Abstract
Background
Surgeons often rely on their intuition, experience and published data for surgical decision making and informed consent. Literature provides average values that do not allow for individualized assessments. Accurate validated machine learning (ML) risk calculators for adult spinal deformity (ASD) patients, based on 10 year multicentric prospective data, are currently available. The objective of this study is to assess surgeon ASD risk perception and compare it to validated risk calculator estimates.
Methods
Nine ASD complete (demographics, HRQL, radiology, surgical plan) preoperative cases were distributed online to 100 surgeons from 22 countries. Surgeons were asked to determine the risk of major complications and reoperations at 72 h, 90 d and 2 years postop, using a 0–100% risk scale. The same preoperative parameters circulated to surgeons were used to obtain ML risk calculator estimates. Concordance between surgeons’ responses was analyzed using intraclass correlation coefficients (ICC) (poor < 0.5/excellent > 0.85). Distance between surgeons’ and risk calculator predictions was assessed using the mean index of agreement (MIA) (poor < 0.5/excellent > 0.85).
Results
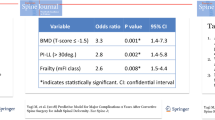
Thirty-nine surgeons (74.4% with > 10 years’ experience), from 12 countries answered the survey. Surgeons’ risk perception concordance was very low and heterogeneous. ICC ranged from 0.104 (reintervention risk at 72 h) to 0.316 (reintervention risk at 2 years). Distance between calculator and surgeon prediction was very large. MIA ranged from 0.122 to 0.416. Surgeons tended to overestimate the risk of major complications and reintervention in the first 72 h and underestimated the same risks at 2 years postop.
Conclusions
This study shows that expert surgeon ASD risk perception is heterogeneous and highly discordant. Available validated ML ASD risk calculators can enable surgeons to provide more accurate and objective prognosis to adjust patient expectations, in real time, at the point of care.



Similar content being viewed by others
References
Shaydakov ME, Tuma F (2020) Operative risk. StatPearls Publishing, Treasure Island
Kleinstueck FS, Fekete TF, Jeszenszky D et al (2016) Adult degenerative scoliosis: comparison of patient-rated outcome after three different surgical treatments. Eur Spine J Off Publ Eur Spine Soc Eur Spinal Deform Soc Eur Sect Cerv Spine Res Soc 25:2649–2656. https://doi.org/10.1007/s00586-014-3484-7
Soroceanu A, Burton DC, Oren JH et al (2016) Medical complications after adult spinal deformity surgery: incidence, risk factors, and clinical impact. Spine 41:1718–1723. https://doi.org/10.1097/BRS.0000000000001636
Scheer JK, Tang JA, Smith JS et al (2013) Reoperation rates and impact on outcome in a large, prospective, multicenter, adult spinal deformity database: clinical article. J Neurosurg Spine 19:464–470. https://doi.org/10.3171/2013.7.SPINE12901
Smith JS, Saulle D, Chen C-J et al (2012) Rates and causes of mortality associated with spine surgery based on 108,419 procedures: a review of the scoliosis research society morbidity and mortality database. Spine 37:1975–1982. https://doi.org/10.1097/BRS.0b013e318257fada
Smith JS, Sansur CA, Donaldson WF et al (2011) Short-term morbidity and mortality associated with correction of thoracolumbar fixed sagittal plane deformity: a report from the scoliosis research society morbidity and mortality committee. Spine 36:958–964. https://doi.org/10.1097/BRS.0b013e3181eabb26
Sansur CA, Smith JS, Coe JD et al (2011) Scoliosis research society morbidity and mortality of adult scoliosis surgery. Spine 36:E593-597. https://doi.org/10.1097/BRS.0b013e3182059bfd
