Abstract
Introduction
Low back pain impacts most people throughout the course of their lives and contributes significantly to the global burden of disease. In some patients, symptoms resolve with little intervention, while others are amenable to surgical intervention, some cases are intractable to current care paradigms. Restorative neurostimulation is an emerging therapy for chronic mechanical low back pain.
Methods
We conducted a prospective post-market follow-up of 42 patients treated for longstanding chronic mechanical low back pain with restorative neurostimulation. Patients were followed up at 45, 90, and 180 days and 1 and 2 years following activation of the device. Pain, disability, and health-related quality of life were recorded.
Results
Among the 37 patients completing 2-year follow-up, numerical rating scale (NRS) pain scores improved from 7.0 ± 0.2 to 3.5 ± 0.3 (p < 0.001), Oswestry Disability Index (ODI) scores improved from 46.2 ± 2.2 to 29.2 ± 3.1 (p < 0.001), and health-related quality of life (measured by the EuroQol 5-Dimension 5-Level questionnaire—EQ-5D-5L) improved from 0.426 ± 0.035 to 0.675 ± 0.030 (p < 0.001). Additionally, 57% of patients experienced a greater than 50% reduction in pain, and 51% of patients benefited by a greater than 15-point reduction in ODI, both substantial improvements.
Conclusion
This real-world sample of patients shows that restorative neurostimulation can provide substantial and durable benefit to a cohort of patients that have traditionally had few reliable treatment options. Our findings support the continued used of this therapy in well-selected patients.
Trial Registration
ClinicalTrials.gov Identifier: NCT01985230.
Plain Language Summary
The goal of this study was to examine the effectiveness of restorative neurostimulation for the treatment of patients with chronic mechanical low back pain. This technique has been studied in a clinical trial setting and been shown to be both safe and effective. This study reports on the real-world experience from five sites in the United Kingdom. Patients with a history of severe low back pain that lasted on average for more than 13 years were implanted with a nerve stimulation device that targets the nerves that control important spinal stabilising muscles. All of the patients were asked to perform two stimulation sessions per day for 30 min each. Over the next 2 years, patients reported substantial reductions in pain and disability and an improvement in health-related quality of life. The safety profile of the therapy was excellent when compared to similar minimally invasive therapies for different spine pathologies. In this difficult-to-treat patient population who have few remaining therapeutic options, restorative neurostimulation is a valuable tool in the clinician’s armamentarium.
Similar content being viewed by others
Why carry out this study? |
This study was performed to examine the long-term results of restorative neurostimulation in a real-world population. |
What was learned from the study? |
Patients with chronic mechanical low back pain benefit significantly from the episodic contraction that results from stimulation of the medial branch of the L2 dorsal ramus. |
Improvements in pain, disability, and health-related quality of life accrue with treatment and are durable at the 2-year follow-up. |
The device has an excellent safety profile compared to similarly implanted devices. |
The real-world evidence of safety and efficacy is comparable to that observed in previous clinical trials. |
Introduction
Low back pain ranks within the top ten causes of disability-adjusted life years across all age groups worldwide [1], with an estimated global mean prevalence of 11.9% [2]. While it is commonly acknowledged that the majority of new cases of low back pain resolve within the first 2 months, that is not the case for many [3]. Some patients are eligible for surgery, others respond to conservative care and pain management approaches, but many cases do not resolve, and a significant proportion of patients with acute pain that resolves will experience a relapse within 12 months. This subset of patients can be difficult to treat and generally experience a protracted course of pain, disability, and decreased quality of life.
Intractable chronic low back pain (CLBP) has a significant impact on patient quality of life and places a heavy burden on the healthcare system and the economy owing to increased medical costs, insurance claims, disability, and loss of productivity in the workplace (absenteeism and presenteeism) [4]. According to the 2011 Health Survey for England, the annual cost of chronic back pain was estimated at £12.3 billion [5], with approximately 13% (£1.6 billion) incurred directly. The cost in the UK aligns with other international examples of the economic impact of CLBP, such as the United States, where direct costs represent 14.5% ($12 billion) of the estimated $84 billion total cost [4]. Half of patients with low back pain do not seek care, indicating that the direct healthcare expenditures are concentrated in a small subset of patients predominantly defined by their level of disability [6]. Thus, the distribution of healthcare spending on non-surgical low back pain patients is skewed to those with severe intractable symptoms, being the most resource-intensive, and a recent analysis predicted that the most expensive 25% of patients incur direct treatment costs of more than US$13,000 per annum [7]. CLBP patients are also highly likely to have a comorbid diagnosis of depression and anxiety, and have an employment status that is impacted by their pain whereby they are unable to work at maximum capacity or at all [8, 9].
