Abstract
Purpose
Previous studies have demonstrated that total cervical disc replacement (cTDR) represents a viable treatment alternative to the ‘gold standard’ anterior cervical discectomy and fusion for the treatment of well-defined cervical pathologies at short- and mid-term follow-up (FU). However, the implementation and acceptance of a non-fusion philosophy is closely associated with its avoidance of adjacent segment degeneration. Proof of the functional sustainability and clinical improvement of symptoms at long-term FU is still pending. The aim of this ongoing prospective study was to investigate the clinical and radiological results of cTDR at long-term FU.
Methods
50 patients were treated surgically within a non-randomised prospective study framework with cTDR (ProDisc C™, Synthes, Paoli, PA, USA). Patients were examined preoperatively followed by routine clinical and radiological examinations at 1, 5 and 10 years after surgery, respectively. In addition to the clinical scores, conventional X-ray images of the cervical spine were taken in anteroposterior and lateral view as well as flexion/extension images. Clinical outcome scores included parameters such as the Neck Disability Index (NDI), Visual Analogue Scale (VAS), arm and neck pain self-assessment questionnaires as well as subjective patient satisfaction rates. The radiological outcome variables included the range of motion (ROM) of the implanted prosthesis between maximum flexion and extension images, the occurrence of heterotopic ossifications and radiographic signs of adjacent segment degenerative changes. The reoperation rate following cTDR was recorded as a secondary outcome variable.
Results
A significant and maintained clinical improvement of all clinical outcome scores was observed after a mean FU of 10.2 years (VASarm 6.3–2.1; VASneck 6.4–1.9; NDI 21–6; p < 0.05). An increase in the incidence and the extent of heterotopic ossifications was noted during the post-operative course with a significant influence on the function of the prosthesis, which, however, did not reveal any detrimental effect on the patients’ clinical symptomatology. Prosthesis mobility declined from 9.0° preoperatively and 9.1° at 1 year FU to 7.7° and 7.6° at the five- and ten-year FU examinations, respectively. Radiological signs of adjacent segment degeneration were detected in 13/38 (35.7%), however, in only 3/38 (7.9%) patients this radiological changes were associated with clinical symptoms requiring conservative treatment. Intraoperative technical failure in two cases required interbody fusion with a cage (2/50). One patient (1/48, 2.1%) treated this motion device had revision surgery at the index level.
Conclusion
Cervical total disc replacement with ProDisc C demonstrated a significant and maintained improvement of all clinical outcome parameters at a follow-up of ≥10 years. The present long-term data reveal that with an exceptionally low implant-related reoperation rate and low symptomatic adjacent segment degeneration rate, cTDR may be regarded as a safe and viable treatment option.
Similar content being viewed by others
Introduction
Over the past decade, total cervical disc replacement (cTDR) has been established as a viable treatment option for a variety of pathologies at a short- and mid-term follow-up (FU). Clinical studies have demonstrated this procedure to be a viable treatment alternative to the gold standard anterior cervical discectomy and fusion (ACDF) [1,2,3,4,5,6,7,8,9].
However, the underlying fundamental rationale for the development of this technology was to avoid and to reduce the incidence of adjacent segment disease (ASD). As a benchmark reference study, Hilibrand et al. [10] revealed an incidence of 2.9% ASD annually over a ten-year period following ACDF. In their cohort, more than 25% of patients developed adjacent segment degenerative changes within ten years postoperatively, and more than 2/3 of these patients required further surgical intervention due to failed conservative therapy.
To date, only a limited number of long-term studies have investigated the role of cTDR in terms of both clinical results as well as radiographic changes.
The primary aim of this current study was therefore to evaluate the long-term clinical efficacy of this motion preserving technology with ProDisc C™ (Synthes, Paoli, PA, USA). The second goal was to establish whether, after a ten-year period, the prosthesis remains functionally intact and mobile, and to establish whether subsequent adjacent segment degenerative changes can be avoided to a sufficient extent.
