Abstract
Purpose
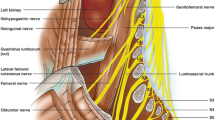
XLIF® is a widely used minimally invasive technique to treat different spine pathologies. The aim of this study was to quantify nerve distortion of lumbar plexus during XLIF® approach and to correlate it with morphometric data.
Methods
Nine fresh frozen cadaveric specimens were used. All specimens were subjected to the same dissection procedure cored on a left XLIF® approach at L2/L3 and L4/L5 levels. Distortion of cutaneous superficial nerves, femoral nerve (FN) at L4/L5 and genitofemoral nerve (GN) at L2/L3 and L4/L5 while opening the retractor were assessed and analyzed with respect to psoas muscle features.
Results
Superficial nerves were slightly displaced but never stretched. FN, as well as GN at L4/L5 level, could be displaced and stretched by the blades. Statistically significant correlation between FN distortion and the amount of psoas fibers interposed between the posterior blade of the retractor and the nerve itself (TCK) was found. GN distortion was found to be related to its clock position on an axial section of psoas muscle seen from cranially at L4/L5.
Conclusion
FN was in close connection with the deep psoas muscle fibers and it is subjected to anterior translation that correlates with TCK. This mechanism may partly explain the rate of femoral nerve palsy that occurs despite neuromonitoring and safe entry zones respect. The GN location at L4/L5 should be considered not only for its projection in Zone I, but also for its clock position on the psoas muscle surface, since it affects its distortion.









Similar content being viewed by others
References
Pimenta L (2001) Lateral endoscopic transpsoas retroperitoneal approach for lumbar spine surgery. In: VIII Brazilian Spine Society Meeting. Belo Horizonte, Minas Gerais, Brazil
Ozgur BM, Aryan HE, Pimenta L, Taylor WR (2006) Extreme lateral interbody fusion (XLIF): a novel surgical technique for anterior lumbar interbody fusion. Spine J Off J North Am Spine Soc 6:435–443. doi:10.1016/j.spinee.2005.08.012
Berjano P, Lamartina C (2013) Far lateral approaches (XLIF) in adult scoliosis. Euro Spine J Off Publ Euro Spine Soc Euro Spinal Deform Soc Euro Section Cervical Spine Res Soc 22(Suppl 2):S242–S253. doi:10.1007/s00586-012-2426-5
Caputo AM, Michael KW, Chapman TM, Jennings JM, Hubbard EW, Isaacs RE, Brown CR (2013) Extreme lateral interbody fusion for the treatment of adult degenerative scoliosis. J Clin Neurosci Off J Neurosurgery Soc Austral 20:1558–1563. doi:10.1016/j.jocn.2012.12.024
Paulino CPA, Carrer A (2010) Anatomical considerations for the extreme lateral (XLIF) approach. Curr Orthop Pract 21:7
Ozgur BM, Agarwal V, Nail E, Pimenta L (2010) Two-year clinical and radiographic success of minimally invasive lateral transpsoas approach for the treatment of degenerative lumbar conditions. SAS J 4:41–46. doi:10.1016/j.esas.2010.03.005
Dakwar E, Vale FL, Uribe JS (2011) Trajectory of the main sensory and motor branches of the lumbar plexus outside the psoas muscle related to the lateral retroperitoneal transpsoas approach. J Neurosurg Spine 14:290–295. doi:10.3171/2010.10.SPINE10395
Uribe JS, Arredondo N, Dakwar E, Vale FL (2010) Defining the safe working zones using the minimally invasive lateral retroperitoneal transpsoas approach: an anatomical study. J Neurosurg Spine 13:260–266. doi:10.3171/2010.3.SPINE09766
Moro T, Kikuchi S, Konno S, Yaginuma H (2003) An anatomic study of the lumbar plexus with respect to retroperitoneal endoscopic surgery. Spine 28:423–428. doi:10.1097/01.BRS.0000049226.87064.3B (discussion 427–428)
Regev GJ, Chen L, Dhawan M, Lee YP, Garfin SR, Kim CW (2009) Morphometric analysis of the ventral nerve roots and retroperitoneal vessels with respect to the minimally invasive lateral approach in normal and deformed spines. Spine 34:1330–1335. doi:10.1097/BRS.0b013e3181a029e1
Benglis DM, Vanni S, Levi AD (2009) An anatomical study of the lumbosacral plexus as related to the minimally invasive transpsoas approach to the lumbar spine. J Neurosurg Spine 10:139–144. doi:10.3171/2008.10.SPI08479
Park DK, Lee MJ, Lin EL, Singh K, An HS, Phillips FM (2010) The relationship of intrapsoas nerves during a transpsoas approach to the lumbar spine: anatomic study. J Spinal Disorders Techniq 23:223–228. doi:10.1097/BSD.0b013e3181a9d540
Banagan K, Gelb D, Poelstra K, Ludwig S (2011) Anatomic mapping of lumbar nerve roots during a direct lateral transpsoas approach to the spine: a cadaveric study. Spine 36:E687–E691. doi:10.1097/BRS.0b013e3181ec5911
Davis TT, Bae HW, Mok JM, Rasouli A, Delamarter RB (2011) Lumbar plexus anatomy within the psoas muscle: implications for the transpsoas lateral approach to the L4–L5 disc. J Bone Joint Surg Am 93:1482–1487. doi:10.2106/JBJS.J.00962