Suboptimal management of low back pain due to lack of effective therapeutic interventions is a significant contributor to the global burden of the condition [10, 11]. The National Institute for Health Care Excellence (NICE) recommendations for intractable CLBP are combined physical and psychological therapies, with non-steroidal anti-inflammatory drugs for pain relief, yet the outcome for these patients is known to be poor [12, 13]. If non-invasive treatment fails, radiofrequency denervation is recommended, but only if the pain is arising from structures supplied by the medial branch nerve (confirmed by positive diagnostic block) [13]. NICE have made a research recommendation for further evidence of clinical and cost effectiveness of radiofrequency denervation. The majority of CLBP cases are “non-specific”, meaning there is no specifically identifiable cause (i.e., spinal pathology or nerve root pain). Beyond the 12-month mark, these recommended treatment options are generally unhelpful, leaving patients with limited therapeutic options beyond repeated cycles of denervation (not less than 16 months since previous one) and analgesia with opioids and other pharmacotherapeutics, all of which are temporary treatments at best.
Intractable CLBP associated with functional instability of the lumbar spine resulting from impaired motor control and atrophy of the multifidus muscle is a good example of a low back pain disease state that has had suboptimal management options [14]. Beyond 12 months of unsuccessful conventional care, this condition is considered intractable. Currently the vast majority of these patients still receive targeted physical therapy and medical management alongside other interventions that have only demonstrated efficacy early in the disease course [15]. When these approaches fail, targeted anaesthetic injections and radiofrequency ablations have been the only remaining options. However, denervation and analgesia can result in diminution of motor control over the multifidus and other structural changes [16] or delay or prevent recovery in already degenerated tissues [17]. Since dynamic stability and multifidus function cannot always be restored with physical therapy, particularly in patients with severe multifidus inhibition or atrophy and who are unable to activate or coordinate the muscle voluntarily [15], denervation and analgesia treatments can ultimately exacerbate the disease state.
Restorative neurostimulation targeting the multifidus is an emerging therapeutic option for intractable CLBP patients. ReActiv8® therapy (Mainstay Medical, Dublin, Ireland) is designed to deliver electrical stimulation to the medial branch of the dorsal ramus to elicit episodic contractions of the lumbar multifidus. With regular stimulation sessions, multifidus function and spinal stability may be restored, reducing pain and disability.
The effectiveness of restorative neurostimulation has been demonstrated in multiple clinical trials [18, 19], two of which led to market approval in Europe, Australia, and the USA. Here, we present the 2-year data from a post-market clinical study conducted in the United Kingdom.
Methods
Study Design
This post-market clinical follow-up (PMCF) study is an open label 5-year prospective follow-up of patients with intractable CLBP treated with restorative neurostimulation of the L2 medial branch of the dorsal ramus at five sites in the United Kingdom. The data presented here are the 2-year patient-reported outcomes collected across all five UK sites (ClinicalTrials.gov Identifier: NCT01985230). Any serious adverse events, whether related or not, and related adverse events were classified by the treating physician. These events were categorised as ‘device-related’, ‘procedure-related’, ‘stimulation-related’, or ‘unrelated’, and were tracked longitudinally through to resolution. Patients were implanted with a ReActiv8® device (Mainstay Medical, Dublin, Ireland) according to the manufacturer’s instructions.
The study protocol was reviewed and approved by a central ethics committee (NHS Health Research Authority North East—York Research Ethics Committee IRA’s project ID number 149412) as is required in the UK, and the protocol was followed in accordance with the Helsinki Declaration of 1964 and its later amendments. All subjects provided written informed consent to participate in the study.
