Abstract
Purpose
Although many risk factors for surgical site infection (SSI) following spinal fusion have been described in the literature, methodologies and study cohorts vary widely. Patient- and procedure-specific risk factors for (SSI) can be identified via a meta-analysis. We sought to review the existing data and isolate significant risk factors for SSI in patients undergoing thoracolumbar spinal fusion.
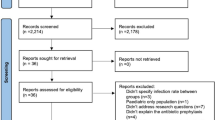
Methods
The literature was searched through December of 2016. Studies including adult patients undergoing thoracolumbar spinal fusion surgery (single or multilevel, anterior, posterior or combined approach) were identified. Only studies that included an odds ratio (OR) for SSI or sufficient data to calculate it were included. A meta-analysis was performed using RevMan 5.1. Depending on heterogeneity (I2), OR with 95% confidence intervals was calculated using either the fixed-effects model (when I2 < 60%) or the random-effects model (when I2 > 60%).
Results
6482 manuscripts were identified and reviewed. 29 manuscripts with 374,488 patients met the criteria for inclusion. Twelve risk factors were assessed by the meta-analysis and grouped into two categories (patient related and procedure related). Significant patient-related factors for SSI included obesity, diabetes, ASA score, tobacco use and revision status. Procedure-related risk factors included operative time, use of osteotomy, fusion length and extension of fusion to the sacrum or pelvis.
Conclusions
This meta-analysis identified significant risk factors for SSI following spine arthrodesis. These included potentially modifiable factors such as obesity, diabetes, smoking status and procedure-related parameters. Non-modifiable risk factors were identified, including ASA score and age. These factors may prove useful for patient counseling as well as surgical planning.
Level of evidence
Level III (Meta-analysis including studies with a level of evidence of III or higher).
Graphical abstract
These slides can be retrieved under Electronic Supplementary Material.




Similar content being viewed by others
References
Sansur CA, Smith JS, Coe JD et al (2011) Scoliosis research society morbidity and mortality of adult scoliosis surgery. Spine (Phila Pa 1976) 36:E593–E597. https://doi.org/10.1097/brs.0b013e3182059bfd
Verla T, Adogwa O, Toche U et al (2016) Impact of increasing age on outcomes of spinal fusion in adult idiopathic scoliosis. World Neurosurg 87:591–597. https://doi.org/10.1016/j.wneu.2015.10.061
Abdul-jabbar A, Takemoto S, Weber MH et al (2012) Surgical site infection in spinal. Surgery 37:1340–1345. https://doi.org/10.1097/BRS.0b013e318246a53a
Olsen MA (2008) Risk factors for surgical site infection following orthopaedic spinal operations. J Bone Joint Surg Am 90:62. https://doi.org/10.2106/jbjs.f.01515
Edwards JR, Peterson KD, Mu Y et al (2009) National healthcare safety network (NHSN) report: data summary for 2006 through 2008, issued December 2009. Am J Infect Control 37:783–805. https://doi.org/10.1016/j.ajic.2009.10.001
Hart RA, Cabalo A, Bess S et al (2013) Comparison of patient and surgeon perceptions of adverse events after adult spinal deformity surgery. Spine (Phila Pa 1976) 38:732–736. https://doi.org/10.1097/brs.0b013e31827ae242
Gum JL, Carreon LY, Stimac JD, Glassman SD (2013) Predictors of oswestry disability index worsening after lumbar fusion. Orthopedics 36:e478–e483. https://doi.org/10.3928/01477447-20130327-26
