Abstract
Introduction
The instantaneous center of rotation (iCOR) of a motion segment has been shown to correlate with its total range of motion (ROM). Importantly, a correlation of the correct placement of cervical total disc replacement (cTDR) to preserve a physiological iCOR has been previously identified. However, changes of these parameters and the corresponding clinical relevance have hardly been analyzed. This study assesses the radiological and clinical correlation of iCOR and ROM following cTDR.
Materials/methods
A retrospective multi-center observational study was conducted and radiological as well as clinical parameters were evaluated preoperatively and 1 year after cTDR with an unconstrained device. Radiographic parameters including flexion/extension X-rays (flex/ex), ROM, iCOR and the implant position in anterior–posterior direction (IP ap), as well as corresponding clinical parameters [(Neck Disability Index (NDI) and the visual analogue scale (VAS)] were assessed.
Results
57 index segments of 53 patients treated with cTDR were analyzed. Pre- and post-operative ROM showed no significant changes (8.0° vs. 10.9°; p > 0.05). Significant correlations between iCOR and IP (Pearson’s R: 0.6; p < 0.01) as well as between ROM and IP ap (Pearson’s R: − 0.3; p = 0.04) were identified. NDI and VAS improved significantly (p < 0.01). A significant correlation between NDI and IP ap after 12 months (Pearson’s R: − 0.39; p < 0.01) was found.
Conclusion
Implantation of the tested prosthesis maintains the ROM and results in a physiological iCOR. The exact position of the device correlates with the clinical outcome and emphasize the importance of implant design and precise implant positioning.
Similar content being viewed by others
Introduction
Increasing life expectancy together with active life style are promoting the trend toward motion-preserving surgical procedures, such as cervical total disc replacement (cTDR). The aim of this technique is to replace the intervertebral disc, releasing and decompressing the corresponding nerve roots while maintaining and restoring segmental and overall range of motion (ROM). Finally, this might reduce the likelihood of clinically relevant adjacent segment disease (ASD) representing one of the most common sequelae of fusion (anterior cervical discectomy and fusion; ACDF) [1]. The literature provides evidence, that ASD occurs with an annual incidence of 3% per year within the first ten years and has a cumulative incidence of 25% within 10 years [2, 3]. Various cervical disc prostheses are currently available differing in design, material and range of motion (ROM) [4,5,6,7,8]. For the current study, the ROTAIO® prosthesis (SIGNUS Medizintechnik GmbH, Alzenau, Germany) was used [9]. For most current devices, existing data focusses either on clinical outcomes or on overall kinematic analyses [9,10,11]. However, there are only few studies analyzing the correlation between clinical and kinematic results and even less focus on implant positioning and the effect of the instantaneous center of rotation (iCOR) on clinical parameters [12, 13].
The ROM is defined as the segmental movement in any direction to its full potential without causing pain. As a consequence, the ROM might be used to determine and to quantify pre- and post-operative hyper or hypomobility after cTDR [14]. Lateral flexion and extension x-ray images are routinely used to assess the ROM in the cervical as well as the lumbar spine [15, 16]. However, the ROM may vary significantly due to postoperative neck pain or reduced patient compliance [10, 11, 17,18,19,20,21]. In order to describe the quality of motion adequately, it is essential to determine the instantaneous center of rotation (iCOR), which is used to outline the movement direction in a given or treated segment during motion [14]. Previous studies indicate that the location of the iCOR after cTDR deviates significantly from its preoperative location at the instrumented level, but a detailed understanding of its clinical impact is still missing [12, 13, 22]. The same is true for the ROTAIO® prosthesis, a novel unconstrained cTDR device. There is currently no data available, on how the design mimics the physiological function of the cervical spine in relation to the ROM, whether the postoperative iCOR deviates from the preoperative iCOR and whether these parameters have an impact on clinical outcome.
This study aimed to analyse the pre- and postoperative ROM and the pre- and post-operative shift of the iCOR after cTDR with the ROTAIO® prosthesis and to evaluate a potential correlation between ROM, iCOR and the clinical outcome after 12 months.