Materials and methods
Study design
Within the framework of a prospective, non-randomised study, all patients who were treated with a ProDisc C™ artificial disc prosthesis at a single large spine center between 10/2003 and 08/2005 were consecutively included in this study following their written consent. The investigation included pre-operative data as well as 1-, 5- and 10-year post-operative FU results.
The inclusion and exclusion criteria of this study were clearly defined prior to the initiation of this study (Table 1). Primary inclusion criteria included cervical degenerative disc disease and clinical symptoms of nerve root compression associated with intractable radiculopathy with and without neurological deficits between the levels C3/4 to C6/7, which had proven unresponsive to non-operative treatment.
Clinical, radiological and socio-economic outcome parameters were determined by means of self-assessment questionnaires, NDI (Neck Disability Index), VAS (Visual Analogue Score) arm and neck pain and were completed by all patients individually. Standardized questions relating to patient satisfaction and employment status were likewise completed at each FU stage of the investigation.
Radiological examinations entailed X-ray images of the cervical spine in two planes as well as flexion/extension images. Measurements of the prosthesis range of motion (ROM) as well as of the adjacent segments disc space heights were performed with Impax software (IMPAX EE, Agfa Healthcare N.V.).
The extent of heterotopic ossifications (HO) was graded according to the modified McAfee classification system for lumbar disc prostheses as previously described by Mehren/Suchomel et al. (Table 2) [11].
The measurement of the prosthesis’ long-term mobility, the grading of HO and of adjacent segment degeneration (ASD) was performed by two independent observers. Adjacent segment degeneration was recorded in the presence of radiographic anomalies such as the occurrence of osteophyte formations, reduced height of the intervertebral disc space or a pathological increase of the segmental mobility in comparison to the pre-operative images.
In contrast to the work of Hilibrand et al. [10], an post-operative MRI investigation of the cervical spine was not routinely included in the present study.
Implant and surgical technique
The ProDisc C™ implant (Synthes Inc., Paoli, PA, USA), which was used exclusively in this study, was the first generation of a metal-on-polyethylene, ball-and-socket type articulating device. Primary stability is provided by keels which are attached to the endplates and which fit into a chiseled slot in the cranial and caudal adjacent vertebral bodies. Long-term stability is provided by a plasma-sprayed titanium surface which is intended to promote secondary bony ingrowth. A right-sided anterolateral, microsurgically modified approach was routinely used as the surgical access as previously described by Caspar et al. [12].
The discectomy and decompression of the spinal canal was performed with the assistance of a surgical microscope.
The midline was marked under a-p fluoroscopy. The segment was held in distraction by retaining screws. A trial implant with the appropriate footprint and height was adequately placed in the intervertebral space. The slots for the keels were chiseled, guided by the trial implant, which was followed by the final insertion of the device into the prepared disc space. Bone wax was used to seal the holes of the retaining screws, but not for other open bony surfaces due to the keel-based implantation mechanism. With regards to post-operative care, a soft collar was used until wound healing was completed. Non-steroidal anti-inflammatory medication was not used routinely.
Statistical analysis
The level of significance was established using the Wilcoxon test. A p value of less than 0.05 was considered statistically significant. Interobserver reliability was determined using the Dahlberg method. A value of >1 was assumed to represent a statistically sufficient reliability.
Results
Patient characteristics
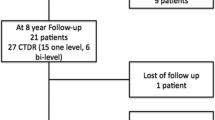
50 patients were initially included in this study. N = 2 patients experienced intraoperative complications with fractures of the posterior wall of the vertebral body, which subsequently required interbody fusion with a cage.
Another patient was excluded at his own request. In this case, the implant had to be replaced ahead of 1-year FU by a cage due to ongoing neck pain and significant psychological distress experienced by the patient.
The average age was 44.8 years (range 25–67 years) with an equal gender distribution (23f/24m). A total of 70 prostheses were implanted from C3/4 to C6/7 as outlined in Table 3.
A monosegmental prosthesis was implanted in 27 cases (57.4%), bisegmental cTDR in 17 cases (36.2%) and a three-segmental disc replacement was performed in n = 3 cases (6.4%), respectively. The mean FU was 10.2 years (range 9.6–11.7 years), with a FU rate of 80.9% (n = 38).
