Abstract
Introduction
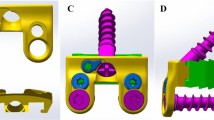
Anterior cervical decompression and fusion is a well-established procedure for treatment of degenerative disc disease and cervical trauma including flexion-distraction injuries. Low-profile interbody devices incorporating fixation have been introduced to avoid potential issues associated with dissection and traditional instrumentation. While these devices have been assessed in traditional models, they have not been evaluated in the setting of traumatic spine injury. This study investigated the ability of these devices to stabilize the subaxial cervical spine in the presence of flexion-distraction injuries of increasing severity.
Methods
Thirteen human cadaveric subaxial cervical spines (C3–C7) were tested at C5–C6 in flexion–extension, lateral bending and axial rotation in the load-control mode under ±1.5 Nm moments. Six spines were tested with locked screw configuration and seven with variable angle screw configuration. After testing the range of motion (ROM) with implanted device, progressive posterior destabilization was performed in 3 stages at C5–C6.
Results
The anchored spacer device with locked screw configuration significantly reduced C5–C6 flexion–extension (FE) motion from 14.8 ± 4.2 to 3.9 ± 1.8°, lateral bending (LB) from 10.3 ± 2.0 to 1.6 ± 0.8, and axial rotation (AR) from 11.0 ± 2.4 to 2.5 ± 0.8 compared with intact under (p < 0.01). The anchored spacer device with variable angle screw configuration also significantly reduced C5–C6 FE motion from 10.7 ± 1.7 to 5.5 ± 2.5°, LB from 8.3 ± 1.4 to 2.7 ± 1.0, and AR from 8.8 ± 2.7 to 4.6 ± 1.3 compared with intact (p < 0.01). The ROM of the C5–C6 segment with locked screw configuration and grade-3 F-D injury was significantly reduced from intact, with residual motions of 5.1 ± 2.1 in FE, 2.0 ± 1.1 in LB, and 3.3 ± 1.4 in AR. Conversely, the ROM of the C5–C6 segment with variable-angle screw configuration and grade-3 F-D injury was not significantly reduced from intact, with residual motions of 8.7 ± 4.5 in FE, 5.0 ± 1.6 in LB, and 9.5 ± 4.6 in AR.
Conclusions
The locked screw spacer showed significantly reduced motion compared with the intact spine even in the setting of progressive flexion-distraction injury. The variable angle screw spacer did not sufficiently stabilize flexion–distraction injuries. The resulting motion for both constructs was higher than that reported in previous studies using traditional plating. Locked screw spacers may be utilized with additional external immobilization while variable angle screw spacers should not be used in patients with flexion-distraction injuries.



Similar content being viewed by others
References
Robinson RA (1963) The problem of neck pain: its alleviation by anterior removal of intervertebral disc with interbody fusion in the cervical spine. J Med Assoc State Ala 33:1–14
Smith GW, Robinson RA (1958) The treatment of certain cervical-spine disorders by anterior removal of the intervertebral disc and interbody fusion. J Bone Joint Surg Am 40-A(3):607–624
Frempong-Boadu A, Houten JK, Osborn B, Opulencia J, Kells L, Guida DD, Le Roux PD (2002) Swallowing and speech dysfunction in patients undergoing anterior cervical discectomy and fusion: a prospective, objective preoperative and postoperative assessment. J Spinal Disord Tech 15(5):362–368
Lee MJ, Bazaz R, Furey CG, Yoo J (2005) Influence of anterior cervical plate design on dysphagia: a 2-year prospective longitudinal follow-up study. J Spinal Disord Tech 18(5):406–409. doi:10.1097/01.bsd.0000177211.44960.71