Material and methods
Study design
This is a retrospective analysis of clinical and radiographic data from a previous prospective multicenter study (ROTAIO Multi Int PRO) evaluating clinical and radiological parameters pre- and 12 months postoperatively after cTDR with the ROTAIO® prosthesis. The ROTAIO Multi Int PRO study was approved by the local ethics committee (ID: AN 5199; session number 328/4.13) to ensure the standards of good clinical practice (GCP).
Patient population
We analyzed 53 patients treated with a uni- or bilevel cTDR from 5 different neurosurgical centers. 49 patients (92.5%) received a one level cTDR and 4 patients (7.5%) were treated by two-level cTDR. In- and exclusion criteria are summarized in Table 1.
Prosthesis design
The ROTAIO® prosthesis is an unconstrained prosthesis enabling an uncoupled translation of the vertebral bodies with a variable center of rotation (Fig. 1). This is warranted by a superior and inferior end plate with fixed sliding elements. The special design is intended to mimic physiological motion of the index segment aiming to reduce the biomechanical load on the adjacent levels. The device replaces the disc within the disc space and is sligthly inserted into the upper and lower vertebral endplates using specific insertion tools and is available in 16 different sizes [9].
Surgical technique
Positioning, approach and decompression of the index segment was performed according to a standard right-sided anterior cervcial spine approach (Smith-Robinson-Cloward approach) [23]. For implantation of the device, the provided insertion instruments and the corresponding technique recommended by the manufacturer users’ manual (SIGNUS Medizintechnik GmbH, Alzenau, Germany) were used. The correct sizing of the implanted prosthesis is determined with the use of a trial implant.
Clinical outcome parameters
The visual analogue scale (VAS) was determined to assess neck, head, arm and overall pain levels and the neck disability index (NDI) was used to identify self-rated disability preoperatively and 12 months postoperatively. These data were taken from an already implemented multi-center prospective study (ROTAIO Multi Int PRO) examining the first 12 post-operative months after cTDR.
Radiological outcome parameters
Lateral static and dynamic radiographs (X-rays) of the cervical spine were routinely obtained preoperatively and at the end of the follow-up period. The ROM (in degrees [°]) at the instrumented level was determined using lateral flexion/extension X-rays (flex/ex). To identify the average point of rotation between two vertebrae of a motion segment, we identified the iCOR at the index segment pre- and postoperatively. The iCOR is reported in percentage (%) relative to a local coordinate system of the adjacent inferior vertebral body (100% = length/height of the vertebral body) (Fig. 2). The corresponding iCOR was identified in anterior–posterior direction (iCOR ap) as well as in cranio-caudal direction (iCOR cc). The last radiological parameter to be determined was the implant position (IP), defined as the symmetry deviation between the midline of the implant and the midline of the adjacent inferior vertebral body in anterior–posterior direction. IP ap was reported in percent (%) (Fig. 3).
Statistical analysis
The imaging and statistical analysis was carried out by RAYLYTIC GmbH, Leipzig. The data analysis was generated unbiased through manual assessments by qualified, trained personnel and/or automated, validated computer routines (FXA image analysis software, FDA 510(k) number: K110765) in conformance with GLP and DIN EN ISO 13485 guidelines [24]. Values are expressed by means ± standard deviation (SD). The 2-sided-T-test was performed to analyze differences in clinical and radiological outcome parameters compared to the preoperative values. For correlation analysis between radiological and clinical parameters pre- to 12 months postoperatively, the Pearson’s (r) correlation coefficient was used. A p-value < 0.05 was considered statistically significant. All statistical evaluations were performed with SPSS Version 21.0 (IBM Corp. Released 2012. IBM SPSS Statistics for Mac OS X, Version 21.0, NY: IBM Corp.).