Patient Selection
Consenting patients suitable for treatment with restorative neurostimulation therapy were recruited from five sites across the UK and included in the PMCF. As this cohort was intended to represent restorative neurostimulation in general clinical practice, little formal guidance was given in the way of selection criteria beyond the instructions for use and indications for the CE Mark. Effectively, patients were eligible if they were adults with a history of predominantly mechanical CLBP for longer than 90 days that was refractory to physiotherapy and medication, though in practice the patient history of CLBP was considerably longer. Physicians were trained in physical tests to establish the presence of mechanical low back pain with multifidus dysfunction such as the prone instability test [20] to include as part of the clinical work up, though the results of these individual tests were not additional inclusion or exclusion criteria. Patients were not indicated for implantation if they had a clear indication for surgery, or another clinical condition that the treating physician deemed could interfere with delivery of the therapy or assessment of pain relief. Patients were assessed at baseline by a chronic pain, musculoskeletal, or neuromodulation management multidisciplinary team (MDT). Psychological impact was assessed using both MDT assessment and the Depression, Anxiety and Stress Scale (DASS) [21], where a threshold of greater than 10–13 on the depression subscale is indicative of mild depression, and 14+ moderate to severe depression. Depression was not an exclusion criterion in this cohort. Thus the patients enrolled into this study presented with chronic mechanical low back pain with multifidus dysfunction as identified by their treating physician using physical assessment and/or magnetic resonance imaging (MRI) in order to be consistent with the instructions for use of the device.
Device Description
The neurostimulation system consists of an implantable pulse generator (IPG), two stimulating leads, and an external activator device. The proximal ends of the leads are connected to the IPG. The distal ends of the leads each contain four stimulating electrodes and two tines to secure the leads. The IPG can be programmed to deliver stimulation between any pair of electrodes on each lead.
Surgical Technique
The surgical implantation technique has been discussed elsewhere [19]; however, briefly, the leads are placed in a medial to lateral orientation through a midline incision such that the distal electrodes are positioned adjacent to the medial branch of the L2 dorsal ramus as it passes over the junction of the L3 superior articular process and the transverse process. The distal end of the lead is fixed into the intertransversarii using proprietary fixation to minimise lead migration, and the proximal end is connected to an IPG) which is positioned under the skin in the lower lumbar or upper gluteal area. Figure 1 highlights the optimal device positioning.
Device Activation and Programming
Devices were activated approximately 14 days post-implant and programmed to elicit smooth yet strong contractions of the lumbar multifidus. Programming details were reviewed at follow-up visits and optimised if deemed necessary. Patients were given a hand-held wireless activator and instructed on its use. They were instructed to deliver the therapy by initiating two daily 30-min stimulation sessions while resting in either a prone or lateral position.
Data Collection and Analysis
Patients returned for in-person follow-up visits at 45, 90, and 180 days and 1 and 2 years after the activation visit, with annual visits continuing through to 5 years post-activation. The trial schema is displayed in Fig. 2. During visits, patients completed assessments for pain (numerical rating scale—NRS), disability (Oswestry Disability Index—ODI), and health-related quality of life (measured by the EuroQol 5-Dimension 5-Level questionnaire—EQ-5D-5L).
Patient-reported outcomes were compared to baseline using repeated-measures analysis of variance (ANOVA) with Bonferroni correction for multiple comparisons conducted in R version 3.6.1 and RStudio version 1.2.5019. The impact of missing data was estimated using a simple last observation carried forward imputation.
Results
Patient Demographics
The demographic characteristics of 42 implanted patients are summarised in Table 1. The mean age was 47.2 ± 11.0 years, and 60% of patients were male. The mean duration of pain was 13.7 ± 10.2 years from first occurrence. In this patient cohort, 41% of patients were in full-time employment, 14% were employed part time, 19% were in part-time employment due to back pain, 19% were not working due to back pain, and 7% were not working for other reasons.
Patient Disposition and Follow-up
Over the enrolment period, 47 CLBP patients presenting at pain management outpatient clinics provided informed consent to participate in this study (Fig. 3). Five patients were excluded prior to implantation—one as a result of a MRI finding of a surgically treatable pathology, one due to an insufficient intensity of low back pain (NRS < 6), and three elected to not participate in the study prior to implantation. One patient presenting with CLBP with a congenital hemiplegia was implanted, but excluded from this analysis as this was considered a contra-indication per the protocol. The remaining 42 patients received the implantable restorative neurostimulation device. Between 6 and 12 months, three patients exited the study, having their devices explanted due to lack of efficacy. In year 2 of the study, one patient had the device explanted for a lack of efficacy and one patient could not be contacted for follow-up appointment.
