Abstract
Study design
Validation of classification system.
Objectives
To externally validate the Proximal Humerus Ossification System (PHOS) as a reliable skeletal maturity scoring system and to assess the learning curve associated with teaching the procedure to individuals of varying levels of experience.
Background
Assessment of skeletal maturity is essential for treatment decisions in Adolescent Idiopathic Scoliosis (AIS). PHOS is a five-stage system that uses the proximal humeral physis in assessing skeletal maturity and has been shown to reliably grade skeletal age leading up to and beyond peak growth age (PGA). This system is advantageous in the AIS patient, as it is often captured in standard scoliosis films.
Methods
A medical student, an orthopedic surgery resident (PGY-2), spine fellow, and experienced scoliosis surgeon in his 25th year in practice were given a three-slide PHOS learning module. Each participant rated 100 X-rays on two separate occasions, separated by 1 week. Intra- and inter-observer reliability, as well as cross-institutional reliability, were calculated using intraclass correlation coefficients (ICC) with 95% confidence intervals [CI95].
Results
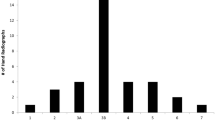
Average intra-observer reliability ICC between scoring sessions was 0.94 [0.92, 0.96] and inter-observer reliability by level of training were 0.94 [0.91, 0.96], 0.93 [0.9, 0.95], 0.94 [0.91, 0.96], 0.96 [0.94, 0.97] for the medical student, PGY-2, fellow, and attending, respectively. Reliability across institutions was 0.99 [0.98, 0.99]. Combined rating observations (n = 400) showed 82% exact matches, as well as 17% and 1% mismatches by 1 and 2 stages, respectively. Similar to the PHOS developers, we found PHOS stage 3 to occur immediately after PGA.
Conclusion
PHOS is easily learned and employed by raters with varying levels of training. It comprises a five-stage system to reliably measure bone age leading up to PGA and thereafter. This new system relies on visualization of the proximal humerus, which is readily available on standard scoliosis X-rays.
Level of evidence
Level III.

taken from the PHOS developers. d (right) was adapted from the Human Walking (p. 34) by V. T. Inman, H. J. Ralston, and F. Todd




Similar content being viewed by others
References
Negrini S et al (2012) 2011 SOSORT guidelines: orthopaedic and rehabilitation treatment of idiopathic scoliosis during growth. Scoliosis 7(1):3
Parent S, Newton PO, Wenger DR (2005) Adolescent idiopathic scoliosis: etiology, anatomy, natural history, and bracing. Instr Course Lect 54:529–536
Negrini S et al (2005) Italian guidelines on rehabilitation treatment of adolescents with scoliosis or other spinal deformities. Eura Medicophys 41(2):183–201
Grivas TB et al (2006) Association between adolescent idiopathic scoliosis prevalence and age at menarche in different geographic latitudes. Scoliosis 1:9
Wong HK et al (2005) Idiopathic scoliosis in Singapore schoolchildren: a prevalence study 15 years into the screening program. Spine (Phila Pa 1976) 30(10):1188–1196
Aebi M (2005) The adult scoliosis. Eur Spine J 14(10):925–948
Sitoula P et al (2015) Prediction of curve progression in idiopathic scoliosis. Spine 40(13):1006–1013
Sanders JO et al (2008) Predicting scoliosis progression from skeletal maturity: a simplified classification during adolescence. J Bone Jt Surg Am 90(3):540–553
Risser JC (1958) The Iliac apophysis; an invaluable sign in the management of scoliosis. Clin Orthop 11:111–119
Tanner JM, Whitehouse RH, Takaishi M (1966) Standards from birth to maturity for height, weight, height velocity, and weight velocity: British children, 1965. II. Arch Dis Child 41(220):613–635
Karol LA et al (2016) The effect of the Risser stage on bracing outcome in adolescent idiopathic scoliosis. JBJS 98(15):1253–1259
Vira S et al (2017) The interobserver and intraobserver reliability of the sanders classification versus the Risser stage. J Pediatr Orthop 37(4):e246–e249