Scholz M, Reyes PM, Schleicher P, Sawa AG, Baek S, Kandziora F, Marciano FF, Crawford NR (2009) A new stand-alone cervical anterior interbody fusion device: biomechanical comparison with established anterior cervical fixation devices. Spine 34(2):156–160. doi:10.1097/BRS.0b013e31818ff9c4
Balaram AGA, O’Leary P, Voronov L, Havey R, Carandang G, Abjornson C, Patwardhan A (2009) Biomechanical evaluation of a low profile, anchored cervical interbody spacer device at the index level or adjacent to plated fusion. Paper presented at the Cervical Spine Research Society, Salt Lake City, 3–5 Dec, 2009
Patwardhan AG, Havey RM, Ghanayem AJ, Diener H, Meade KP, Dunlap B, Hodges SD (2000) Load-carrying capacity of the human cervical spine in compression is increased under a follower load. Spine 25(12):1548–1554
Patwardhan AG, Havey RM, Carandang G, Simonds J, Voronov LI, Ghanayem AJ, Meade KP, Gavin TM, Paxinos O (2003) Effect of compressive follower preload on the flexion-extension response of the human lumbar spine. J Orthop Res 21(3):540–546. doi:10.1016/S0736-0266(02)00202-4
Allen BL Jr, Ferguson RL, Lehmann TR, O’Brien RP (1982) A mechanistic classification of closed, indirect fractures and dislocations of the lower cervical spine. Spine 7(1):1–27
Vaccaro AR, Madigan L, Schweitzer ME, Flanders AE, Hilibrand AS, Albert TJ (2001) Magnetic resonance imaging analysis of soft tissue disruption after flexion-distraction injuries of the subaxial cervical spine. Spine 26(17):1866–1872
Paxinos O, Ghanayem AJ, Zindrick MR, Voronov LI, Havey RM, Carandang G, Hadjipavlou A, Patwardhan AG (2009) Anterior cervical discectomy and fusion with a locked plate and wedged graft effectively stabilizes flexion-distraction stage-3 injury in the lower cervical spine: a biomechanical study. Spine 34(1):E9–E15. doi:10.1097/BRS.0b013e318188386a
Kaiser MG, Haid Jr. RW, Subach BR, Barnes B, Rodts Jr. GE (2002) Anterior cervical plating enhances arthrodesis after discectomy and fusion with cortical allograft. Neurosurgery 50(2):229–236; discussion 236–238
Song KJ, Taghavi CE, Hsu MS, Lee KB, Kim GH, Song JH (2010) Plate augmentation in anterior cervical discectomy and fusion with cage for degenerative cervical spinal disorders. Eur Spine J 19(10):1677–1683. doi:10.1007/s00586-010-1283-3
Lu DC, Theodore P, Korn WM, Chou D (2008) Esophageal erosion 9 years after anterior cervical plate implantation. Surg Neurol 69(3):310–312; discussion 312–313. doi:10.1016/j.surneu.2007.02.037
Winslow CP, Winslow TJ, Wax MK (2001) Dysphonia and dysphagia following the anterior approach to the cervical spine. Arch Otolaryngol Head Neck Surg 127(1):51–55
Kuo YC, Levine MS (2010) Erosion of anterior cervical plate into pharynx with pharyngotracheal fistula. Dysphagia. doi:10.1007/s00455-009-9271-7
Daniels AH, Riew KD, Yoo JU, Ching A, Birchard KR, Kranenburg AJ, Hart RA (2008) Adverse events associated with anterior cervical spine surgery. J Am Acad Orthop Surg 16(12):729–738
Hilibrand AS, Robbins M (2004) Adjacent segment degeneration and adjacent segment disease: the consequences of spinal fusion? Spine J 4(6 Suppl):190S–194S. doi:10.1016/j.spinee.2004.07.007
Ishihara H, Kanamori M, Kawaguchi Y, Nakamura H, Kimura T (2004) Adjacent segment disease after anterior cervical interbody fusion. Spine J 4(6):624–628. doi:10.1016/j.spinee.2004.04.011
Hilibrand AS, Carlson GD, Palumbo MA, Jones PK, Bohlman HH (1999) Radiculopathy and myelopathy at segments adjacent to the site of a previous anterior cervical arthrodesis. J Bone Joint Surg Am 81(4):519–528
Yang JY, Song HS, Lee M, Bohlman HH, Riew KD (2009) Adjacent level ossification development after anterior cervical fusion without plate fixation. Spine 34(1):30–33. doi:10.1097/BRS.0b013e318190d833
