Abstract
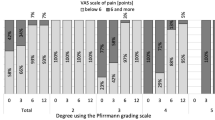
Several studies have suggested that psychosocial distress is an important predictor of negative outcome in lumbar spine surgery. Ozguler et al. [Spine 27:1783–1789, 2002, 18] described a classification tool for low back pain patients using the Dallas Pain Questionnaire (DPQ) which included a measure of distress. We wanted to evaluate the ability of this classification tool to predict the outcome in spinal fusion patients. Five hundred and sixty-six patients (239 men, 327 women; mean age 46, range 18–81) operated between 1992 and 2002, with a complete DPQ preoperatively and after a minimum of 1-year follow-up, were included. They were classified preoperatively and at follow-up into four groups: group 1 (slight disability), group 2 (intermediate disability), group 3 (major disability) and group 4 (major disability and emotional distress). Using logistic regression, seven predictor variables were investigated: age (−39 years/40–59 years/60+ years), Gender (male/female), Indication (spondylolisthesis/primary degeneration/secondary degeneration), Work status (working/without work or on sick leave/retired or pensioned), Duration of pain (less than 1 year/1–2 years/more than 2 years), Presence of radiating pain (yes/no) and disability/distress [intermediate disability (group 1–2)/major disability (group 3)/major disability and distress (group 4)]. The outcome variable was disability at follow-up (low = group1 + 2/high = group 3 + 4). Preoperative classification was group 1, 1%; group 2, 14%; group 3, 37%; group 4, 48%. Variables found to predict high disability at follow-up were secondary degeneration Odds Ratio (OR) 1.61 (P=0.020), being retired/pensioned OR 3.48 (P<0.0005), age between 40–59 years OR 1.68 (P=0.011), belonging to group 3 OR 2.69 (P=0.003) or belonging to group 4 OR 5.53 (P<0.0005). The classification based on the DPQ were able to identify lumbar spinal fusion patients with a considerable amount of psychological distress in their symptomatology. Furthermore, the presence of distress, as determined by this classification, was a highly significant risk factor for inferior outcome.


Similar content being viewed by others
References
Christensen FB, Bunger CE (1997) Retrograde ejaculation after retroperitoneal lower lumbar interbody fusion. Int Orthop 21:176–180
Christensen FB, Karlsmose B, Hansen ES, Bunger CE (1996) Radiological and functional outcome after anterior lumbar interbody spinal fusion. Eur Spine J 5:293–298
Christensen FB, Thomsen K, Eiskjaer SP, Gelinick J, Bunger CE (1998) Functional outcome after posterolateral spinal fusion using pedicle screws: comparison between primary and salvage procedure. Eur Spine J 7:321–327
Christensen FB, Laursen M, Gelineck J, Hansen ES, Bunger CE (2001) Posterolateral spinal fusion at unintended levels due to bone-graft migration: no effect on clinical outcome in 19/130 patients. Acta Orthop Scand 72:354–358
Christensen FB, Hansen ES, Eiskjaer SP, Hoy K, Helmig P, Neumann P, Niedermann B, Bunger CE (2002) Circumferential lumbar spinal fusion with brantigan cage versus posterolateral fusion with titanium cotrel-dubousset instrumentation: a prospective, randomized clinical study of 146 patients. Spine 27:2674–2683
Christensen FB, Hansen ES, Laursen M, Thomsen K, Bunger CE (2002) Long-term functional outcome of pedicle screw instrumentation as a support for posterolateral spinal fusion: randomized clinical study with a 5-year follow-up. Spine 27:1269–1277
Dupont WD (2002) Statistical modeling for biomedical researchers. A simple introduction to the analysis of complex data. University Press, Cambridge
Haas M, Jacobs GE, Raphael R, Petzing K (1995) Low back pain outcome measurement assessment in chiropractic teaching clinics: responsiveness and applicability of two functional disability questionnaires. J Manipulative Physiol Ther 18:79–87
Hagg O, Fritzell P, Ekselius L, Nordwall A (2003) Predictors of outcome in fusion surgery for chronic low back pain. A report from the Swedish Lumbar Spine Study. Eur Spine J 12:22–33
Hobby JL, Lutchman LN, Powell JM, Sharp DJ (2001) The distress and risk assessment method (DRAM). J Bone Joint Surg Br 83:19–21
Hosmer DW, Lemeshow S (2000) Applied logistic regression. Wiley, New York