Sciubba DM, Yurter A, Smith JS et al (2015) A comprehensive review of complication rates after surgery for adult deformity: a reference for informed consent. Spine Deform 3:575–594. https://doi.org/10.1016/j.jspd.2015.04.005
Lonergan T, Place H, Taylor P (2016) Acute complications after adult spinal deformity surgery in patients aged 70 years and older. Clin Spine Surg 29:314–317. https://doi.org/10.1097/BSD.0b013e3182764a23
Núñez-Pereira S, Pellisé F, Vila-Casademunt A et al (2019) Impact of resolved early major complications on 2 year follow-up outcome following adult spinal deformity surgery. Eur Spine J Off Publ Eur Spine Soc Eur Spinal Deform Soc Eur Sect Cerv Spine Res Soc 28:2208–2215. https://doi.org/10.1007/s00586-019-06041-x
Ames CP, Smith JS, Gum JL et al (2020) Utilization of predictive modeling to determine episode of care costs and to accurately identify catastrophic cost nonwarranty outlier patients in adult spinal deformity surgery: a step toward bundled payments and risk sharing. Spine 45:E252–E265. https://doi.org/10.1097/BRS.0000000000003242
Worley N, Marascalchi B, Jalai CM et al (2016) Predictors of inpatient morbidity and mortality in adult spinal deformity surgery. Eur Spine J Off Publ Eur Spine Soc Eur Spinal Deform Soc Eur Sect Cerv Spine Res Soc 25:819–827. https://doi.org/10.1007/s00586-015-4104-x
Charosky S, Guigui P, Blamoutier A et al (2012) Complications and risk factors of primary adult scoliosis surgery: a multicenter study of 306 patients. Spine 37:693–700. https://doi.org/10.1097/BRS.0b013e31822ff5c1
Sethi RK, Pong RP, Leveque J-C et al (2014) The Seattle spine team approach to adult deformity surgery: a systems-based approach to perioperative care and subsequent reduction in perioperative complication rates. Spine Deform 2:95–103. https://doi.org/10.1016/j.jspd.2013.12.002
Elston DM (2020) Confirmation bias in medical decision-making. J Am Acad Dermatol 82:572. https://doi.org/10.1016/j.jaad.2019.06.1286
Buchlak QD, Yanamadala V, Leveque J-C et al (2017) The seattle spine score: predicting 30-day complication risk in adult spinal deformity surgery. J Clin Neurosci Off J Neurosurg Soc Australas 43:247–255. https://doi.org/10.1016/j.jocn.2017.06.012
Croskerry P, Singhal G, Mamede S (2013) Cognitive debiasing 1: origins of bias and theory of debiasing. BMJ Qual Saf 22(Suppl 2):ii58–ii64. https://doi.org/10.1136/bmjqs-2012-001712
Pellisé F, Serra-Burriel M, Smith JS et al (2019) Development and validation of risk stratification models for adult spinal deformity surgery. J Neurosurg Spine. https://doi.org/10.3171/2019.3.SPINE181452
Ames CP, Smith JS, Pellisé F et al (2019) Artificial intelligence based hierarchical clustering of patient types and intervention categories in adult spinal deformity surgery: towards a new classification scheme that predicts quality and value. Spine 44:915–926. https://doi.org/10.1097/BRS.0000000000002974
Ames CP, Smith JS, Pellisé F et al (2019) Development of deployable predictive models for minimal clinically important difference achievement across the commonly used health-related quality of life instruments in adult spinal deformity surgery. Spine 44:1144–1153. https://doi.org/10.1097/BRS.0000000000003031
Harrell FE, Califf RM, Pryor DB et al (1982) Evaluating the yield of medical tests. JAMA 247:2543–2546
Mirza SK, Deyo RA, Heagerty PJ et al (2008) Development of an index to characterize the invasiveness of spine surgery: validation by comparison to blood loss and operative time. Spine 33:2651–2661. https://doi.org/10.1097/BRS.0b013e31818dad07
