Abstract
Background
Cervical and back pains are important clinical problems affecting human populations globally. It is suggested that Propionibacterium acnes (P. acnes) is associated with disc herniation. The aim of this study is to evaluate the distribution of P. acnes infection in the cervical and lumbar disc material obtained from patients with disc herniation.
Methods and material
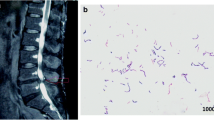
A total of 145 patients with mean age of 45.21 ± 11.24 years who underwent micro-discectomy in cervical and lumbar regions were enrolled into the study. The samples were excited during the operation and then cultured in the anaerobic incubations. The cultured P. acnes were detected by 16S rRNA-based polymerase chain reaction.
Results
In this study, 145 patients including 25 cases with cervical and 120 cases with lumbar disc herniation were enrolled to the study. There was no significant difference in the age of male and female patients (p = 0.123). P. acnes infection was detected in nine patients (36%) with cervical disc herniation and 46 patients (38.3%) with lumbar disc herniation and no significant differences were reported in P. acnes presence according to the disc regions (p = 0.508.). Moreover, there was a significant difference in the presence of P. acnes infection according to the level of lumbar disc herniation (p = 0.028).
Conclusion
According to the results, the presence of P. acnes is equal in patients with cervical and lumbar disc herniation. There was a significant difference in the distribution of P. acnes infection according to level of lumbar disc herniation.
Level of Evidence
II
Similar content being viewed by others
References
Ma S-Y, Kim H-D (2010) The effect of motorized spinal decompression delivered via SpineMED combined with physical therapy modalities for patients with cervical radiculopathy. J Phys Ther Sci 22:429–435
Güler M, Aydın T, Akgöl E, Taşpınar Ö (2015) Concomitance of fibromyalgia syndrome and cervical disc herniation. J Phys Ther Sci 27:785
Freynhagen R, Baron R, Gockel U, Tölle TR (2006) Pain DETECT: a new screening questionnaire to identify neuropathic components in patients with back pain. Curr Med Res Opin® 22:1911–1920
Sardar K, Das G, Mahta P, Mallick S, Hubbard R (2014) Medical ozone in herniated disc: a classical review. J Pain Relief 3(2167–0846):1000148
Bogduk N, Aprill C, Derby R (2013) Lumbar discogenic pain: state-of-the-art review. Pain Med 14:813–836
Schellhas KP, Smith MD, Gundry CR, Pollei SR (1996) Cervical discogenic pain: prospective correlation of magnetic resonance imaging and discography in asymptomatic subjects and pain sufferers. Spine 21:300–311
Crock H (1970) A reappraisal of intervertebral disc lesions. Med J Aust 1:983–989
Albert HB, Lambert P, Rollason J, Sorensen JS, Worthington T, Pedersen MB, Nørgaard HS, Vernallis A, Busch F, Manniche C (2013) Does nuclear tissue infected with bacteria following disc herniations lead to Modic changes in the adjacent vertebrae? Eur Spine J 22:690–696
Harris AE, Hennicke C, Byers K, Welch WC (2005) Postoperative discitis due to Propionibacterium acnes: a case report and review of the literature. Surg Neurol 63:538–541
Stirling A, Worthington T, Rafiq M, Lambert PA, Elliott TS (2001) Association between sciatica and Propionibacterium acnes. The Lancet 357:2024–2025
Arnell K, Cesarini K, Lagerqvist-Widh A, Wester T, Sjölin J (2008) Cerebrospinal fluid shunt infections in children over a 13-year period: anaerobic cultures and comparison of clinical signs of infection with Propionibacterium acnes and with other bacteria. J Neurosurg Pediatr 1(5):366–372. doi:10.3171/PED/2008/1/5/366
Ramage G, Tunney MM, Patrick S, Gorman SP, Nixon JR (2003) Formation of Propionibacterium acnes biofilms on orthopaedic biomaterials and their susceptibility to antimicrobials. Biomaterials 24:3221–3227
Douglas H, Gunter SE (1946) The taxonomic position of Corynebacterium acnes. J Bacteriol 52:15
Conen A, Walti LN, Merlo A, Fluckiger U, Battegay M, Trampuz A (2008) Characteristics and treatment outcome of cerebrospinal fluid shunt-associated infections in adults: a retrospective analysis over an 11-year period. Clin Infect Dis 47:73–82
Thompson T, Albright AL (1998) Proprionibacterium acnes infections of cerebrospinal fluid shunts. Child Nerv Syst 14:378–380
Deramo VA, Ting TD (2001) Treatment of Propionibacterium acnes endophthalmitis. Curr Opin Ophthalmol 12:225–229
