Abstract
Purpose
Spondylodiscitis mainly affects the anterior part of the spine. In this paper, we retrospectively analyze our experience with the anterior stand-alone approach (ASAA) in the treatment of spinal infections.
Methods
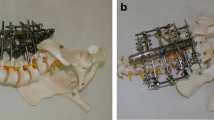
Forty consecutive patients with severe spondylodiscitis underwent the ASAA during the acute infective phase. Treatment consisted of disease debridement, vertebral body reconstruction using titanium expandable prostheses and anterior fixation.
Results
There was neither mortality nor major morbidity. Successful arthrodesis was achieved in 39 out of 40 patients who remained disease free throughout the follow-up period. Six months after treatment, one patient experienced pseudarthrosis and required supplemented posterior spinal fixation for vertebral instability. However, adequate arthrodesis was eventually obtained even in this patient.
Conclusions
ASAA with spine reconstruction using synthetic materials during the acute infection phase was safe and effective. The infections were rapidly defeated, the patients were allowed to stand up early after the procedure and the length of hospital stay was significantly reduced.






Similar content being viewed by others
References
Hodgson AR, Stock FE, Fang HS, Ong GB (1960) Anterior spinal fusion. The operative approach and pathological findings in 412 patients with Pott’s disease of the spine. Br J Surg 48:172–178
Krodel A, Sturz H (1989) Differentiated surgical and conservative treatment of spondylitis and spondylodiscitis. Z Orthop Ihre Grenzbeg 127:587–596 in German
Eismont FJ, Bohlman HH, Soni PL, Goldberg VM, Freehafer AA (1983) Pyogenic and fungal vertebral osteomyelitis with paralysis. J Bone Joint Surg Am 65:19–29
Calderone RR, Larsen JM (1996) Overview and classification of spinal infections. Orthop Clin North Am 27:1–8
D’Aliberti G, Talamonti G, Villa F, Debernardi A, Sansalone CV, LaMaida A, Torre M, Collice M (2008) Anterior approach to thoracic and lumbar spine lesions: results in 145 consecutive cases. J Neurosurg Spine 9:466–482
Chang CC, Merritt K (1994) Infection at the site of implanted materials with and without preadhered bacteria. J Orthop Res 12:526–531
American Spinal Cord Injury Association (1992) Standards for neurological and functional classification of spinal cord injury, revised. Americal Spinal Cord Injury Association, Chicago
Denis F, Armstrong GW, Searls K, Matta L (1984) Acute thoracolumbar burst fractures in the absence of neurologic deficit. A comparison between operative and nonoperative treatment. Clin Orthop Relat Res 189:142–149
Kim KD, Johnson PJ, Masciopinto JE (1999) Management of spinal epidural abscess and subdural empyema. Tech Neurosurg 5:293–302
McHenry MC, Easley KA, Locker GA (2002) Vertebral osteomyelitis: long-term outcome for 253 patients from 7 Cleveland-area hospitals. Clin Infect Dis 34:1342–1350
Hsieh P, Wienecke RJ, O’Shaughnessy BA, Koski TR, Ondra SL (2004) Surgical strategies for vertebral osteomyelitis and epidural abscess. Neurosurg Focus 17:E4
Turgut M (2001) Spinal tuberculosis (Pott’s disease): its clinical presentation, surgical management, and outcome. A survey study on 694 patients. Neurosurg Rev 24:8–13
Ruf M, Strolze D, Merck RH, Ames M, Harms J (2007) Treatment of vertebral osteomyelitis by radical debridement and stabilization using titanium mesh cage. Spine 32:E275–E280
Kuklo TR, Potter BK, Bell SB, Moquin RR, Rosner MK (2006) Single-stage treatment of pyogenic spinal infection with titanium mesh cages. J Spinal Disord Tech 19:376–382
Sundararaj GD, Behera S, Ravi V, Venkatesh K, Cherian VM, Lee V (2003) Role of posterior stabilization in the management of tuberculosis of the dorsal and lumbar spine. J Bone Joint Surg Br 85:100–106
Yilmaz C, Selek HY, Gurkan I, Erdemli B, Korkusuz Z (1999) Anterior instrumentation for the treatment of spinal tuberculosis. J Bone Joint Surg Am 81:1261–1267
Dvorak MF, Known BK, Fisher CG, Eiserloh HL, Boyd M, Wing PC (2003) Effectiveness of titanium mesh cylindrical cages in anterior column reconstruction after thoracic and lumbar vertebral body resection. Spine 28:902–908
Grob D, Daehn S, Mannion AF (2005) Titanium mesh cages (TMC) in spine surgery. Eur Spine J 14:211–221
Ecklund JM, Depper MH, Zeidman SM (1999) Pyogenic vertebral osteomyelitis. Tech Neurosurg 5:282–292
Moon MS, Woo YK, Lee KS, Ha KY, Kim SS, Sun DH (1995) Posterior instrumentation and anterior interbody fusion for tuberculous kyphosis of dorsal and lumbar spines. Spine 20:1910–1916
Emery SE, Chan DP, Woodward HR (1989) Treatment of hematogenous pyogenic vertebral osteomyelitis with anterior debridement and primary bone grafting. Spine 14:284–291
Krodel A, Kruger A, Lohscheidt K, Pfahler M, Reflor HJ (1999) Anterior debridement, fusion, and extrafocal stabilization in the treatment of osteomyelitis of the spine. J Spinal Disord 12:17–26
Klockner C, Valencia R (2003) Sagittal alignment after anterior debridement and fusion with or without additional posterior instrumentation in the treatment of pyogenic and tuberculous spondylodiscitis. Spine 28:1036–1042
Safran O, Rand N, Kaplan L, Sagiv S, Floman Y (1998) Sequential or simultaneous, same-day anterior decompression and posterior stabilization in the management of vertebral osteomyelitis of the lumbar spine. Spine 23:1885–1890
McDonnel DE, Harrison SJ (1998) Lateral approach to the craniocervical complex. Tech Neurosurg 4:306–318
Conflict of interest
None.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
D’Aliberti, G., Talamonti, G., Villa, F. et al. The anterior stand-alone approach (ASAA) during the acute phase of spondylodiscitis: results in 40 consecutively treated patients. Eur Spine J 21 (Suppl 1), 75–82 (2012). https://doi.org/10.1007/s00586-012-2238-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00586-012-2238-7