Clinical outcome scores
A statistically significant improvement of VAS and NDI scores was noted at all FU examinations. The VAS for arm and neck pain improved over the entire course of the observation period from 6.3 and 6.4 preoperatively to a stable value of 2.1 and 1.9 at the 10-year FU, respectively (p < 0.005).
Likewise, the NDI revealed a significant improvement (p < 0.005) from 21 points preoperatively to six points at the last FU (Fig. 1).
This highly significant improvement of VAS and NDI scores was reflected in similarly high patient satisfaction rates at the 10-year FU examination. 78.9% (n = 30/38) of all patients reported a highly satisfactory outcome, 21.1% (n = 8/38) a satisfactory outcome and 89.5% (n = 34) of all patients reported that they would, when asked retrospectively, opt to undergo surgery again. The remaining 10.5% (n = 4) of all patients did not wish to provide their subjective outcome.
Up until the final 10-year FU examination, none of the patients had to be re-operated on for symptomatic adjacent segment degeneration. Three patients received conservative treatment including selective fluoroscopically guided spine infiltrations due to symptoms of recurrent neck pain, which provided a sustained improvement of their complaints.
Thus, the overall reoperation rate in this cohort was 2.1% (1/48).
Radiological findings
No cases of prosthesis dislocations were observed in n = 70 implanted devices. A significant subsidence of the cranial implant component was observed in one case where the patient was involved in a motor vehicle accident 6 months after surgery. Conservative therapy and immobilization of the cervical spine with a brace over a 3-month period served to achieve a complete remission of symptoms.
The subsequent course revealed an anterior bony bridging with complete fusion of the affected segment.
The index segment revealed a mean pre-operative ROM (range of motion) of 9.0°. This ROM declined to 7.6° and 7.7° at the 5- and 10-year FU examination, respectively (p = 0.03). The median prosthesis ROM was 9.1° preoperatively, 9.0° at the 1-year FU examination and 7.7° and 7.6° at the 5- and 10-year FU as outlined in Fig. 2, respectively.
In addition, the incidence of heterotopic ossifications had a significant influence on the device mobility from grade 3 HO onwards with significantly reduced ROM values (Fig. 3).
A significantly increasing incidence and severity of heterotopic ossifications was furthermore observed during the post-operative course (Fig. 4). Ultimately, at 10-year FU, grade 0 ossifications were observed in 10% of all cases, grade 1 in 10% of cases, grade 2 in 22% of cases, grade 3 with functional impairment of the prosthesis in 32% of cases and grade 4 with solid fusion of the index segment in 26% of cases.
There was no significant correlation between the occurrence of heterotopic ossifications and the clinical outcome parameters in terms of VAS neck scores up until the 10-year FU (NDI: p = 0.34; VAS arm: p = 0.60).
According to well-defined pre-operative criteria, radiological signs of adjacent segment degeneration (ASD) were observed in 35.7% (n = 13) of all radiologically evaluated cases at the 10-year FU. A cranial ASD was detected in n = 10 cases, and caudal adjacent level degenerative changes in n = 3 cases.
The correlation between the device mobility and the occurrence of ASD is shown in Fig. 5. A highly significant difference can already be detected preoperatively with respect to the prosthesis mobility and the occurrence of ASD at later post-operative FU stages. (p = 0.0024). This discrepancy became even more pronounced in the subsequent long-term course (p < 0.0006).
The radiological changes became clinically symptomatic as an ASD in n = 3 patients with axial neck pain as the leading complaint (n = 3/38; 7.9%). All three patients were treated conservatively. Physiotherapy and fluoroscopically guided spine infiltrations of the adjacent level facet joints led to a satisfactory improvement of the clinical symptomatology. With the exception of the case described above, no secondary revision surgery was necessary for any of the patients right up to the last FU.