Zimlichman E, Henderson D, Tamir O et al (2013) Health care-associated infections: a meta-analysis of costs and financial impact on the US health care system. JAMA Int Med 173:2039–2046. https://doi.org/10.1001/jamainternmed.2013.9763
Akins PT, Harris J, Alvarez JL et al (2015) Risk factors associated with 30-day readmissions after instrumented spine surgery in 14,939 patients. Spine (Phila Pa 1976) 40:1022–1032. https://doi.org/10.1097/brs.0000000000000916
Leaper DJ, van Goor H, Reilly J et al (2004) Surgical site infection—a European perspective of incidence and economic burden. Int Wound J 1:247–273. https://doi.org/10.1111/j.1742-4801.2004.00067.x
Higgins J, Green S (2011) Cochrane handbook for systematic reviews of interventions version 5.1.0 [updated March 2011]. Cochrane Collab
Berríos-Torres SI, Umscheid CA, Bratzler DW et al (2017) Centers for disease control and prevention guideline for the prevention of surgical site infection. JAMA Surg 1–8:784–791. https://doi.org/10.1001/jamasurg.2017.0904
Stang A (2010) Critical evaluation of the Newcastle–Ottawa scale for the assessment of the quality of nonrandomized studies in meta-analyses. Eur J Epidemiol 25:603–605. https://doi.org/10.1007/s10654-010-9491-z
Lau J, Ioannidis JPA, Terrin N et al (2006) The case of the misleading funnel plot. BMJ 333:597–600. https://doi.org/10.1136/bmj.333.7568.597
Centre TNC (2014) Review manager (RevMan)
Higgins JPT, Thompson SG (2002) Quantifying heterogeneity in a meta-analysis. Stat Med 21:1539–1558. https://doi.org/10.1002/sim.1186
Boston KM, Baraniuk S, O’Heron S, Murray KO (2009) Risk factors for spinal surgical site infection, Houston, Texas. Infect Control Hosp Epidemiol 30:884–889. https://doi.org/10.1086/605323
Browne JA, Cook C, Pietrobon R et al (2007) Diabetes and early postoperative outcomes following lumbar fusion. Spine (Phila Pa 1976) 32:2214–2219. https://doi.org/10.1097/brs.0b013e31814b1bc0
Chaichana KL, Bydon M, Santiago-Dieppa DR et al (2014) Risk of infection following posterior instrumented lumbar fusion for degenerative spine disease in 817 consecutive cases. J Neurosurg Spine 20:45–52. https://doi.org/10.3171/2013.10.SPINE1364
Chen S, Anderson MV, Cheng WK, Wongworawat MD (2009) Diabetes associated with increased surgical site infections in spinal arthrodesis. Clin Orthop Relat Res 467:1670–1673. https://doi.org/10.1007/s11999-009-0740-y
Diebo BG, Passias PG, Marascalchi BJ et al (2015) Primary versus revision surgery in the setting of adult spinal deformity: a nationwide study on 10,912 patients. Spine (Phila Pa 1976) 40:1674–1680. https://doi.org/10.1097/brs.0000000000001114
Djurasovic M, Bratcher KR, Glassman SD et al (2008) The effect of obesity on clinical outcomes after lumbar fusion. Spine (Phila Pa 1976) 33:1789–1792. https://doi.org/10.1097/brs.0b013e31817b8f6f
Fang A, Hu SS, Endres N, Bradford DS (2005) Risk factors for infection after spinal surgery. Spine (Phila Pa 1976) 30:1460–1465. https://doi.org/10.1097/01.brs.0000166532.58227.4f
Gruskay J, Kepler C, Smith J et al (2012) Is surgical case order associated with increased infection rate after spine surgery? Spine (Phila Pa 1976) 37:1170–1174. https://doi.org/10.1097/brs.0b013e3182407859
Kalanithi PA, Arrigo R, Boakye M (2012) Morbid obesity increases cost and complication rates in spinal arthrodesis. Spine (Phila Pa 1976) 37:982–988. https://doi.org/10.1097/brs.0b013e31823bbeef
Kasliwal MK, Smith JS, Shaffrey CI et al (2012) Does prior short-segment surgery for adult scoliosis impact perioperative complication rates and clinical outcome among patients undergoing scoliosis correction? J Neurosurg Spine 17:128–133. https://doi.org/10.3171/2012.4.spine12130