Park JB, Watthanaaphisit T, Riew KD (2007) Timing of development of adjacent-level ossification after anterior cervical arthrodesis with plates. Spine J 7(6):633–636. doi:10.1016/j.spinee.2006.10.021
Bozkus H, Ames CP, Chamberlain RH, Nottmeier EW, Sonntag VK, Papadopoulos SM, Crawford NR (2005) Biomechanical analysis of rigid stabilization techniques for three-column injury in the lower cervical spine. Spine 30(8):915–922. doi:10.1097/01.brs.0000158949.37281.d7
Do Koh Y, Lim TH, Won You J, Eck J, An HS (2001) A biomechanical comparison of modern anterior and posterior plate fixation of the cervical spine. Spine 26(1):15–21
Pitzen T, Lane C, Goertzen D, Dvorak M, Fisher C, Barbier D, Steudel WI, Oxland T (2003) Anterior cervical plate fixation: biomechanical effectiveness as a function of posterior element injury. J Neurosurg 99(1 Suppl):84–90
Bohler J, Gaudernak T (1980) Anterior plate stabilization for fracture-dislocations of the lower cervical spine. J Trauma 20(3):203–205
Henriques T, Olerud C, Bergman A, Jonsson H Jr (2004) Distractive flexion injuries of the subaxial cervical spine treated with anterior plate alone. J Spinal Disord Tech 17(1):1–7. doi:10.1097/00024720-200402000-00002
Lambiris E, Zouboulis P, Tyllianakis M, Panagiotopoulos E (2003) Anterior surgery for unstable lower cervical spine injuries. Clin Orthop Relat Res 411:61–69. doi:10.1097/01.blo.0000068185.83581.cf
Razack N, Green BA, Levi AD (2000) The management of traumatic cervical bilateral facet fracture-dislocations with unicortical anterior plates. J Spinal Disord 13(5):374–381
Goffin J, Plets C, Van den Bergh R (1989) Anterior cervical fusion and osteosynthetic stabilization according to Caspar: a prospective study of 41 patients with fractures and/or dislocations of the cervical spine. Neurosurgery 25(6):865–871
Brodke DS, Anderson PA, Newell DW, Grady MS, Chapman JR (2003) Comparison of anterior and posterior approaches in cervical spinal cord injuries. J Spinal Disord Tech 16(3):229–235
Goffin J, van Loon J, Van Calenbergh F, Plets C (1995) Long-term results after anterior cervical fusion and osteosynthetic stabilization for fractures and/or dislocations of the cervical spine. J Spinal Disord 8(6):500–508; discussion 499
Woodworth RS, Molinari WJ, Brandenstein D, Gruhn W, Molinari RW (2009) Anterior cervical discectomy and fusion with structural allograft and plates for the treatment of unstable posterior cervical spine injuries. J Neurosurg Spine 10(2):93–101. doi:10.3171/2008.11.SPI08615
Garvey TA, Eismont FJ, Roberti LJ (1992) Anterior decompression, structural bone grafting, and caspar plate stabilization for unstable cervical spine fractures and/or dislocations. Spine 17(10 Suppl):S431–S435
Mourning D, Reitman CA, Heggeness MH, Esses SI, Hipp JA (2007) Initial intervertebral stability after anterior cervical discectomy and fusion with plating. Spine J 7(6):643–646. doi:10.1016/j.spinee.2006.10.024
Fielding JW (1988) The status of arthrodesis of the cervical spine. J Bone Joint Surg Am 70(10):1571–1574
Acknowledgments
Supported by the Department of Veterans Affairs, Washington, DC, USA and Synthes Spine, Inc., West Chester, PA, USA.
Conflict of interest
None.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Wojewnik, B., Ghanayem, A.J., Tsitsopoulos, P.P. et al. Biomechanical evaluation of a low profile, anchored cervical interbody spacer device in the setting of progressive flexion-distraction injury of the cervical spine. Eur Spine J 22, 135–141 (2013). https://doi.org/10.1007/s00586-012-2446-1
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00586-012-2446-1