Clinical Outcomes
Mean baseline patient-reported outcomes are listed in Table 2. At baseline, the mean ± SE pain score (NRS) was 7.0 ± 0.2, mean ± SE disability index (ODI) was 46.6 ± 2.2, and mean ± SE quality-of-life index (EQ-5D-5L) was 0.426 ± 0.035. The mean depression score was mild, with 14% of patients scoring moderate levels. Mean anxiety and stress scores at baseline were normal to mild.
Longitudinal changes in pain, disability, and quality of life are represented in Fig. 4a–c. This demonstrates a statistically significant improvement between baseline and 1 or 2 years. After 2 years of therapy, average NRS scores had reduced to 3.5 ± 0.3 (p < 0.001), ODI scores decreased to 29.2 ± 3.1 (p < 0.001), and the EQ-5D-5L index improved to 0.680 ± 0.030 (p < 0.001). The improvement in mean NRS between 1 and 2 years also met the threshold for statistical significance (p < 0.001).
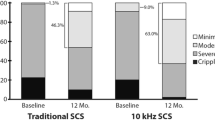
Figure 5 shows that the proportion of patients obtaining a substantial benefit in pain reduction (> 50% improvement) at 2 years was 57%, and 65% were reporting mild to negligible pain (NRS ≤ 3). Over half (51.4%) of the patients benefited from a greater then 15-point improvement in disability score with 43% of patients benefitting with a greater than 20-point reduction.
Two years after implantation, 37/42 (88%) of patients completed their follow-up appointments. The pain and disability changes over baseline are shown in a waterfall plot in Fig. 6. Of the five patients missing, four had their device explanted due to dissatisfaction with therapy, and one was not able to be contacted.
Table 3 show mean NRS scores for the completed cases, imputation by first observation carried forward (FOCF) and last observation carried forward (LOCF). Using either of these imputation methods to account for the five patients withdrawing from the study and lost to follow-up at 2 years, the mean NRS increased above the completed cases by 0.5, accounting for 7% of the change from baseline. The mean ODI at 2 years increased by 3.4 points using LOCF and 3.0 using FOCF above the 2-year completed case mean (29.2 ± 3.1), and the mean EQ-5D index decreased by 0.057 and 0.040 below the 2-year completed case mean (0.675 ± 0.030).
Safety Outcomes
The safety profile over the 2-year follow-up period showed no serious adverse events as reported by the treating physician.
A total of 20 events in 12 subjects were reported as related to the procedure, system, and/or stimulation, over the total of 930 device implant months (Table 4). All are within the expected range for this type of device and procedure.
The most common device and/or procedure-related event is tissue overstimulation, which was resolved with reprogramming in most cases. All surgical procedures were completed without incident. There were two lead fractures that required revision. A total of four patients had the system explanted due to lack of efficacy, and of those, two also noted pain at the IPG site.
Discussion
The ReActiv8-A PMCF Study is a multi-centre, prospective, single-arm study to gather data on the performance and residual risks of ReActiv8 in the real-world environment post-approval/CE Mark.
Therapy Response
Unlike analgesic approaches for neuropathic pain, where benefits can be instantaneous, restorative stimulation is believed to reduce pain and disability by the restoration of motor control of the multifidus, which occurs as a result of multiple cycles of muscle contraction. This implies that function is restored over time as spinal biomechanics normalise, reducing the aberrant movement patterns that place spinal structures under noxious loads and deformations, thereby activating tissue nociceptors and inflammatory mechanisms. The results of this study are consistent with this hypothesis and show statistically significant improvement in pain from baseline, as well as significant improvement between years 1 and 2, demonstrating an accrual of effect. Similar trends are observed for ODI and EQ-5D-5L compared to baseline, although the further accrual of effects between years 1 and 2 trended towards additional improvement.
The results of this real-world cohort study, which is intended to evaluate the therapy during routine clinical practice, are consistent with pre-market trials, where the enrolment criteria are designed to be more tightly controlled. The 2-year data from the ReActiv8-B study showed a 67% and 55% reduction in pain and disability scores, respectively [22]. The results of the current study provide further real-world evidence of the effectiveness of restorative neurostimulation therapy in a moderate-sized multi-site cohort.