Discussion
The effectiveness of cTDR has been under investigation for many years. One of the major challenges for cTDR includes the highly satisfactory clinical results of the “gold standard” treatment ACDF. At short term FU, no significant differences can be found between both technologies as long as the same adequate decompression techniques are performed. Numerous studies have demonstrated, however, that both cTDR and ACDF achieved comparatively similar improvements in all clinical outcome parameters [3, 4, 6, 8, 9, 13, 14]. However, a number of studies demonstrated that at short- and mid-term FU, the rates of post-operative revision surgeries were significantly lower and in favour of cTDR [1, 3, 5, 15]. The underlying reasons for this observation included implant and technique-related issues, which were linked to the fusion of the segments (i.e. non-union, implant subsidence and others). However, the ultimate proof that motion preservation with cTDR devices may result in lower rates of adjacent segment degeneration as well as lower reoperation rates is still pending.
Long-term follow-up of clinical outcome parameters
The present study cohort revealed a significant and maintained improvement of all clinical outcome parameters (NDI, VAS arm, VAS neck) at all post-operative stages in comparison to baseline levels up until the 10-year FU examination.
Similar observations were verified in a number of studies, which demonstrated comparable post-operative scores at different long-term observation periods, ranging between 4 and 30 years, and irrespective of the type of prosthesis used [2,3,4, 16,17,18,19].
However, a systematic review which compared cTDR with ACDF did not detect any relevant differences in disability, pain, general state of health, neurological success and satisfaction parameters at 2 years of FU [13].
These findings can, however, no longer be upheld based on the data from current comparative long-term studies, as previously published RCTs demonstrated statistically significantly superior clinical results for the cTDR group in comparison to the patients treated with ACDF [3, 4]. As an explanation for these findings, the significantly lower long-term revision rates, especially at the adjacent segment, should be taken into consideration. Janssen et al. published their data from a prospective randomised U.S. FDA investigation device exemption study of the Prodisc C with 7 years of follow-up. The authors found similar clinical outcomes between the Prodisc C (n = 103) and ACDF group (n = 106), however, with lower rates of second surgery observed in the cTDR cohort. Loumeau et al. [3] assessed the data from an RCT and compared the results from monosegmental treatments between Prodisc C versus ACDF with 7 years of FU. Revision surgeries had to be carried out in 27% of all cases in the cohort of fusion candidates, 9% thereof at the adjacent segment and 18% at the index segment due to pseudoarthrosis. Conversely, however, no revision surgery was required in the cTDR cohort. In a similar randomised study setting comparing monosegmental fusion with plate versus Prodisc C, Delamater et al. [20] reported somewhat lower reoperation rates at the 5-year FU. The ACDF group demonstrated a five times higher reoperation rate (16/106), mainly due to pseudoarthrosis (6/106) and symptomatic adjacent segment degeneration (8/106).
In comparison, the reoperation rate following total cervical disc replacement appeared to be low with only 2.9% (2/103 revision cases performed at the index segment; 1/103 at the adjacent segment), which was one of the main findings of the study.
In the current study, after an average FU of 10.2 years, only one reoperation was required in a patient with persisting neck pain and concomitant psychological distress, which was referred to the prosthesis and which therefore necessitated a conversion to an ACDF. There were no further cases, which required reoperation due to implant failure or adjacent segment disease. Hisey et al. reported the similar results of a RCT study comparing Mobi C with ACDF at 48 month of follow-up with only 0.6% of patients that underwent subsequent surgery to treat symptoms arising from the adjacent level to the index level in the TDR group in comparison to 3.7% in the fusion group [15].
Therefore, those patients treated with disc prosthesis demonstrated a 2% reoperation rate in this present long-term FU investigation. Including the two cases which required an interbody fusion with a cage resulting from intraoperative complications due to technical failures, the overall “intent to treat” reoperation rate was 3/50 (6%).
This low incidence of revision cases over a long-term FU in particular is one of the key arguments, which promotes the use of cTDR, irrespective of potentially concomitant radiological changes or the occurrence of heterotopic ossifications.
Adjacent segment degeneration
Up until the last FU, after an average of 10.2 years, adjacent segment degenerative changes such as disc height reduction, endplate sclerosis or development of spondylophytes were observed in 35.7% of all patients that were available for radiological assessment (n = 13/38). This rate of adjacent level degenerative changes does not differ substantially from the repeatedly cited work from Hilibrand et al. [10] with respect to the annual incidence of 2.9% of an adjacent segment degeneration following fusion.