Koutsoumbelis S, Hughes AP, Girardi FP et al (2011) Risk factors for postoperative infection following posterior lumbar instrumented arthrodesis. J Bone Joint Surg Am 93:1627–1633. https://doi.org/10.2106/JBJS.J.00039
Kurtz SM, Lau E, Ong KL et al (2012) Infection risk for primary and revision instrumented lumbar spine fusion in the Medicare population. J Neurosurg Spine 17:342–347. https://doi.org/10.3171/2012.7.SPINE12203
Lieber B, Han BJ, Strom RG et al (2016) Preoperative predictors of spinal infection within the national surgical quality inpatient database. World Neurosurg 89:517–524. https://doi.org/10.1016/j.wneu.2015.12.085
Maragakis LL, Cosgrove SE, Martinez EA et al (2009) Intraoperative fraction of inspired oxygen is a modifiable risk factor for surgical site infection after spinal surgery 104. Anesthesiology 110:556–562
Mehta AI, Babu R, Karikari IO et al (2012) 2012 Young investigator award winner: the distribution of body mass as a significant risk factor for lumbar spinal fusion postoperative infections. Spine (Phila Pa 1976) 37:1652–1656. https://doi.org/10.1097/brs.0b013e318241b186
Pull Ter Gunne AF, Van Laarhoven CJHM, Cohen DB (2010) Incidence of surgical site infection following adult spinal deformity surgery: An analysis of patient risk. Eur Spine J 19:982–988. https://doi.org/10.1007/s00586-009-1269-1
Schimmel JJP, Horsting PP, De Kleuver M et al (2010) Risk factors for deep surgical site infections after spinal fusion. Eur Spine J 19:1711–1719. https://doi.org/10.1007/s00586-010-1421-y
Smith JS, Sansur CA, Donaldson WF et al (2011) Short-term morbidity and mortality associated sagittal plane deformity. Spine (Phila Pa 1976) 36:958–964. https://doi.org/10.1097/brs.0b013e3181eabb26
Soroceanu A, Burton DC, Diebo BG et al (2015) Impact of obesity on complications, infection, and patient-reported outcomes in adult spinal deformity surgery. J Neurosurg Spine 23:656–664. https://doi.org/10.3171/2015.3.SPINE14743
Tominaga H, Setoguchi T, Ishidou Y et al (2016) Risk factors for surgical site infection and urinary tract infection after spine surgery. Eur Spine J 1–8:3908–3915. https://doi.org/10.1007/s00586-016-4674-2
Veeravagu A, Patil CG, Lad SP, Boakye M (2009) Risk factors for postoperative spinal wound infections after spinal decompression and fusion surgeries. Spine (Phila Pa 1976) 34:1869–1872. https://doi.org/10.1097/brs.0b013e3181adc989
Watanabe M, Sakai D, Matsuyama D et al (2010) Risk factors for surgical site infection following spine surgery: efficacy of intraoperative saline irrigation. J Neurosurg Spine 12:540–546. https://doi.org/10.3171/2009.11.SPINE09308
Yamato Y, Matsuyama Y, Hasegawa K et al (2016) A Japanese nationwide multicenter survey on perioperative complications of corrective fusion for elderly patients with adult spinal deformity. J Orthop Sci. https://doi.org/10.1016/j.jos.2016.11.006
Huang KT, Hazzard M, Thomas S et al (2015) Differences in the outcomes of anterior versus posterior interbody fusion surgery of the lumbar spine: a propensity score-controlled cohort analysis of 10,941 patients. J Clin Neurosci 22:848–853. https://doi.org/10.1016/j.jocn.2014.11.016
Núñez-Pereira S, Rodríguez-Pardo D, Pellisé F et al (2014) Postoperative urinary tract infection and surgical site infection in instrumented spinal surgery: Is there a link? Clin Microbiol Infect 20:768–773. https://doi.org/10.1111/1469-0691.12527