Hunt SM, McKenna SP, McEwen J, Backett EM, Williams J, Papp E (1980) A quantitative approach to perceived health status: a validation study. J Epidemiol Community Health 34:281–286
Jamison J (2002) Chiropractic management: beyond manual care. J Manipulative Physiol Ther 25:332
Junge A, Frohlich M, Ahrens S, Hasenbring M, Sandler A, Grob D, Dvorak J (1996) Predictors of bad and good outcome of lumbar spine surgery. A prospective clinical study with 2 years’ follow up. Spine 21:1056–1064
Lawlis GF, Cuencas R, Selby D, McCoy CE (1989) The development of the Dallas Pain Questionnaire. An assessment of the impact of spinal pain on behavior. Spine 14:511–516
Main CJ, Wood PL, Hollis S, Spanswick CC, Waddell G (1992) The distress and risk assessment method. A simple patient classification to identify distress and evaluate the risk of poor outcome. Spine 17:42–52
Nickel R, Egle UT, Rompe J, Eysel P, Hoffmann SO (2002) Somatisation predicts the outcome of treatment in patients with low back pain. J Bone Joint Surg Br 84:189–195
Ozguler A, Gueguen A, Leclerc A, Landre MF, Piciotti M, Le Gall S, Morel-Fatio M, Boureau F (2002) Using the dallas pain questionnaire to classify individuals with low back pain in a working population. Spine 27:1783–1789
Piperno M, Hellio le Graverand MP, Reboul P, Mathieu P, Tron AM, Perrin G, Peschard MJ, Richard M, Vignon E (1997) Phospholipase A2 activity in herniated lumbar discs. Clinical correlations and inhibition by piroxicam. Spine 22:2061–2065
Rosenstiel AK, Keefe FJ (1983) The use of coping strategies in chronic low back pain patients: relationship to patient characteristics and current adjustment. Pain 17:33–44
Tandon V, Campbell F, Ross ER (1999) Posterior lumbar interbody fusion Association between disability and psychological disturbance in noncompensation patients. Spine 24:1833–1838
Taylor SJ, Taylor AE, Foy MA, Fogg AJ (1999) Responsiveness of common outcome measures for patients with low back pain. Spine 24:1805–1812
Thomsen K, Christensen FB, Eiskjaer SP, Hansen ES, Fruensgaard S, Bunger CE (1997) 1997 Volvo Award winner in clinical studies. The effect of pedicle screw instrumentation on functional outcome and fusion rates in posterolateral lumbar spinal fusion: a prospective, randomized clinical study. Spine 22:2813–2822
Trief PM, Grant W, Fredrickson B (2000) A prospective study of psychological predictors of lumbar surgery outcome. Spine 25:2616–2621
Waddell G, Newton M, Henderson I, Somerville D, Main CJ (1993) A fear-avoidance beliefs questionnaire (FABQ) and the role of fear-avoidance beliefs in chronic low back pain and disability. Pain 52:157–168
Walsh TL, Hanscom B, Lurie JD, Weinstein JN (2003) Is a condition-specific instrument for patients with low back pain/leg symptoms really necessary? The responsiveness of the Oswestry Disability Index, MODEMS, and the SF-36. Spine 28:607–615
Author information
Authors and Affiliations
Corresponding author
Appendix: Development, reproducibility and choice of classification scheme
Appendix: Development, reproducibility and choice of classification scheme
Original scoring of the classification
First, the original continuous visual analogue scale ranging from 0 to 140 was divided and transformed into a numerical scale ranging from 0 to 10. Next, two summary variables, Sum1 and Sum2, were created. The first is calculated as the sum of the numerical scores of question 1 to question 10. The second was calculated as the sum of the numerical scores of question 11 to question 16. Based on these two sum scores, the groups are defined as:
-
Group 4: Sum1 + (3×Sum2) ≥ 132
-
Group 3: Not belonging to group 4 and Sum1 + (1/2)×Sum2 ≥ 49
-
Group 2: Not belonging to group 4 or 3 and Sum1+(1/3)×Sum2 ≥ 22
-
Group 1: Sum1 + (1/3)Sum2 < 22.
Principal component and hierarchical cluster analysis
Using SPSS for Windows 11.0, a principal component analysis of the 16 items from the DPQ was performed extracting two factors. After the VAS-based score had been transformed, we used the raw data with no weighting so that the scores would mimic a 0–10 numerical scale.
The loading plot derived from the analysis is seen in Fig. 3. It closely resembles the loading plot shown in the article by Ozguler et al. with the exception of item 15, which is the question regarding social support.