Results
32 females (60.4%) and 21 males (39.6%) with a mean age of 47.4 years (range: 27–65 years) received a ROTAIO® prosthesis in a total of 57 index segments. In the two-level-treated patients, each segment was analyzed for itself. The treated index segments were C4/5 (n = 2, 3.5%), C5/6 (n = 26, 54.6%) and C6/7 (n = 29, 50.9%). All patients reached a follow-up (FU) of 12 months. No implant-related complications occurred within the FU period and no revision surgeries were performed.
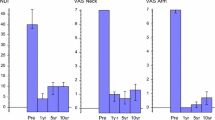
All clinical parameters improved significantly from pre- to 12 months postoperatively, except for VAS head (p < 0.01). The NDI score significantly decreased (39.3 ± 16.8 vs. 16.4 ± 16.5, p = 0.001), as well as the overall VAS (5.8 ± 2.4 vs. 2.3 ± 2.6, p = 0.001), VAS neck (5.1 ± 1.9 vs. 2.3 ± 2.3, p = 0.001) and VAS arm (5.3 ± 2.9 vs. 2.0 ± 2.4, p = 0.001). VAS head also improved, but did not reach significance (2.9 ± 2.7 vs. 2.0 ± 2.5, p = 0.07).
The mean ROM at the index segment measured 8.0° ± 3.7° preoperatively compared to 10.9° ± 4.7° 12 months postoperatively without a significant difference (p > 0.05). Analysis of iCOR ap and iCOR cc after cTDR at the index segment demonstrated no statistically significant change (iCOR ap 43.4 ± 12.4 vs. 43.4 ± 53.8; iCOR cc − 17.4 ± 13.0 vs. 10.7 ± 12.4, p > 0.05), so that the preoperative iCOR ap and iCOR cc could be preserved.
A significant positive correlation between iCOR ap and IP ap was recognized (Pearson’s R: 0.6; p < 0.01). Additionally, a significant negative correlation between ROM and IP ap (Pearson’s R: − 0.3; p = 0.04) was present (Fig. 4). The correlation analysis of radiological and clinical outcome parameters showed a significant correlation between IP ap and NDI 12 months postoperatively (Pearson’s R: − 0.39; p < 0.01) (Fig. 5). Thus, the more anteriorly the device is placed, the better the NDI outcome.
There were no further significant correlations between clinical and radiological parameters (Table 2).
Discussion
The detailed radiological analysis of a large cohort treated with a novel unconstrained cTDR device demonstrates the preservation of the iCOR and the ROM indicating physiologic motion. Implant positioning seems to play a relevant role for quality of motion and clinical outcome.
As expected after anterior decompression, clinical parameters improved significantly 12 months postoperatively. Kinematic evaluation of the pre- and postoperative ROM revealed no significant changes. The iCOR ap and iCOR cc of the index segment were also largely preserved, with a minimal non significant shift. Moreover, a significant correlation between iCOR ap and IP ap, as well as between the ROM and IP ap was revealed. There was a correlation between NDI and IP, which indicates the importance of proper implant positioning. This correlation may also be relevant for future prothesis designs.
To quantify pre- and post-operative hyper- or hypomobility, we determined the ROM [14]. Like most other investigators of various cTDR devices (6, 10, 12, 25–27), a preservation of the ROM could also be demonstrated with the used device in our analysis.
Since it is known that ROM can vary greatly due to postoperative neck pain or reduced patient compliance, it is recommended to determine the iCOR additionally, in order to describe the quality of motion appropriately [10, 11, 17,18,19,20,21]. With regard to iCOR, there are studies reporting the importance of mimicking the preoperative iCOR of a healthy functional spinal unit in order to preserve physiological ROM and the natural kinematics of the cervical spine [5, 12, 13, 17]. The advantage of maintaining a physiological iCOR and ROM may reduce excessive stress on adjacent facet joints and as a consequence prevent or minimize ASD [10, 11, 17]. Additionally, the only way to determine whether the patient's iCOR has been covered by the implantation of this special prosthesis might be demonstrated best by a central and ventral positioning of the implant in the postoperative radiographic images as part of the clinical practice.