Smith JS, Shaffrey CI, Glassman SD et al (2011) Risk-benefit assessment of surgery for adult scoliosis: an analysis based on patient age. Spine 36:817–824. https://doi.org/10.1097/BRS.0b013e3181e21783
van de Graaf VA, Bloembergen CH, Willigenburg NW et al (2020) Can even experienced orthopaedic surgeons predict who will benefit from surgery when patients present with degenerative meniscal tears? a survey of 194 orthopaedic surgeons who made 3880 predictions. Br J Sports Med 54:354–359. https://doi.org/10.1136/bjsports-2019-100567
Bilimoria KY, Liu Y, Paruch JL et al (2013) Development and evaluation of the universal ACS NSQIP surgical risk calculator: a decision aid and informed consent tool for patients and surgeons. J Am Coll Surg 217(833–842):e1-3. https://doi.org/10.1016/j.jamcollsurg.2013.07.385
Sacks GD, Dawes AJ, Ettner SL et al (2016) Impact of a risk calculator on risk perception and surgical decision making: a randomized trial. Ann Surg 264:889–895. https://doi.org/10.1097/SLA.0000000000001750
Bihorac A, Ozrazgat-Baslanti T, Ebadi A et al (2019) My surgery risk: development and validation of a machine-learning risk algorithm for major complications and death after surgery. Ann Surg 269:652–662. https://doi.org/10.1097/SLA.0000000000002706
Veeravagu A, Li A, Swinney C et al (2017) Predicting complication risk in spine surgery: a prospective analysis of a novel risk assessment tool. J Neurosurg Spine 27:81–91. https://doi.org/10.3171/2016.12.SPINE16969
Lee MJ, Cizik AM, Hamilton D, Chapman JR (2014) Predicting medical complications after spine surgery: a validated model using a prospective surgical registry. Spine J Off J N Am Spine Soc 14:291–299. https://doi.org/10.1016/j.spinee.2013.10.043
Khor S, Lavallee D, Cizik AM et al (2018) Development and validation of a prediction model for pain and functional outcomes after lumbar spine surgery. JAMA Surg 153:634–642. https://doi.org/10.1001/jamasurg.2018.0072
Pellisé F, Vila-Casademunt A, Núñez-Pereira S et al (2018) The adult deformity surgery complexity index (ADSCI): a valid tool to quantify the complexity of posterior adult spinal deformity surgery and predict postoperative complications. Spine J Off J N Am Spine Soc 18:216–225. https://doi.org/10.1016/j.spinee.2017.06.042
Ames CP, Smith JS, Pellisé F et al (2019) Development of predictive models for all individual questions of SRS-22R after adult spinal deformity surgery: a step toward individualized medicine. Eur Spine J Off Publ Eur Spine Soc Eur Spinal Deform Soc Eur Sect Cerv Spine Res Soc 28:1998–2011. https://doi.org/10.1007/s00586-019-06079-x
Batty GD, Gale CR, Kivimäki M et al (2020) Comparison of risk factor associations in UK Biobank against representative, general population based studies with conventional response rates: prospective cohort study and individual participant meta-analysis. BMJ 368:m131. https://doi.org/10.1136/bmj.m131
Weaver L, Beebe TJ, Rockwood T (2019) The impact of survey mode on the response rate in a survey of the factors that influence minnesota physicians’ disclosure practices. BMC Med Res Methodol 19:73. https://doi.org/10.1186/s12874-019-0719-7
Welton KL, Kraeutler MJ, McCarty EC et al (2018) Current pain prescribing habits for common shoulder operations: a survey of the American shoulder and elbow surgeons membership. J Shoulder Elb Surg 27:S76–S81. https://doi.org/10.1016/j.jse.2017.10.005
Acknowledgements
The International Spine Study Group Foundation receives funding support from DePuy Synthes, K2M, Nuvasive, Orthofix and Zimmer Biomet. The European Spine Study Group receives funding support from DePuy Synthes and Medtronic.
Funding
The research groups receive funding support from DePuy Synthes, Medtronic K2M, Nuvasive, Orthofix and Zimmer Biomet.