Hierarchical cluster analysis was performed using the individual values of the two extracted factors. The analysis was set to extract four clusters using the ward method. The four clusters were relatively distinct and could be separated visually by three straight lines (Fig. 4). This resulted in classification of the groups in accordance with the following rules:\( \begin{aligned} {\text{Group}}\;{\text{1:}}\;{\text{Sum1}} - 2\tfrac{2} {3}{\text{Sum2}} > - 14\tfrac{2} {3}\;{\text{\& }}\;{\text{Sum1}} - \tfrac{5} {6}{\text{Sum2}} < {\text{43}}\tfrac{1} {3} & \\ {\text{Group}}\;2{\text{:}}\;{\text{Sum1}} - 2\tfrac{2} {3}{\text{ Sum2 > }} - 14\tfrac{2} {3}\;{\text{\& }}\;{\text{Sum1}} - \tfrac{5} {6}{\text{Sum2}} \geqslant {\text{43}}\tfrac{1} {3} & \\ {\text{Group}}\;3{\text{:}}\;{\text{Sum1}} - 2\tfrac{2} {3}{\text{ Sum2}} \leqslant - 14\tfrac{2} {3}\;{\text{\& }}\;{\text{Sum1}} - \tfrac{5} {6}{\text{Sum2 < 35}} & \\ {\text{Group}}\;4{\text{:}}\;{\text{Sum1}} - 2\tfrac{2} {3}{\text{ Sum2}} \leqslant - 14\tfrac{2} {3}\;{\text{\& }}\;{\text{Sum1}} - \tfrac{5} {6}{\text{Sum2}} \geqslant {\text{35}} & \\ \end{aligned} \) This classification resulted in a misclassification of 11.5% of the patients, but with good agreement between the cluster analysis classes and the practical classification (Table 8). When compared with the classification by Ozguler et al. there was very poor agreement (Table 9).
Differences between the two classification schemes
As compared to the result obtained by Ozguler et al., we found a similar result in the principal component analysis with one exception: while question 15 regarding social support correlated positively with both components, it correlated weakly with component 2. Ozguler et al. found it to correlate negatively with the second component. This implies that it might not reflect emotional capacities but more likely physical capacities. As it is included in the calculation of the second summary score, this might be one reason for the difference obtained in our hierarchical cluster analysis as compared to the result of Ozguler et al. The distribution of the four clusters was, however, very similar to that seen in Fig. 4 if the analysis was done based only on the other 15 questions in the DPQ (data not shown). Similarly, no difference in the distribution was seen if the clusters were plotted not according to Sum1 and Sum2 but instead to the sums of questions 1–10 + 15 and questions 11–14 + 16 (data not shown). Thus, it seems unlikely that the difference between the two classification schemes is fully attributable to the different loading of question 15 in the principal component analysis.
Another explanation for the difference could be that Ozguler et al. developed their classification on a patient sample with a broader range of disability. Comparing Fig. 4 with the corresponding figure from the paper by Ozguler et al., it is evident that our patient sample is somewhat skewed toward the higher values of the two sum scores. The lack of patients with low values of the two summary scores in our sample could explain the different results obtained by the hierarchical cluster analysis in our study. Additionally, Ozguler et al. used the DPQ with numerical 0–10 scales instead of the original VAS-scales used in our version of the questionnaire.
Comparison of classification schemes
Using the classification by Ozguler et al., the four groups differ due to a graduated increase in the value of the first summary score (increased level of physical disability) whereas the increase in the second summary score (emotional capacities) is much lower except for those in group 4 (In Fig. 2 in the paper by Ozguler et al., they are classified by the line labelled C, which is almost horizontal, displaying the addition of emotional disturbance characterising this group). Using the classification based on our sample, there is a more linear increase in both the sum scores. Thus, it is not possible to isolate a group that differs much in relation to emotional disturbance.
Using the subjective evaluation of the patient as outcome, logistic regression was performed using the same predictive variables as in the article, except for the variable “preoperative classification”, which was now based on the classification developed using our patient sample. The resulting ORs were almost identical, except that when using the classification based on our patient sample, preoperative classification did not remain in the model (data not shown).
Choice of classification scheme
We chose to use the original classification despite the fact that we could not reproduce the classification in our patient sample. We did so because the original classification was developed on a larger patient sample with a broader range of disability; furthermore, we find the interpretation of the original classification straighter and more intuitive in comparison with the classification based on our analysis. We observed no predictive value of the classification based on our analysis with respect to subjective outcome after fusion surgery. We are of the opinion that the original classification is robust, that it can handle differences due to different language versions and that it gives meaningful and valuable information also, in relation to spinal fusion patients.
Rights and permissions
About this article
Cite this article
Andersen, T., Christensen, F.B. & Bünger, C. Evaluation of a Dallas Pain Questionnaire classification in relation to outcome in lumbar spinal fusion. Eur Spine J 15, 1671–1685 (2006). https://doi.org/10.1007/s00586-005-0046-z
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00586-005-0046-z