Tominaga H, Setoguchi T, Kawamura H et al (2016) Risk factors for unavoidable removal of instrumentation after surgical site infection of spine surgery: a retrospective case-control study. Medicine (Baltimore) 95:e5118. https://doi.org/10.1097/MD.0000000000005118
Parratte S, Pesenti S, Argenson JN (2014) Obesity in orthopedics and trauma surgery. Orthop Traumatol Surg Res 100:S91–S97. https://doi.org/10.1016/j.otsr.2013.11.003
Abdallah DY, Jadaan MM, McCabe JP (2013) Body mass index and risk of surgical site infection following spine surgery: a meta-analysis. Eur Spine J 22:2800–2809. https://doi.org/10.1007/s00586-013-2890-6
Nickel BT, Klement MR, Penrose CT et al (2016) Lingering risk: bariatric surgery before total knee arthroplasty. J Arthroplasty 31:207–211. https://doi.org/10.1016/j.arth.2016.02.075
Inacio MCS, Kritz-Silverstein D, Raman R et al (2014) The risk of surgical site infection and re-admission in obese patients undergoing total joint replacement who lose weight before surgery and keep it off post-operatively. Bone Joint J 96–B:629–635. https://doi.org/10.1302/0301-620x.96b5.33136
Smith TO, Aboelmagd T, Hing CB, MacGregor A (2016) Does bariatric surgery prior to total hip or knee arthroplasty reduce post-operative complications and improve clinical outcomes for obese patients? Systematic review and meta-analysis. Bone Joint J 98–B:1160–1166. https://doi.org/10.1302/0301-620x.98b9.38024
Satake K, Kanemura T, Matsumoto A et al (2013) Predisposing factors for surgical site infection of spinal instrumentation surgery for diabetes patients. Eur Spine J 22:1854–1858. https://doi.org/10.1007/s00586-013-2783-8
Hikata T, Iwanami A, Hosogane N et al (2014) High preoperative hemoglobin A1c is a risk factor for surgical site infection after posterior thoracic and lumbar spinal instrumentation surgery. J Orthop Sci 19:223–228. https://doi.org/10.1007/s00776-013-0518-7
Jackson KL 2nd, Devine JG (2016) The effects of smoking and smoking cessation on spine surgery: a systematic review of the literature. Glob Spine J 6:695–701. https://doi.org/10.1055/s-0036-1571285
Pull ter Gunne AF, van Laarhoven CJHM, Cohen DB (2010) Surgical site infection after osteotomy of the adult spine: does type of osteotomy matter? Spine J 10:410–416. https://doi.org/10.1016/j.spinee.2009.11.017
La Maida GA, Luceri F, Gallozzi F et al (2015) Complication rate in adult deformity surgical treatment: safety of the posterior osteotomies. Eur Spine J 24:879–886. https://doi.org/10.1007/s00586-015-4275-5
Auerbach JD, Lenke LG, Bridwell KH et al (2012) Major complications and comparison between 3-column osteotomy techniques in 105 consecutive spinal deformity procedures. Spine (Phila Pa 1976) 37:1198–1210. https://doi.org/10.1097/brs.0b013e31824fffde
Leven DM, Lee NJ, Kothari P et al (2016) Frailty index is a significant predictor of complications and mortality after surgery for adult spinal deformity. Spine Phila Pa 41:1394–1401. https://doi.org/10.1097/brs.0000000000001886
Author information
Authors and Affiliations
Consortia
Corresponding author
Ethics declarations
Conflict of interest
All authors declare that they have no conflict of interest.
Additional information
This study was done in the context of the Risk stratification project lead by the Scoliosis Research Society.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Pesenti, S., Pannu, T., Andres-Bergos, J. et al. What are the risk factors for surgical site infection after spinal fusion? A meta-analysis. Eur Spine J 27, 2469–2480 (2018). https://doi.org/10.1007/s00586-018-5733-7
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00586-018-5733-7