Further investigations revealed that the postoperative iCOR correlates with cTDR design and that devices with a variable iCOR more easily restore the physiological iCOR and the natural kinematics in comparison with a prosthesis with a fixed iCOR [10,11,12, 25]. With the used unconstrained device in this study, we also observed maintenance of physiological iCOR and ROM after cTDR. Due to our results and the unconstrained design, the used prosthesis enables an uncoupled translation in the index segment and thus preserves physiological motion. Theoretically, this should translate into reduced ASD. Whereas most studies focused on ROM, we additionally analyzed implant position, as there is some variability of implant positioning in cTDR with basically all devices. The effects of IP on motion and outcome are unknown.
Some cTDR studies performed a simplified determination of the change of iCOR and a correlation analysis with clinical outcome. A slight anterior shift of the iCOR was detected, but no significant correlations between change of iCOR and clinical outcome were observed [26, 27]. The location of the iCOR, however, depends on cTDR positioning and as a consequence, the surgeon defines the iCOR. By using a semi-constrained prosthesis, there is theoretically a lower likelihood of a coincidencial match of the physiological iCOR (centrode) and the limited prosthesis COR, even if the device is appropriately implanted [10, 17, 28]. This likelihood is even decreased by the use of a constrained prosthesis. With the unconstrained device used in this study, we observed a significant positive correlation between iCOR ap and IP ap (R: 0.6), as well as a significant negative correlation between ROM and IP ap (R: − 0.3). Thus, the further anteriorly the prosthesis was implanted, the further the iCOR was shifted anteriorly, which reduced the ROM. This resulted in a significant decrease in the NDI score and thus a better clinical outcome. This is in line with the correlation analysis of all radiological and clinical parameters, which detected the most pronounced correlation between IP ap and NDI (R: − 0.39). The more anteriorly the device is implanted, the more the NDI is decreased. These findings are inconsistent compared to prior studies investigating a semiconstrained device. These studies revealed no significant correlations between the iCOR location and the clinical outcome, even if the prostheses designs are not fully comparable [5, 26, 28].
Our study demonstrates a favorable clinical outcome after cTDR with an unconstrained device, indicated by a significant decrease in NDI and VAS 12 months postoperatively. Our findings are in line with the results of a prior study using the same prosthesis with excellent clinical results 2 years after cTDR [9]. Long-term studies with other devices have reported good results [10, 29,30,31]. Long-term data for the used unconstrained device of this study is not yet available, but the preservation of physiologic motion is promire.
Relevance of findings
According to our observations it seems to be advantageous to position the used unconstrained prosthesis anteriorly leading to a slightly reduced ROM but resulting in a significant decrease in NDI and thus a better clinical outcome. These findings reveal the relevance of exact implant positioning in cTDR. Even for unconstrained devices with a variable iCOR and maintenance of physiologic motion it seems of great importance to consider the exact placement of the prosthesis to achieve better clinical outcome. This data may also be relevant for future prothesis designs.
Comparable studies for other unconstrained devices and implant positioning are lacking. However, prospective long-term clinical and kinematic outcome parameters are required to prove superiority of cTDR compared to ACDF procedures by hopefully reducing ASD.
Limitations
Obviously, the results can only be applied to the used unconstrained prosthesis, but similar effects of implant design or positioning may be found with other devices. Additionally, our results are limited by the lack of randomization, by the limited patient cohort and the retrospective study design. Generally, the kinematic analysis, performed by using 2D techniques, represents a snapshot and depends on many factors such as the individual ligament stiffness, cervical muscles and the patient’s compliance.
Conclusion
Implantation of unconstrained prostheses with the opportunity of uncoupled translation maintains the physiological ROM and iCOR. However, special attention should be paid on implant positioning. Accordingly, comparable data should be available for all cTDR designs, in order to improve the device function through optimal surgical handling and positioning.