Nunley et al. [21] previously reported similar observations. After a median of 4 years of FU, the authors reported symptomatic ASD following total cervical disc replacement with an annual incidence of 3.1%. Jawahar et al. [22] also reported a comparable incidence of ASD. In a RCT, 93 patients were included (59 cTDR versus 34 cases of ACDF). After a median FU of 37 months (24–49 months), ASD was diagnosed in 16% of the cTDR patients and in 18% of patients with ACDF.
However, it needs to be highlighted that a routine MRI investigation of the cervical spine was not included in the present study protocol. Conversely, the presence of ASD was determined based on lateral X-ray images by two independent observers according to previously established and well-defined criteria. Similar radiological criteria were used by Lee et al. [23]. They found adjacent segment degeneration in 35.7% in the cervical disc arthroplasty group and in 57.1% in the fusion group at a mean follow-up of 43.4 resp. 44.6 months for the fusion group. Interestingly, the ASD appeared earlier in the fusion group. The risk factor analysis indicated a higher lordosis angulation from C3 to C7 for non-ASD-patients in both groups and the development of heterotopic ossifications in the arthroplasty group was associated with the presence of ASP. Contrary to this study, Di Martino et al. [24] conclude in a systematic review regarding the cervical spine alignment in disc arthroplasty that the overall cervical alignment after TDR tends towards a loss of lordosis. Some studies demonstrated that focal or global kyphosis after ACDF is associated with the appearance of adjacent segment disease [25, 26]. The topic of post-operative cervical alignment as an influencing factor for ASD has to be studied more in detail in further investigations.
As outlined in Fig. 5, lower ROM values preoperatively were already positively correlated with the occurrence of adjacent level degenerative changes at later post-operative FU stages.
One possible explanation of the present results could be that an impaired pre-operative mobility of the motion segment had already taken effect on the natural course of degeneration in the adjacent segment. In addition, the significant decrease in the ROM during the post-operative course may be interpreted as an indicator of the importance of maintained motion preservation of the index segment.
At later FU stages, an increase in high-grade ossifications of the prostheses was noted, which was associated with a significant reduction in range of motion. Despite the fact that this had no significant adverse effects on the clinical outcome parameters, as noted in other studies [27,28,29,30,31,32,33], efforts should be made to avoid the occurrence of HO.
Ament et al. conclude in a cost-effectiveness study regarding cTDR and ACDF for the treatment of two-level cervical degenerated disc disease that cTDR appears to be a highly cost-effective surgical modality compared with ACDF. Qureshi et al. analysed the cost-effectiveness comparing single level TDR and ACDF and conclude also that cTDR and ACDF are cost-effective procedures, but cTDR must remain functional for at least 14 years to establish greater cost-effectiveness than ACDF [34]. The appearance of HO right up to solid fusion (Grade 4) is a well known complication in cervical total disc replacement which can affect the motion, respectively, the function of the prosthesis [31, 32, 35] regardless the implant-type [7, 11, 17, 27, 28, 36,37,38,39]. The progression of HO into higher grades over time was also seen in other studies [28, 32]. Up to now there is no study available that could demonstrate a significant effect of the use of NSAID in the early post-operative period to avoid or reduce the incidence of HO. Nevertheless, at least a trend toward less HO formation and fewer immobile discs in patients who used NSAID’s after could be observed [29, 39, 40]. Further possible underlying causes for the high incidence of heterotopic ossifications may include the preparation of the end plates as well as the opening of the cortex resulting from the chiseling of the keels during implant insertion [39, 41]. Future studies should therefore investigate whether further developments and design changes which serve to avoid damages to the vertebral body surface may ultimately reduce the incidence of heterotopic ossifications.
Study limitations
One of the limitations of this present investigation is a potential selection bias, which may be attributed to the fact that the data are derived from a non-randomised case series.