Seng P, Bayle S, Alliez A, Romain F, Casanova D, Stein A (2015) The microbial epidemiology of breast implant infections in a regional referral centre for plastic and reconstructive surgery in the south of France. Int J Infect Dis 35:62–66
Del Pozo JL, Tran NV, Petty PM, Johnson CH, Walsh MF, Bite U, Clay RP, Mandrekar JN, Piper KE, Steckelberg JM (2009) Pilot study of association of bacteria on breast implants with capsular contracture. J Clin Microbiol 47:1333–1337
Delahaye F, Fol S, Celard M, Vandenesch F, Beaune J, Bozio A, de Gevigney G (2005) Propionibacterium acnes infective endocarditis. Study of 11 cases and review of literature. Arch Mal Coeur Vaiss 98:1212–1218
Schroeder JE, Girardi FP, Sandhu H, Weinstein J, Cammisa FP, Sama A (2016) The use of local vancomycin powder in degenerative spine surgery. Eur Spine J 25(4):1029–1033. doi:10.1007/s00586-015-4119-3
Lall RR, Wong AP, Lall RR, Lawton CD, Smith ZA, Dahdaleh NS (2015) Evidence-based management of deep wound infection after spinal instrumentation. J Clin Neurosci 22:238–242
Haidar R, Najjar M, Boghossian AD, Tabbarah Z (2010) Propionibacterium acnes causing delayed postoperative spine infection: review. Scand J Infect Dis 42:405–411
Trampuz A, Widmer AF (2006) Infections associated with orthopedic implants. Curr Opin Infect Dis 19:349–356
Klatte TO, Sabihi R, Guenther D, Kamath AF, Rueger JM, Gehrke T, Kendoff D (2015) High rates of occult infection after shoulder fracture fixation: considerations for conversion shoulder arthroplasty. HSS J® 11:198–203
Doita M, Kanatani T, Harada T, Mizuno K (1996) Immunohistologic study of the ruptured intervertebral disc of the lumbar spine. Spine 21:235–241
Kinane DF, Riggio MP, Walker KF, MacKenzie D, Shearer B (2005) Bacteraemia following periodontal procedures. J Clin Periodontol 32:708–713
Lafaurie GI, Mayorga-Fayad I, Torres MF, Castillo DM, Aya MR, Barón A, Hurtado PA (2007) Periodontopathic microorganisms in peripheric blood after scaling and root planing. J Clin Periodontol 34:873–879
Noble RC, Overman S (1987) Propionibacterium acnes osteomyelitis: case report and review of the literature. J Clin Microbiol 25:251–254
Osmon DR, Berbari EF, Berendt AR, Lew D, Zimmerli W, Steckelberg JM, Rao N, Hanssen A, Wilson WR (2012) Diagnosis and management of prosthetic joint infection: clinical practice guidelines by the Infectious Diseases Society of America. Clin Infect Dis 56:1–10
Caddick JM, Hilton AC, Rollason J, Lambert PA, Worthington T, Elliott TS (2005) Molecular analysis of methicillin-resistant Staphylococcus aureus reveals an absence of plasmid DNA in multidrug-resistant isolates. FEMS Immunol Med Microbiol 44:297–302
Arnell K, Cesarini K, Lagerqvist-Widh A, Wester T, Sjölin J (2008) Cerebrospinal fluid shunt infections in children over a 13-year period: anaerobic cultures and comparison of clinical signs of infection with Propionibacterium acnes and with other bacteria. J Neurosurg: Pediatr 1:266–372
Perry A, Lambert P (2011) Propionibacterium acnes: infection beyond the skin. Expert Rev Anti-Infect Ther 9:1149–1156
Uckay I, Dinh A, Vauthey L, Asseray N, Passuti N, Rottman M, Biziragusenyuka J, Riché A, Rohner P, Wendling D (2010) Spondylodiscitis due to Propionibacterium acnes: report of twenty-nine cases and a review of the literature. Clin Microbiol Infect 16:353–358
Brüggemann H, Henne A, Hoster F, Liesegang H, Wiezer A, Strittmatter A, Hujer S, Dürre P, Gottschalk G (2004) The complete genome sequence of Propionibacterium acnes, a commensal of human skin. Science 305:671–673
Brzuszkiewicz E, Weiner J, Wollherr A, Thürmer A, Hüpeden J, Lomholt HB, Kilian M, Gottschalk G, Daniel R, Mollenkopf H-J (2011) Comparative genomics and transcriptomics of Propionibacterium acnes. PLoS One 6:e21581
Brüggemann H (2005) Insights in the pathogenic potential of Propionibacterium acnes from its complete genome. Semin Cutan Med Surg 24(2):67–72. doi:10.1016/j.sder.2005.03.001
Cove J, Holland K, Cunliffe W (1983) Effects of oxygen concentration on biomass production, maximum specific growth rate and extracellular enzyme production by three species of cutaneous propionibacteria grown in continuous culture. J Gen Microbiol 129:3327–3334
Gribbon EM, Shoesmith J, Cunliffe W, Holland K (1994) The microaerophily and photosensitivity of Propionibacterium acnes. J Appl Bacteriol 77:583–590