Hackman L, Black S (2013) The reliability of the Greulich and Pyle atlas when applied to a modern Scottish population. J Forensic Sci 58(1):114–119
Li DT et al (2018) Humeral head ossification predicts peak height velocity timing and percentage of growth remaining in children. J Pediatr Orthop 38(9):e546–e550
Nelson S et al (2000) The brush inquiry: an opportunity to investigate health outcomes in a well-characterized cohort. Am J Hum Biol 12(1):1–9
Laowansiri U et al (2013) Maxillary growth and maturation during infancy and early childhood. Angle Orthod 83(4):563–571
Pyle SI, Mann AW et al (1948) A substitute for skeletal age (Todd) for clinical use; the red graph method. J Pediatr 32(2):125–136
Pyle SI, Reed RB, Stuart HC (1959) Patterns of skeletal development in the hand. Pediatrics 24:886–903
McGraw KO, Wong SP (1996) Forming inferences about some intraclass correlation coefficients. Psychol Methods 1(1):30
Koo TK, Li MY (2016) A guideline of selecting and reporting intraclass correlation coefficients for reliability research. J Chiropr Med 15(2):155–163
Daffner SD, Beimesch CF, Wang JC (2010) Geographic and demographic variability of cost and surgical treatment of idiopathic scoliosis. Spine (Phila Pa 1976) 35(11):1165–1169
Yawn BP, Yawn RA (2000) The estimated cost of school scoliosis screening. Spine (Phila Pa 1976) 25(18):2387–2391
Lonstein JE, Winter RB, Bradford DS (1995) Moe’s textbook of scoliosis and other spinal deformities. Scoliosis Research Society, Philadelphia
Yang JH et al (2014) Evaluation of accuracy of plain radiography in determining the Risser stage and identification of common sources of errors. J Orthop Surg Res 9:101
Minkara A et al (2018) High risk of mismatch between sanders and risser staging in adolescent idiopathic scoliosis: are we guiding treatment using the wrong classification? J Pediatr Orthop. https://doi.org/10.1097/BPO.0000000000001135
Norman GR et al (2008) Biostatistics: the bare essentials. PMPH USA
Li DT et al (2019) The proximal humeral ossification system improves assessment of maturity in patients with scoliosis. J Bone Jt Surg Am 101(20):1868–1874
Funding
This study was funded by the Pediatric Orthopedic Society of North America (POSNA).
Author information
Authors and Affiliations
Contributions
TDPVT, DL, CM, DC, DC, BS, and BL: conception and design, acquisition and data, analysis and interpretation of data, drafting of the manuscript, revision for important intellectual content, administrative, technical or material support, and approval final version of paper. TDPVT and DL: statistical analysis. TDPVT and BL: supervision.
Corresponding author
Ethics declarations
Conflict of interest
Dr. Li reports grants from Pediatric Orthopedic Society of North America, during the conduct of the study. Dr. Lonner reports grants from POSNA, during the conduct of the study; personal fees, non-financial support and other from Depuy Synthes, other from Ethicon, personal fees and other from Zimmer Biomet, personal fees and non-financial support from Apifix, personal fees from Unyq Align, other from Paradigm Spine, non-financial support and other from Spine Search, other from Setting Scoliosis Straight Foundation, personal fees from K2M, outside the submitted work. The remaining authors have nothing to disclose.
Ethical approval
This study was reviewed and approved by the Yale Human Research Protection Program IRB. IRB Submission ID 2000021626.
Informed consent
Obtained by the original investigators who compiled the imaging data set.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Di Pauli von Treuheim, T., Li, D.T., Mikhail, C. et al. Reliable skeletal maturity assessment for an AIS patient cohort: external validation of the proximal humerus ossification system (PHOS) and relevant learning methodology. Spine Deform 8, 613–620 (2020). https://doi.org/10.1007/s43390-020-00105-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s43390-020-00105-5