Author information
Authors and Affiliations
Consortia
Corresponding author
Ethics declarations
Conflict of interest
Dr. Alanay reports grants from Medtronic, grants from Depuy Synthes, personal fees from Globus Medical, personal fees from Zimmer Biomet, outside the submitted work. Dr. Vila-Casademunt has nothing to disclose. Dr. Ames reports personal fees from UCSF, personal fees from Stryker, personal fees from Biomet Zimmer Spine, personal fees from DePuy Synthes, personal fees from Nuvasive, personal fees from Next Orthosurgical, personal fees from K2M, personal fees from Medicrea, personal fees from Titan Spine, personal fees from Medtronic, personal fees from ISSG, personal fees from Operative Neurosurgery, personal fees from SRS, personal fees from Global Spinal Analytics, outside the submitted work. Dr. Shaffrey reports grants from ISSG Foundation, during the conduct of the study; other from Nuvasive, other from Medtronic, other from SI Bone, other from Zimmer Biomet, outside the submitted work. Dr. Yilgor has nothing to disclose. Dr. Burton reports grants, personal fees and other from DePuy Synthes, other from Progenerative Medical, non-financial support from ISSG, non-financial support from SRS, other from Bioventus, other from Pzifer, outside the submitted work. Dr. Klineberg reports personal fees from Depuy Synthes, personal fees from Stryker, personal fees from Medicrea/Medtronic, grants and personal fees from AO Spine, outside the submitted work. Dr. ESSG reports grants from Depuy Synthes, grants from Medtronic, outside the submitted work. Dr. Kleinstück reports other from Depuy Synthes Spine, during the conduct of the study. Dr. Pellisé reports grants from Depuy Synthes Spine, grants and other from Medtronic, other from Nuvasive, outside the submitted work. Dr. Sánchez Pérez-Grueso has nothing to disclose. Dr. Obeid reports grants from depuy synthes, during the conduct of the study; personal fees from depuy synthes, personal fees from medtronic, personal fees from clariance, personal fees from spineart, personal fees from alphatec, outside the submitted work. Dr. ISSG reports grants from DePuy Synthes Spine, grants from K2M/Stryker, grants from NuVasive, grants from Orthofix, grants from Allosource, grants from BI Bone, during the conduct of the study; grants from Medtronic, grants from Stryker, grants from Globus, outside the submitted work. Dr. Gum reports grants from Intellirod, grants from NuVasive, grants from Integra, grants from Pfizer, grants from ISSG, grants from Norton Healthcare, during the conduct of the study; personal fees from Acuity, personal fees from Medtronic, personal fees from Depuy, personal fees from K2M/Stryker, personal fees from NuVasive, outside the submitted work; In additon, Dr. Gum has a patent Medtronic pending. Dr. Pizones reports grants from Depuy Synthes, grants and other from Medtronic, other from Stryker, during the conduct of the study. Dr. Smith reports grants from DePuy Synthes/ISSGF, during the conduct of the study; personal fees from Stryker, personal fees from Cerapedics, other from Carlsmed, personal fees from Zimmer Biomet, grants, personal fees and other from NuVasive, personal fees from Thieme, grants from NREF, grants from AOSpine, grants and personal fees from DePuy Synthes, other from Alphatec, other from Scoliosis Research Society, outside the submitted work. Dr. Gupta reports personal fees, non-financial support and other from DePuy, personal fees from Innomed, personal fees and non-financial support from Globus, personal fees and non-financial support from Medtronic, other from J&J, other from P&G, non-financial support from Scoliosis Research Society, personal fees and non-financial support from AO Spine, non-financial support from Mizuho, non-financial support from Medicrea, personal fees and non-financial support from Alphatec, outside the submitted work. Dr. Kelly has nothing to disclose. Dr. Loibl has nothing to disclose. Dr. Serra-Buriel ahs nothing to dislcose. Dr. bess reports grants from depuy synthes, grants from nuvasive, grants from k2 stryker, grants from ISSGF, during the conduct of the study; grants and other from K2 stryker, grants from medtronic, grants from globus, grants from sea spine, grants from si bone, outside the submitted work. Dr. Haddad has nothing to dislcose. Dr. Núñez-Pereira has nothing to disclose. Dr. Fekete has nothing to disclose.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Pellisé, F., Vila-Casademunt, A., Núñez-Pereira, S. et al. Surgeons’ risk perception in ASD surgery: The value of objective risk assessment on decision making and patient counselling. Eur Spine J 31, 1174–1183 (2022). https://doi.org/10.1007/s00586-022-07166-2
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00586-022-07166-2