In addition, an adequate assessment of adjacent segment degenerative changes is challenging without post-operative MRI imaging of the cervical spine. However, due to the above mentioned and previously defined radiological criteria examined in conjunction with an additional clinical deterioration, an adjacent segment disease can still be diagnosed adequately.
Conclusions
Cervical artificial disc replacement with ProDisc C demonstrated a maintained, significant and satisfactory improvement of all clinical parameters over a long-term FU. Although a substantial rate of high-grade ossifications (grade 3 and 4) have previously been published, the present data did not reveal any detrimental effect on the patient’s clinical symptomatology. With low implant-related reoperation rates and low symptomatic adjacent segment degeneration rates after a FU period of 10.2 years, artificial cervical disc replacement can be regarded as a safe and effective treatment option.
References
Delamarter RB, Zigler J (2012) Five-year reoperation rates, cervical total disc replacement versus fusion, results of a prospective randomized clinical trial. Spine (Phila Pa 1976) 38:1. doi:10.1097/BRS.0b013e3182797592
Burkus JK, Haid RW, Traynelis VC, Mummaneni PV (2010) Long-term clinical and radiographic outcomes of cervical disc replacement with the Prestige disc: results from a prospective randomized controlled clinical trial. J Neurosurg Spine 13:308–318. doi:10.3171/2010.3.SPINE09513
Loumeau TP, Darden BV, Kesman TJ et al (2016) A RCT comparing 7-year clinical outcomes of one level symptomatic cervical disc disease (SCDD) following ProDisc-C total disc arthroplasty (TDA) versus anterior cervical discectomy and fusion (ACDF). Eur spine J Off Publ Eur Spine Soc Eur Spinal Deform Soc Eur Sect Cerv Spine Res Soc. doi:10.1007/s00586-016-4431-6
Phillips FM, Geisler FH, Gilder KM et al (2015) Long-term outcomes of the US FDA IDE prospective, randomized controlled clinical trial comparing PCM cervical disc arthroplasty with anterior cervical discectomy and fusion. Spine (Phila Pa 1976) 40:674–683. doi:10.1097/BRS.0000000000000869
Davis RJ, Kim KD, Hisey MS et al (2013) Cervical total disc replacement with the Mobi-C cervical artificial disc compared with anterior discectomy and fusion for treatment of 2-level symptomatic degenerative disc disease: a prospective, randomized, controlled multicenter clinical trial. J Neurosurg Spine 19:532–545. doi:10.3171/2013.6.SPINE12527
Coric D, Kim PK, Clemente JD et al (2013) Prospective randomized study of cervical arthroplasty and anterior cervical discectomy and fusion with long-term follow-up: results in 74 patients from a single site. J Neurosurg Spine 18:36–42. doi:10.3171/2012.9.SPINE12555
Davis RJ, Nunley PD, Kim KD et al (2015) Two-level total disc replacement with Mobi-C cervical artificial disc versus anterior discectomy and fusion: a prospective, randomized, controlled multicenter clinical trial with 4-year follow-up results. J Neurosurg Spine 22:15–25. doi:10.3171/2014.7.SPINE13953.Disclosure
Skeppholm M, Lindgren L, Henriques T et al (2015) The Discover artificial disc replacement versus fusion in cervical radiculopathy—a randomized controlled outcome trial with 2-year follow-up. Spine J 15:1284–1294. doi:10.1016/j.spinee.2015.02.039
Vaccaro A, Beutler W, Peppelman W et al (2013) Clinical outcomes with selectively constrained SECURE-C cervical disc arthroplasty: two-year results from a prospective, randomized, controlled, multicenter investigational device exemption study. Spine (Phila Pa 1976) 38:2227–2239. doi:10.1097/BRS.0000000000000031
Hilibrand AS, Carlson GD, Palumbo MA et al (1999) Radiculopathy and myelopathy at segments adjacent to the site of a previous anterior cervical arthrodesis. J Bone Jt Surg Am 81:519–528
