomized trial of metal-on-metal artificial lumbar disc replacement: initial results for treatment of discogenic pain. Spine (Phila Pa 1976) 33:123–131
Zigler J, Delamarter R, Spivak JM et al (2007) Results of the prospective, randomized, multicenter food and drug administration investigational device exemption study of the ProDisc-L total disc replacement versus circumferential fusion for the treatment of 1-level degenerative disc disease. Spine (Phila Pa 1976) 32:1155–1163
Gornet MF, Burkus JK, Dryer RF, Peloza JH (2011) Lumbar disc arthroplasty with MAVERICK disc versus stand-alone interbody fusion: a prospective, randomized, controlled, multicenter investigational device exemption trial. Spine (Phila Pa 1976) 36:E1600–E1611
Delamarter RB, Bae HW, Pradhan BB (2005) Clinical results of ProDisc-II lumbar total disc replacement: report from the United States clinical trial. Orthop Clin North Am 36:301–313
Delamarter R, Zigler JE, Balderston RA, Cammisa FP, Goldstein JA, Spivak JM (2011) Prospective, randomized, multicenter food and drug administration investigational device exemption study of the ProDisc-l total disc replacement compared with circumferential arthrodesis for the treatment of two-level lumbar degenerative disc disease: results at 24 months. J Bone Joint Surg Am 93:705–715
Berg S, Tullberg T, Branth B, Olerud C, Tropp H (2009) Total disc replacement compared to lumbar fusion: a randomised controlled trial with 2-year follow-up. Eur Spine J 18:1512–1519
Ozer AF, Crawford NR, Sasani M et al (2010) Dynamic lumbar pedicle screw-rod stabilization: two-year follow-up and comparison with fusion. Open Orthop J 4:137–141
Morishita Y, Ohta H, Naito M et al (2011) Kinematic evaluation of the adjacent segments after lumbar instrumented surgery: a comparison between rigid fusion and dynamic non-fusion stabilization. Eur Spine J 20:1480–1485
Cheng BC, Gordon J, Cheng J, Welch WC (2007) Immediate biomechanical effects of lumbar posterior dynamic stabilization above a circumferential fusion. Spine (Phila Pa 1976) 32:2551–2557
Beastall J, Karadimas E, Siddiqui M et al (2007) The Dynesys lumbar spinal stabilization system: a preliminary report on positional magnetic resonance imaging findings. Spine (Phila Pa 1976) 32:685–690
Yu SW, Yen CY, Wu CH, Kao FC, Kao YH, Tu YK (2012) Radiographic and clinical results of posterior dynamic stabilization for the treatment of multisegment degenerative disc disease with a minimum follow-up of 3 years. Arch Orthop Trauma Surg 132:583–589
Zencica P, Chaloupka R, Hladikova J, Krbec M (2010) Adjacent segment degeneration after lumbosacral fusion in spondylolisthesis: a retrospective radiological and clinical analysis. Acta Chir Orthop Traumatol Cech 77:124–130
Harrop JS, Youssef JA, Maltenfort M et al (2008) Lumbar adjacent segment degeneration and disease after arthrodesis and total disc arthroplasty. Spine (Phila Pa 1976) 33:1701–1707
Levin DA, Hale JJ, Bendo JA (2007) Adjacent segment degeneration following spinal fusion for degenerative disc disease. Bull NYU Hosp Jt Dis 65:29–36
Park P, Garton HJ, Gala VC, Hoff JT, McGillicuddy JE (2004) Adjacent segment disease after lumbar or lumbosacral fusion: review of the literature. Spine (Phila Pa 1976) 29:1938–1944
van den Eerenbeemt KD, Ostelo RW, van Royen BJ, Peul WC, van Tulder MW (2010) Total disc replacement surgery for symptomatic degenerative lumbar disc disease: a systematic review of the literature. Eur Spine J 19:1262–1280
Frelinghuysen P, Huang RC, Girardi FP, Cammisa FJ (2005) Lumbar total disc replacement part I: rationale, biomechanics, and implant types. Orthop Clin North Am 36:293–299
McAfee PC, Cunningham B, Holsapple G et al (2005) A prospective, randomized, multicenter food and drug administration investigational device exemption study of lumbar total disc replacement with the CHARITE artificial disc versus lumbar fusion: part II: evaluation of radiographic outcomes and correlation of surgical technique accuracy with clinical outcomes. Spine (Phila Pa 1976) 30:1576–1583 E388–E390
Freeman BJ, Davenport J (2006) Total disc replacement in the lumbar spine: a systematic review of the literature. Eur Spine J 15(Suppl 3):S439–S447
Gibson JN, Waddell G (2005) Surgery for degenerative lumbar spondylosis. Cochrane Database Syst Rev D1352
Han X, Zhu Y, Cui C, Wu Y (2009) A meta-analysis of circumferential fusion versus instrumented posterolateral fusion in the lumbar spine. Spine (Phila Pa 1976) 34:E618–E625
Madan SS, Boeree NR (2003) Comparison of instrumented anterior interbody fusion with instrumented circumferential lumbar fusion. Eur Spine J 12:567–575
Conflict of interest
The authors declare that they have no conflict of interest.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Rao, MJ., Cao, SS. Artificial total disc replacement versus fusion for lumbar degenerative disc disease: a meta-analysis of randomized controlled trials. Arch Orthop Trauma Surg 134, 149–158 (2014). https://doi.org/10.1007/s00402-013-1905-4
Received:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00402-013-1905-4