Safety Performance
Reactiv8 is a minimally invasive procedure to enable stimulation of motor nerves to restore bilateral multifidus muscle function. Although not an intraspinal neuromodulation technique, comparisons with therapies such as spinal cord stimulation (SCS) or dorsal root ganglion stimulation (DRGS) give context to the Reactiv8 safety profile. For example, during a DRGS long-term follow-up study period of 24 months [23], of the 33 participants who received the full implant of DRGS, 23 participants (70%) had 33 device- or procedure-related complications. Fourteen participants (42%) underwent 17 revisions of the device, and five participants (15%) had the device explanted (dissatisfied [n = 4], change to SCS with rechargeable IPG [n = 1]) [22].
The 24-month data from the PROCESS study, comparing SCS to medical management, reported 19/42 (45%) patients having a device complication, with 31% requiring revision surgery [24].
In this PMCF cohort of patients implanted with the Reactiv8, only 12 of the 42 patients (28.6%) experienced an adverse event. Of the 20 adverse events, 10 were stimulation-related, with seven of them resolving with simple re-programming. There were two lead fractures, resulting in a revision procedure rate of 4.7%, and four of the 42 (9.5%) patients had their device explanted due to lack of efficacy. The safety outcomes reported at 1 year in the ReActiv8-B study [19] are also similar to those observed in this study.
Health Implications
Low back pain impacts most adults at some time in their lives, and although in many it may be considered a self-limiting condition, it is now understood to follow various trajectories, with many patients resulting in a state that generally does not resolve spontaneously [3, 25]. Commonly, these pain trajectories are described as persistent or stable (mild/moderate/severe), fluctuating or episodic, recovering or improving, and relapsing [25,26,27,28], but are invariably difficult to treat. Patients with long-standing low back pain, such as those in this cohort, who have a mean duration of nearly 14 years from their first episode, do not tend to spontaneously resolve. Two years after the initiation of restorative neurostimulation, 65% of patients were classified as remitters, with pain less than or equal to three points on the NRS, and 51% had a 15-point or greater reduction in their ODI.
Study Limitations
Five patients did not complete the 2-year follow-up appointment, and their missing data were imputed using simple LOCF and FOCF, including the four patients where the device was explanted for lack of efficacy. The absence of a control group may be viewed as another limitation; however, the implanted candidates had exhausted conventional medical management.
Study Strengths
This study presents real-world evidence of post-market implementation of restorative neurostimulation and, as such, is characterised by some heterogeneity in patient baseline symptoms. These data demonstrate the generalizability of the long-term data from the Gilligan et al. randomised controlled trial (RCT) [19] results to the real-world population and add further support to the adoption of this technique.
Conclusion
The 2-year follow-up of patients receiving restorative neurostimulation for intractable CLBP at multiple sites across the United Kingdom demonstrates a statistically significant, clinically meaningful and durable response across pain, disability, and quality-of-life scores. The safety of the procedure is well established as documented not only in this real-world evaluation but also in the pivotal studies that led to regulatory approval. While greater lead fracture and migration rates were initially reported with earlier device designs, these issues have been resolved with a revised procedure and lead design. As observed in the pivotal ReActiv8-B study, there were no lead migrations in this cohort and there were only two revision procedures for lead fractures. This is a remarkable safety profile when seen in the context of similar minimally invasive therapies. Given the high healthcare costs that patients such as these accrue through multiple episodes of care and interventions over the long course of their disease, durable therapies directed to resolve the cause of pain, like restorative neurostimulation, are warranted in well-selected patients.
References
Abbafati C, Abbas KM, Abbasi-Kangevari M, Abd-Allah F, Abdelalim A, Abdollahi M, et al. Global burden of 369 diseases and injuries in 204 countries and territories, 1990–2019: a systematic analysis for the Global Burden of Disease Study 2019. Lancet. 2020;396:1204–22.
Hoy D, Bain C, Williams G, March L, Brooks P, Blyth F, et al. A systematic review of the global prevalence of low back pain. Arthritis Rheum. 2012;64:2028–37.
Hestbaek L, Leboeuf-Yde C, Manniche C. Low back pain: what is the long-term course? A review of studies of general patient populations. Eur Spine J. 2003;12:149–65.
Dagenais S, Caro J, Haldeman S. A systematic review of low back pain cost of illness studies in the United States and internationally. Spine J. 2008;8:8–20.
Bridges S. Chapter 9: Chronic pain. Health survey for England—2011, health, social care and lifestyles, vol. 1. NHS Digital; 2012.
Ferreira ML, Machado G, Latimer J, Maher C, Ferreira PH, Smeets RJ. Factors defining care-seeking in low back pain—a meta-analysis of population based surveys. Eur J. 2010;14:747.e1-747.e7.