Mehren C, Suchomel P, Grochulla F et al (2006) Heterotopic ossification in total cervical artificial disc replacement. Spine (Phila Pa 1976) 31:2802–2806. doi:10.1097/01.brs.0000245852.70594.d5
Caspar W, Barbier DD, Klara PM (1989) Anterior cervical fusion and Caspar plate stabilization for cervical trauma. Neurosurgery 25:491–502
Zechmeister I, Winkler R, Mad P (2011) Artificial total disc replacement versus fusion for the cervical spine: a systematic review. Eur Spine J 20:177–184. doi:10.1007/s00586-010-1583-7
Upadhyaya CD, Wu J-C, Trost G et al (2012) Analysis of the three United States Food and Drug Administration investigational device exemption cervical arthroplasty trials. J Neurosurg Spine 16:216–228. doi:10.3171/2011.6.SPINE10623
Hisey MS, Bae HW, Davis RJ et al (2015) Prospective, randomized comparison of cervical total disk replacement versus anterior cervical fusion. J Spinal Disord Tech 28:237–243
Zhao Y, Zhang Y, Sun Y et al (2016) Application of cervical arthroplasty with Bryan cervical disc: 10-year follow-up results in China. Spine (Phila Pa 1976) 41:111–115. doi:10.1097/BRS.0000000000001145
Suchomel P, Jurák L, Beneš V et al (2010) Clinical results and development of heterotopic ossification in total cervical disc replacement during a 4-year follow-up. Eur Spine J 19:307–315. doi:10.1007/s00586-009-1259-3
Goffin J, van Loon J, Van Calenbergh F, Lipscomb B (2010) A clinical analysis of 4- and 6-year follow-up results after cervical disc replacement surgery using the Bryan cervical disc prosthesis. J Neurosurg Spine 12:261–269. doi:10.3171/2009.9.SPINE09129
Dejaegher J, Walraevens J, Van Loon J, Van Calenbergh F (2016) 10-year follow-up after implantation of the Bryan cervical disc prosthesis. Eur Spine J. doi:10.1007/s00586-016-4897-2
Delamarter RB, Zigler JE, Murrey DB et al (2012) Seven-year reoperation rates: results of a prospective randomized clinical trial: cervical total disc replacement versus fusion. Spine J 12:S96. doi:10.1016/j.spinee.2012.08.268
Nunley PD, Jawahar A, Cavanaugh DA et al (2013) Symptomatic adjacent segment disease after cervical total disc replacement: re-examining the clinical and radiological evidence with established criteria. Spine J 13:5–12. doi:10.1016/j.spinee.2012.11.032
Jawahar A, Cavanaugh DA, Kerr EJ 3rd et al (2010) Total disc arthroplasty does not affect the incidence of adjacent segment degeneration in cervical spine: results of 93 patients in three prospective randomized clinical trials. Spine J 10:1043–1048. doi:10.1016/j.spinee.2010.08.014
Lee SE, Jahng T-A, Kim HJ (2015) Correlation between cervical lordosis and adjacent segment pathology after anterior cervical spinal surgery. Eur Spine J 24:2899–2909. doi:10.1007/s00586-015-4132-6
Di Martino A, Papalia R, Albo E et al (2015) Cervical spine alignment in disc arthroplasty: should we change our perspective? Eur Spine J 24:810–825. doi:10.1007/s00586-015-4258-6
Katsuura A, Hukuda S, Saruhashi Y, Mori K (2001) Kyphotic malalignment after anterior cervical fusion is one of the factors promoting the degenerative process in adjacent intervertebral levels. Eur spine J Off Publ Eur Spine Soc Eur Spinal Deform Soc Eur Sect Cerv Spine Res Soc 10:320–324
Scheer JK, Tang JA, Smith JS et al (2013) Cervical spine alignment, sagittal deformity, and clinical implications: a review. J Neurosurg Spine 19:141–159. doi:10.3171/2013.4.SPINE12838
Zhou H, Qu Y, Dong R et al (2015) Does heterotopic ossification affect the outcomes of cervical total disc replacement? A meta-analysis. Spine (Phila Pa 1976) 40:E332–E340. doi:10.1097/BRS.0000000000000776
Yi S, Oh J, Choi G et al (2014) The fate of heterotopic ossification associated with cervical artificial disc replacement. Spine (Phila Pa 1976) 39:2078–2083. doi:10.1097/BRS.0000000000000640