Csukás Z, Banizs B, Rozgonyi F (2004) Studies on the cytotoxic effects of Propionibacterium acnes strains isolated from cornea. Microb Pathog 36:171–174
Adams M, McNally D, Dolan P (1996) Stress distributions inside intervertebral discs. The effects of age and degeneration. J Bone Jt Surg, Br 78:965–972
Tsuji H, Hirano N, Ohshima H, Ishihara H, Terahata N, Motoe T (1993) Structural variation of the anterior and posterior anulus fibrosus in the development of human lumbar intervertebral disc| a risk factor for intervertebral disc rupture. Spine 18:204–210
Stirling A, Rafiq M, Mathur K, Elliott T, Worthington T, Lambert P (2002) Association between sciatica and skin commensals. J Bone Jt Surg, Br 84:147
Agarwal V, Golish SR, Alamin TF (2011) Bacteriologic culture of excised intervertebral disc from immunocompetent patients undergoing single level primary lumbar microdiscectomy. J Spinal Disord Tech 24:397–400
Albert HB, Sorensen JS, Christensen BS, Manniche C (2013) Antibiotic treatment in patients with chronic low back pain and vertebral bone edema (Modic type 1 changes): a double-blind randomized clinical controlled trial of efficacy. Eur Spine J 22:697–707
Fritzell P, Bergström T, Welinder-Olsson C (2004) Detection of bacterial DNA in painful degenerated spinal discs in patients without signs of clinical infection. Eur Spine J 13:702–706
Zeller V, Ghorbani A, Strady C, Leonard P, Mamoudy P, Desplaces N (2007) Propionibacterium acnes: an agent of prosthetic joint infection and colonization. J Infect 55:119–124
de Morais Cavalcanti SM, de França ER, Lins AK, Magalhães M, de Alencar ERB, Magalhães V (2011) Investigation of Propionibacterium acnes in progressive macular hypomelanosis using real-time PCR and culture. Int J Dermatol 50:1347–1352
Nakamura M, Kametani I, Higaki S, Yamagishi T (2003) Identification of Propionibacterium acnes by polymerase chain reaction for amplification of 16S ribosomal RNA and lipase genes. Anaerobe 9:5–10
Yang S, Rothman RE (2004) PCR-based diagnostics for infectious diseases: uses, limitations, and future applications in acute-care settings. Lancet Infect Dis 4:337–348
Rollason J, McDowell A, Albert HB, Barnard E, Worthington T, Hilton AC, Vernallis A, Patrick S, Elliott T, Lambert P (2013) Genotypic and antimicrobial characterisation of Propionibacterium acnes isolates from surgically excised lumbar disc herniations. Biomed Res Int 2013:530382. doi:10.1155/2013/530382
Zhou Z, Chen Z, Zheng Y, Cao P, Liang Y, Zhang X, Wu W, Xiao J, Qiu S (2015) Relationship between annular tear and presence of Propionibacterium acnes in lumbar intervertebral disc. Eur Spine J 24:2496–2502
Carricajo A, Nuti C, Aubert E, Hatem O, Fonsale N, Mallaval F, Vautrin A, Brunon J, Aubert G (2007) Propionibacterium acnes contamination in lumbar disc surgery. J Hosp Infect 66:275–277
Ben-Galim P, Rand N, Giladi M, Schwartz D, Ashkenazi E, Millgram M, Dekel S, Floman Y (2006) Association between sciatica and microbial infection: true infection or culture contamination? Spine 31:2507–2509
Okoro T, Sell P (2010) A short report comparing outcomes between L4/L5 and L5/S1 single-level discectomy surgery. J Spinal Disord Tech 23:40–42
Aghazadeh J, Salehpour F, Ziaeii E, Javanshir N, Samadi A, Sadeghi J, Mirzaei F, Naseri Alavi SA (2016) Modic changes in the adjacent vertebrae due to disc material infection with Propionibacterium acnes in patients with lumbar disc herniation. Eur Spine J. doi:10.1007/s00586-016-4887-4
Urquhart DM, Zheng Y, Cheng AC, Rosenfeld JV, Chan P, Liew S, Hussain SM, Cicuttini FM (2015) Could low grade bacterial infection contribute to low back pain? A systematic review. BMC Med 13:13
Rajasekaran S, Tangavel C, Aiyer SN, Nayagam SM, Raveendran M, Demonte NL et al (2017) ISSLS prize in clinical science 2017: is infection the possible initiator of disc disease? An insight from proteomic analysis. Eur Spine J 26(5):1384–1400
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Funding
None.
Conflict of interest
None of the authors has any potential conflict of interest.
Rights and permissions
About this article
Cite this article
Javanshir, N., Salehpour, F., Aghazadeh, J. et al. The distribution of infection with Propionibacterium acnes is equal in patients with cervical and lumbar disc herniation. Eur Spine J 26, 3135–3140 (2017). https://doi.org/10.1007/s00586-017-5219-z
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00586-017-5219-z