Spears CA, Hodges SE, Kiyani M, Yang Z, Edwards RM, Musick A, et al. Health care resource utilization and management of chronic, refractory low back pain in the United States. Spine. 2020;45:E1333–41.
Bener A, Verjee M, Dafeeah EE, Falah O, Al-Juhaishi T, Schlogl J, et al. Psychological factors: anxiety, depression, and somatization symptoms in low back pain patients. J Pain Res. 2013;6:95–101.
Wynne-Jones G, Cowen J, Jordan JL, Uthman O, Main CJ, Glozier N, et al. Absence from work and return to work in people with back pain: a systematic review and meta-analysis. Occup Environ Med. 2014;71:448–58.
Kim LH, Vail D, Azad TD, Bentley JP, Zhang Y, Ho AL, et al. Expenditures and health care utilization among adults with newly diagnosed low back and lower extremity pain. JAMA Netw Open. 2019;2:e193676.
Kamper SJ, Logan G, Copsey B, Thompson J, Machado GC, Abdel-Shaheed C, et al. What is usual care for low back pain? A systematic review of health care provided to patients with low back pain in family practice and emergency departments. Pain (US). 2020;161:694–702.
van Middelkoop M, Rubinstein SM, Verhagen AP, Ostelo RW, Koes BW, van Tulder MW. Exercise therapy for chronic nonspecific low-back pain. Best Pract Res Clin Rheumatol. 2010;24:193–204.
NICE. National Institute for Health and Care Excellence: Low back pain and sciatica in over 16s: assessment and management (NICE guideline 59). London: NICE; 2020.
Russo M, Deckers K, Eldabe S, Kiesel K, Gilligan C, Vieceli J, et al. Muscle control and non-specific chronic low back pain. Neuromodulation. 2018;21:1–9.
Macedo LG, Latimer J, Maher CG, Hodges PW, McAuley JH, Nicholas MK, et al. Effect of motor control exercises versus graded activity in patients with chronic nonspecific low back pain: a randomized controlled trial. Phys Ther. 2012;92:363–77.
Smuck M, Crisostomo RA, Demirjian R, Fitch DS, Kennedy DJ, Geisser ME. Morphologic changes in the lumbar spine after lumbar medial branch radiofrequency neurotomy: a quantitative radiological study. Spine J. 2015;15:1415–21.
Cohen SP, Bhaskar A, Bhatia A, Buvanendran A, Deer T, Garg S, et al. Consensus practice guidelines on interventions for lumbar facet joint pain from a multispecialty, international working group. Reg Anesth Pain Med. 2020;45:424–67.
Deckers K, De Smedt K, Mitchell B, Vivian D, Russo M, Georgius P, et al. New therapy for refractory chronic mechanical low back pain—restorative neurostimulation to activate the lumbar multifidus: one year results of a prospective multicenter clinical trial. Neuromodulation. 2018;21:48–55.
Gilligan C, Volschenk W, Russo M, Green M, Gilmore C, Mehta V, et al. An implantable restorative-neurostimulator for refractory mechanical chronic low back pain a randomized sham-controlled clinical trial. Pain. 2021. (Article in press).
Hicks GE, Fritz JM, Delitto A, Mishock J. Interrater reliability of clinical examination measures for identification of lumbar segmental instability. Arch Phys Med Rehabil. 2003;84:1858–64.
Henry JD, Crawford JR. The short-form version of the Depression Anxiety Stress Scales (DASS-21): construct validity and normative data in a large non-clinical sample. Br J Clin Psychol. 2005;44:227–39.
Gilligan CJ, Volschenk W, Russo M, Green M, Gilmore C, Mehta V, et al. Long-term outcomes of restorative neurostimulation in patients with refractory chronic low back pain secondary to multifidus dysfunction: 2-year results of the ReActiv8-B Pivotal Trial. Neuromodulation. 2021. (submitted).
Eldabe S, Copley S, Gulve A, Baranidharan G, Bretherton B, Kansal A, et al. A prospective long-term follow-up of dorsal root ganglion stimulation for the management of chronic intractable pain. Pain. 2021. (Accepted for Publication).
Kumar K, Taylor RS, Jacques L, Eldabe S, Meglio M, Molet J, et al. The effects of spinal cord stimulation in neuropathic pain are sustained: a 24-month follow-up of the prospective randomized controlled multicenter trial of the effectiveness of spinal cord stimulation. Neurosurgery. 2008;63:762–8.