References
Leven D, Meaike J, Radcliff K, Qureshi S (2017) Cervical disc replacement surgery: indications, technique, and technical pearls. Curr Rev Musculoskelet Med 10:160–169. https://doi.org/10.1007/s12178-017-9398-3
Hilibrand B (1999) Radiculopathy and myelopathy at segments adjacent to the site of a previous anterior cervical arthrodesis. JBJS 81:519–528
Epstein NE (2019) A review of complication rates for anterior cervical diskectomy and fusion (ACDF). Surg Neurol Int 10:100. https://doi.org/10.25259/sni-191-2019
Stulik J, Kryl J, Sebesta P et al (2008) ProDisc-C mobile replacement of an intervertebral disc. A prospective mono-centric two-year study. Acta Chir Orthop Traumatol Cech 75:253–261
Meisel H-J, Jurák L, Antinheimo J et al (2016) Four-year results of a prospective single-arm study on 200 semi-constrained total cervical disc prostheses: clinical and radiographic outcome. J Neurosurg Spine 25:556–565. https://doi.org/10.3171/2016.3.SPINE15810
Yu CC, Liu P, Huang DG et al (2016) A new cervical artificial disc prosthesis based on physiological curvature of end plate: a finite element analysis. Spine J 16:1384–1391. https://doi.org/10.1016/j.spinee.2016.06.019
Lazaro BCR, Yucesoy K, Yuksel KZ et al (2010) Effect of arthroplasty design on cervical spine kinematics: analysis of the Bryan Disc, ProDisc-C, and synergy disc. Neurosurg Focus 28:E6. https://doi.org/10.3171/2010.3.FOCUS1058
Beaurain J, Bernard P, Dufour T et al (2009) Intermediate clinical and radiological results of cervical TDR (Mobi-C®) with up to 2 years of follow-up. Eur Spine J 18:841–850. https://doi.org/10.1007/s00586-009-1017-6
Obernauer J, Landscheidt J, Hartmann S et al (2016) Cervical arthroplasty with ROTAIO® cervical disc prosthesis: first clinical and radiographic outcome analysis in a multicenter prospective trial. BMC Musculoskelet Disord 17:1–7. https://doi.org/10.1186/s12891-016-0880-7
Ryu WHA, Kowalczyk I, Duggal N (2013) Long-term kinematic analysis of cervical spine after single-level implantation of Bryan cervical disc prosthesis. Spine J 13:628–634. https://doi.org/10.1016/j.spinee.2013.02.046
Pickett GE, Rouleau JP, Duggal N (2005) Kinematic analysis of the cervical spine following implantation of an artificial cervical disc. Spine (Phila Pa 1976) 30:1949–1954
Lou J, Li H, Rong X et al (2016) Location change of center of rotation after single-level cervical total disc replacement with ProDisc-C. Acta Orthop Traumatol Turc 50:339–345. https://doi.org/10.3944/AOTT.2016.15.0182
Rong X, Gong Q, Liu H et al (2014) The effect of deviated center of rotation on flexion-extension range of motion after single-level cervical arthroplasty: an in vivo study. Spine (Phila Pa 1976) 39:B12–B18. https://doi.org/10.1097/BRS.0000000000000634
Crawford NR, Dickman CA, Sonntag VKH (2000) Neurosurgery: the scientific basis of clinical practice. In: Crockard A, Hayward R, Hoff JT (eds) 3rd edn, Blackwell Science Ltd., Oxford, 2000. pp. 1073–1092. ISBN-10: 0632048387
Dvorak J, Froehlich D, Penning L et al (1988) Functional radiographic diagnosis of the cervical spine: flexion/extension. Spine (Phila Pa 1976) 13:748–755
Frobin W, Leivseth G, Biggemann M, Brinckmann P (2002) Sagittal plane segmental motion of the cervical spine. A new precision measurement protocol and normal motion data of healthy adults. Clin Biomech 17:21–31. https://doi.org/10.1016/S0268-0033(01)00105-X
Galbusera F, Bellini CM, Brayda-Bruno M, Fornari M (2008) Biomechanical studies on cervical total disc arthroplasty: a literature review. Clin Biomech 23:1095–1104. https://doi.org/10.1016/j.clinbiomech.2008.06.002