Guerin P, Obeid I, Gille O, Bourghli A, Luc S, Pointillart V, Cursolle JC, Vital JM (2011) Safe working zones using the minimally invasive lateral retroperitoneal transpsoas approach: a morphometric study. Surg Radiol Anat SRA 33:665–671. doi:10.1007/s00276-011-0798-6
Lu S, Chang S, Zhang YZ, Ding ZH, Xu XM, Xu YQ (2011) Clinical anatomy and 3D virtual reconstruction of the lumbar plexus with respect to lumbar surgery. BMC Musculoskel Disorders 12:76. doi:10.1186/1471-2474-12-76
Guerin P, Obeid I, Bourghli A, Masquefa T, Luc S, Gille O, Pointillart V, Vital JM (2012) The lumbosacral plexus: anatomic considerations for minimally invasive retroperitoneal transpsoas approach. Surg Radiol Anat SRA 34:151–157. doi:10.1007/s00276-011-0881-z
Yusof MI, Nadarajan E, Abdullah MS (2014) The morphometric study of l3-L4 and L4-L5 lumbar spine in Asian population using magnetic resonance imaging: feasibility analysis for transpsoas lumbar interbody fusion. Spine 39:E811–E816. doi:10.1097/BRS.0000000000000368
Rodgers WB, Gerber EJ, Patterson J (2011) Intraoperative and early postoperative complications in extreme lateral interbody fusion: an analysis of 600 cases. Spine 36:26–32. doi:10.1097/BRS.0b013e3181e1040a
Ahmadian A, Deukmedjian AR, Abel N, Dakwar E, Uribe JS (2013) Analysis of lumbar plexopathies and nerve injury after lateral retroperitoneal transpsoas approach: diagnostic standardization. J Neurosurg Spine 18:289–297. doi:10.3171/2012.11.SPINE12755
Houten JK, Alexandre LC, Nasser R, Wollowick AL (2011) Nerve injury during the transpsoas approach for lumbar fusion. J Neurosurg Spine 15:280–284. doi:10.3171/2011.4.SPINE1127
Lehmen JA, Gerber EJ (2015) MIS lateral spine surgery: a systematic literature review of complications, outcomes, and economics. Euro Spine J Off Publ Euro Spine Soc Euro Spinal Deform Soc Euro Section Cervical Spine Res Soc 24(Suppl 3):287–313. doi:10.1007/s00586-015-3886-1
Grimm BD, Leas DP, Poletti SC, Johnson DR 2nd (2014) Postoperative Complications Within the First Year After Extreme Lateral Interbody Fusion: Experience of the First 108 Patients. J Spinal Disorders Techn. doi:10.1097/BSD.0000000000000121
O’Brien J, Haines C, Dooley ZA, Turner AW, Jackson D (2014) Femoral nerve strain at L4–L5 is minimized by hip flexion and increased by table break when performing lateral interbody fusion. Spine 39:33–38. doi:10.1097/BRS.0000000000000039
Reinpold W, Schroeder AD, Schroeder M, Berger C, Rohr M, Wehrenberg U (2015) Retroperitoneal anatomy of the iliohypogastric, ilioinguinal, genitofemoral, and lateral femoral cutaneous nerve: consequences for prevention and treatment of chronic inguinodynia. Hernia J Hernias Abdominal Wall Surg 19:539–548. doi:10.1007/s10029-015-1396-z
Geh N, Schultz M, Yang L, Zeller J (2015) Retroperitoneal course of iliohypogastric, ilioinguinal, and genitofemoral nerves: a study to improve identification and excision during triple neurectomy. Clin Anat 28:903–909. doi:10.1002/ca.22592
Buric J (2015) Relationship between psoas muscle dimensions and post operative thigh pain. A possible preoperative evaluation factor. International journal of spine surgery 9:27. doi:10.14444/2027
He L, Kang Z, Tang WJ, Rong LM (2015) A MRI study of lumbar plexus with respect to the lateral transpsoas approach to the lumbar spine. Euro Spine J Off Publ Euro Spine Soc Euro Spinal Deform Soc Euro Section Cervical Spine Res Soc. doi:10.1007/s00586-015-3847-8
Bendersky M, Sola C, Muntadas J, Gruenberg M, Calligaris S, Mereles M, Valacco M, Bassani J, Nicolas M (2015) Monitoring lumbar plexus integrity in extreme lateral transpsoas approaches to the lumbar spine: a new protocol with anatomical bases. Euro Spine J Off Publ Euro Spine Soc Euro Spinal Deform Soc Euro Section Cervical Spine Res Soc 24:1051–1057. doi:10.1007/s00586-015-3801-9
Uribe JS, Isaacs RE, Youssef JA, Khajavi K, Balzer JR, Kanter AS, Kuelling FA, Peterson MD, Group SDS (2015) Can triggered electromyography monitoring throughout retraction predict postoperative symptomatic neuropraxia after XLIF? Results from a prospective multicenter trial. Euro Spine J Off Publ Euro Spine Soc Euro Spinal Deform Soc Euro Section Cervical Spine Res Soc 24(Suppl 3):378–385. doi:10.1007/s00586-015-3871-8
Acknowledgments
The authors of this work thank Dr Enrico Mandelli (M.S.) for his statistical support.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Funding
NuVasive Inc. funded the study providing the cadavers and the laboratory facilities.
Rights and permissions
About this article
Cite this article
Mandelli, C., Colombo, E.V., Sicuri, G.M. et al. Lumbar plexus nervous distortion in XLIF® approach: an anatomic study. Eur Spine J 25, 4155–4163 (2016). https://doi.org/10.1007/s00586-016-4617-y
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00586-016-4617-y