Gatchel R, Bevers K, Licciardone J, Su J, Du Y, Brotto M. Transitioning from acute to chronic pain: an examination of different trajectories of low-back pain. Healthcare. 2018;6:48.
Axén I, Leboeuf-Yde C. Trajectories of low back pain. Best Pract Res Clin Rheumatol. 2013;27:601–12.
Dunn KM, Campbell P, Jordan KP. Long-term trajectories of back pain: cohort study with 7-year follow-up. BMJ Open. 2013;3:1–7.
Kongsted A, Kent P, Axen I, Downie AS, Dunn KM. What have we learned from ten years of trajectory research in low back pain? BMC Musculoskelet Disord. 2016;17:220.
Acknowledgements
The authors and sponsor would like to thank the participants in this study.
Funding
Sponsorship for this study and Rapid Service Fee was provided by Mainstay Medical.
Editorial and Other Assistance
Editorial assistance in the preparation of this article was provided by Ben Goss, PhD (Mainstay Medical) and Danielle Santarelli, PhD (Genesis Research Services). Statistical and data management support was provided by Teresa Yurik, MS (NAMSA) and trial management by Diane Burnside, BS (Mainstay Medical) and Julian Mathew, MSc. (Mainstay Medical). Support for this assistance was funded by Mainstay Medical.
Authorship
All named authors meet the International Committee of Medical Journal Editors (ICMJE) criteria for authorship for this article, take responsibility for the integrity of the work as a whole, and have given their approval for this version to be published.
Authors' Contributions
All authors contributed to the study conception, design patient implantation, data collection and follow-up. Material preparation, data aggregation and analysis were performed by Simon Thomson and Sam Eldabe. The first draft of the manuscript was written by Simon Thomson and Sam Eldabe, and all authors commented on previous versions of the manuscript. All authors read and approved the final manuscript.
List of Investigators
The authors would like to thank the other ReActiv8-PMCF investigators—Shaishav Bhagat (Ipswich Hospital NHS trust, Ipswich, UK), Nik Patel (Southmead Hospital, North Bristol NHS Trust, Bristol, UK) and Jane Hazelgrove (University Hospital Southampton, Southampton, UK)—for their involvement in the conduct of the study, including device implantation and patient follow-up.
Disclosures
Dr. Simon Thomson has received consultancy fees from Boston Scientific, and institutional research grants from Boston Scientific Neuromodulation, Mainstay Medical and Saluda Medical. Dr. Thomson’s current affiliation is Mid and South Essex University Hospitals NHS. Dr. Sarah Love-Jones has received consultancy fees from Boston Scientific, Medtronic and Nevro Corp, and institutional research grants from Boston Scientific, Medtronic, Nevro Corp, Abbot and Saluda Medical. Mr. Girish Vajramani has received consultancy fees from Abbot, Nevro Corp, Boston Scientific and Nalu Medical. Professor Sam Eldabe has received consultancy fees from Mainstay Medical, Medtronic, Boston Scientific, Abbot and institutional, grants from Nevro Corp. Mr. Adam Williams, Dr. Manohar Sharma and Dr. Rajiv Chawla declare they have no conflict of interest.
Compliance with Ethics Guidelines
The study protocol was reviewed and approved by a central ethics committee, NHS Health Research Authority North East—York Research Ethics Committee IRA’s project ID number 149412, as is required in the UK, and the protocol was followed in accordance with the Helsinki Declaration of 1964 and its later amendments. All subjects provided informed consent to participate in the study.
Data Availability
The datasets generated during and/or analysed during the current study will be available in the ClinicalTrials.gov repository after the closure of the study. In the interim they are available from the corresponding author on reasonable request.
Author information
Authors and Affiliations
Consortia
Corresponding author
Additional information
The members of the ReActiv8 PMCF Investigators are listed in the Acknowledgements section.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License, which permits any non-commercial use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc/4.0/.
About this article
Cite this article
Thomson, S., Chawla, R., Love-Jones, S. et al. Restorative Neurostimulation for Chronic Mechanical Low Back Pain: Results from a Prospective Multi-centre Longitudinal Cohort. Pain Ther 10, 1451–1465 (2021). https://doi.org/10.1007/s40122-021-00307-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40122-021-00307-3