Tu TH, Wu JC, Huang WC et al (2011) Heterotopic ossification after cervical total disc replacement: determination by CT and effects on clinical outcomes. J Neurosurg Spine 14:457–465. doi:10.3171/2010.11.spine10444
Wu J-C, Huang W-C, Tsai H-W et al (2012) Differences between 1- and 2-level cervical arthroplasty: more heterotopic ossification in 2-level disc replacement. J Neurosurg Spine 16:594–600. doi:10.3171/2012.2.SPINE111066
Lee JH, Jung TG, Kim HS et al (2010) Analysis of the incidence and clinical effect of the heterotopic ossification in a single-level cervical artificial disc replacement. Spine J 10:676–682. doi:10.1016/j.spinee.2010.04.017
Lee SE, Chung CK, Jahng TA (2012) Early development and progression of heterotopic ossification in cervical total disc replacement. J Neurosurg Spine 16:31–36. doi:10.3171/2011.8.SPINE11303
Kang J, Shi C, Gu Y et al (2015) Factors that may affect outcome in cervical artificial disc replacement: a systematic review. Eur Spine J 24:2023–2032. doi:10.1007/s00586-015-4096-6
Qureshi SA, McAnany S, Goz V et al (2013) Cost-effectiveness analysis: comparing single-level cervical disc replacement and single-level anterior cervical discectomy and fusion: clinical article. J Neurosurg Spine 19:546–554. doi:10.3171/2013.8.SPINE12623
Kang KC, Lee CS, Han JH, Chung SS (2010) The factors that influence the postoperative segmental range of motion after cervical artificial disc replacement. Spine J 10:689–696. doi:10.1016/j.spinee.2010.04.016
Zigler JE, Delamarter R, Murrey D et al (2012) ProDisc-C and ACDF as surgical treatment for single level cervical symptomatic degenerative disc disease. Spine (Phila Pa 1976) 38:1. doi:10.1097/BRS.0b013e318278eb38
Miao J, Yu F, Shen Y et al (2014) Clinical and radiographic outcomes of cervical disc replacement with a new prosthesis. Spine J 14:878–883. doi:10.1016/j.spinee.2013.07.439
Yi S, Kim KN, Yang MS et al (2010) Difference in occurrence of heterotopic ossification according to prosthesis type in the cervical artificial disc replacement. Spine (Phila Pa 1976) 35:1556–1561. doi:10.1097/BRS.0b013e3181c6526b
Yi S, Shin DA, Kim KN et al (2013) The predisposing factors for the heterotopic ossification after cervical artificial disc replacement. Spine J 13:1048–1054. doi:10.1016/j.spinee.2013.02.036
Tu T, Wu J, Huang W et al (2015) Postoperative nonsteroidal antiinflammatory drugs and the prevention of heterotopic ossification after cervical arthroplasty: analysis using CT and a minimum 2-year follow-up. J Neurosurg Spine 22:447–453. doi:10.3171/2014.10.SPINE14333.Disclosure
Tu TH, Wu JC, Huang WC et al (2012) The effects of carpentry on heterotopic ossification and mobility in cervical arthroplasty: determination by computed tomography with a minimum 2-year follow-up: clinical article. J Neurosurg Spine 16:601–609. doi:10.3171/2012.3.spine11436
Acknowledgements
Open access funding provided by Paracelsus Medical University. The authors wish to thank Mrs. Imme Haubitz for her statistical consultation and data analysis. We are also grateful to Mrs. Pauline Jansen Van Rensburg for her editorial assistance in the preparation of the manuscript.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors certifies that they have no commercial associations that might pose a conflict of interest in connection with this article.
Funding
The authors did not receive any outside funding or grants in support of their research or preparation of this work.
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made.
About this article
Cite this article
Mehren, C., Heider, F., Siepe, C.J. et al. Clinical and radiological outcome at 10 years of follow-up after total cervical disc replacement. Eur Spine J 26, 2441–2449 (2017). https://doi.org/10.1007/s00586-017-5204-6
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00586-017-5204-6