Ahn P-G, Kim KN, Moon SW, Kim KS (2009) Changes in cervical range of motion and sagittal alignment in early and late phases after total disc replacement: radiographic follow-up exceeding 2 years. J Neurosurg Spine 11:688–695. https://doi.org/10.3171/2009.7.SPINE0946
Kim SW, Shin JH, Arbatin JJ et al (2008) Effects of a cervical disc prosthesis on maintaining sagittal alignment of the functional spinal unit and overall sagittal balance of the cervical spine. Eur Spine J 17:20–29. https://doi.org/10.1007/s00586-007-0459-y
Barrey C, Mosnier T, Jund J et al (2009) In vitro evaluation of a ball-and-socket cervical disc prosthesis with cranial geometric center. J Neurosurg Spine 11:538–546. https://doi.org/10.3171/2009.6.SPINE0949
Versus C, Geometric C (2008) In vivo kinematics of two types of ball-and-socket cervical disc replacements in the sagittal plane. Spine 33:6–9
Barrey C, Champain S, Campana S et al (2012) Sagittal alignment and kinematics at instrumented and adjacent levels after total disc replacement in the cervical spine. Eur Spine J 21:1648–1659. https://doi.org/10.1007/s00586-012-2180-8
Atlas IS, Koller H, Robinson Y (2019) Cervical spine surgery: standard and advanced techniques: cervical spine research society - Europe instructional surgical atlas; 1st edn. 2019 edition (12 July 2019), Springer, pp 317–322, ISBN-10:3319934317
Schulze M, Trautwein F, Vordemvenne T et al (2011) A method to perform spinal motion analysis from functional X-ray images. J Biomech 44:1740–1746. https://doi.org/10.1016/j.jbiomech.2011.03.040
Kowalczyk I, Lazaro BCR, Fink M et al (2011) Analysis of in vivo kinematics of 3 different cervical devices: bryan disc, ProDisc-C, and Prestige LP disc. Clin Artic J Neurosurg Spine 15:630–635. https://doi.org/10.3171/2011.8.SPINE11273
Suchomel P, Jurák L, Antinheimo J et al (2014) Does sagittal position of the CTDR-related centre of rotation influence functional outcome? Prospective 2-year follow-up analysis. Eur Spine J 23:1124–1134. https://doi.org/10.1007/s00586-014-3223-0
Karikari IO, Isaacs RE (2010) Minimally invasive transforaminal lumbar interbody fusion: a review of techniques and outcomes. Spine (Phila Pa 1976) 35:S294–S301. https://doi.org/10.1097/BRS.0b013e3182022ddc
Koller H, Meier O, Zenner J et al (2013) In vivo analysis of cervical kinematics after implantation of a minimally constrained cervical artificial disc replacement. Eur Spine J 22:747–758. https://doi.org/10.1007/s00586-012-2583-6
Walraevens JRR, Liu B, Vander SJ et al (2010) Postoperative segmental malalignment after surgery with the Bryan cervical disc prosthesis: is it related to the mechanics and design of the prosthesis? J Spinal Disord Tech 23:372–376. https://doi.org/10.1097/BSD.0b013e3181bccc69
Quan GMY, Vital JM, Hansen S, Pointillart V (2011) Eight-year clinical and radiological follow-up of the bryan cervical disc arthroplasty. Spine (Phila Pa 1976) 36:639–646. https://doi.org/10.1097/BRS.0b013e3181dc9b51
Pointillart V, Castelain JE, Coudert P et al (2018) Outcomes of the Bryan cervical disc replacement: fifteen year follow-up. Int Orthop 42:851–857. https://doi.org/10.1007/s00264-017-3745-2
Funding
Open access funding provided by University of Innsbruck and Medical University of Innsbruck.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
We have no conflicts of interest to disclose.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Lang, A., Lener, S., Grassner, L. et al. Clinical and radiological outcome 1-year after cervical total disc replacement using the Signus ROTAIO – Prosthesis. Eur Spine J 31, 3477–3483 (2022). https://doi.org/10.1007/s00586-022-07416-3
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00586-022-07416-3