
Minimally invasive tubular laminectomies in multilevel spine surgery—an illustrative case-based review of techniques and combined approaches
Introduction
Minimally invasive procedures are nowadays commonly utilized for the treatment of many spinal pathologies. We present a review of tubular techniques, with schematic case-based illustrations, that may be utilized during the selection of tailored surgical approaches to multilevel spinal conditions.
Surgical techniques
Patients are positioned prone on a radiolucent Jackson table. Intraoperative lateral and antero-posterior (AP) fluoroscopy are utilized to guide the approach as needed. Neuro-navigation assisted techniques can also be utilized to minimize x-rays exposure (1).
Tubular retractors (METRx or Xtube, Medtronic) are utilized to expose the lamina and/or posterior joints, as described in previous publications (2,3). In cases of revision surgery, where the spinous process and lamina had been previously removed, antero-posterior (AP) X-rays can be particularly useful to direct the tubular approach and avoid drifting toward the contralateral side while exposing the superficial tissues (as the natural barrier provided by the spinous process may not be present anymore). Correct interpretation of intraoperative AP X-rays can help adjusting the angle of the tubular dissection before the neural structures are visualized. Radiation exposure for the patient and team can be minimized by stepping away from the surgical field while implementing pulse radiation, by using protective gears and by constantly apply the ALARA concepts. For a tubular laminectomy the incision is usually made 1 fingerbreadth lateral to the midline/spinous process. For a transforaminal lumbar interbody fusion (TLIF) the placement of the skin incision is guided by the AP x-rays during K-wires pedicle placement (usually 4–5 cm lateral to the midline).
To perform the tubular laminectomies the Authors prefer to utilize a Midax-rex drill with a matchstick burr and a curved long attachment that does not impede distal visualization at the tip. Loupe magnification is usually sufficient in these cases.
Most of the tubular laminectomies are performed using 22 mm diameter METRx tubes. In case previously placed instrumentations that does not require surgical revision is present at the operative level (Pedicles screws/rods, Interspinous process device) an 18 mm tube can be utilized to clear the instrumentation avoiding the need for a minimally invasive removal and replacement of the hardware.
Following is an illustrative review of the tubular techniques that can be selected and combined for the treatment of multilevel spinal stenosis, tandem stenosis, spondylolisthesis with and without bilateral pars fracture associated with stenosis or disk herniation at adjacent levels and multilevel (or holocord) spinal epidural abscess.
Information related to the illustrative cases presented in the article are summarized in Table 1.
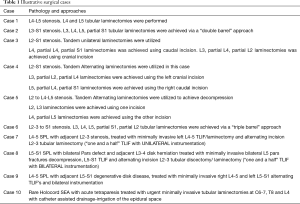
Full table
Multilevel spinal stenosis
and a half to 2 level tubular laminectomy
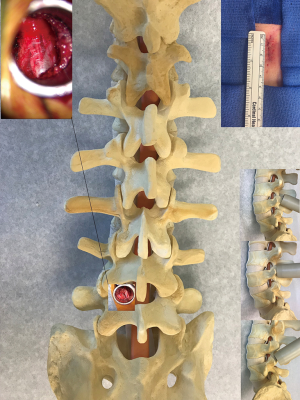
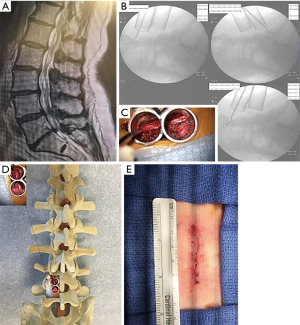
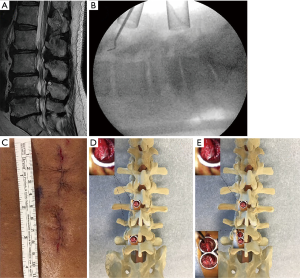
In the thoraco-lumbar spine, using a single 2.5 cm incision and a 22 mm tubular retractor, a tubular laminectomy involving up to 2 adjacent levels can be performed by tilting the tube cranially and caudally as needed. For a 2-level laminectomy involving 2 vertebral levels (e.g., L4 and L5) the tube is usually docked at the level of the intervertebral space just over the yellow ligament. Tilting the tube cranially and caudally, the laminectomies are then completed following the known surgical technique. If 3 vertebrae are involved by the stenosis (e.g., L3-4, L4-5 stenosis in need of a L4 laminectomy, partial L3, partial L5 laminectomy), the tube is docked on the central vertebral and the inferior half of the superior lamina and the superior half of the inferior lamina can be exposed by tilting the tube cranially and caudally as needed (Figure 1). Contralateral foraminotomies can be achieved by orienting the tube towards the contralateral side, while tilting the bed slightly away from the surgeon. Case 1 illustrate this technique in a L4-5 laminectomy (Figure 2).
to 3 and a half level tubular laminectomy
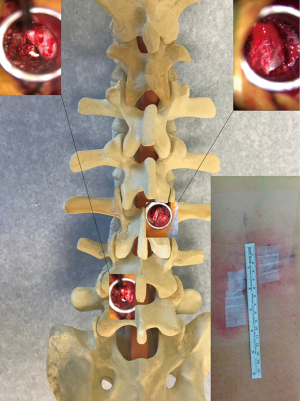
In the thoraco-lumbar spine, using a single 4 cm incision and 22 mm fixed or 24 mm expandable tubular retractors, a laminectomy involving up to 3 and a half adjacent levels can be achieved (Figure 3).
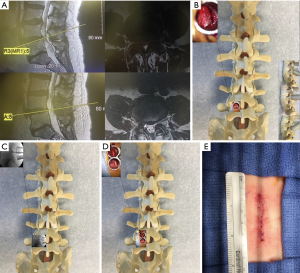
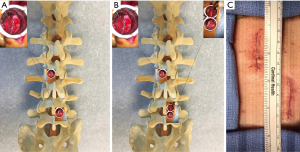
For a 2-level laminectomy a single fixed tubular retractor is utilized. When very bulky paraspinal muscles are encountered, or to achieve a 2 and a half level laminectomy, an expandable retractor (Xtube, Medtronic) is utilized. A “Double barrel” technique can be utilized to expose up to 3 and a half adjacent levels, as previously described by the Authors (4). The tubes are sequentially placed at the spinal levels of interest before starting the laminectomies so, when needed, the construct can be pivoted cranially and caudally to achieve exposure up to 3 and a half spinal levels as illustrated by the intraoperative X-rays in Case 2 (Figure 4). Placing the tubes before the starting the laminectomies also avoids the issues associated with having to re-dock the tubular system once the dura is exposed (or in case a durotomy is accidently created before the end of the procedure).
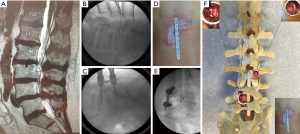
to 4 level tubular laminectomy
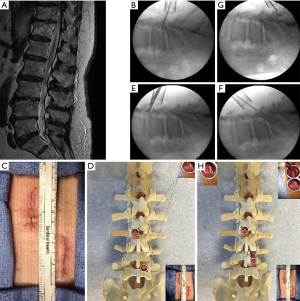
In the thoraco-lumbar spine, using a single 5.5 cm incision, a laminectomy up to 4 adjacent levels can be achieved using fixed 22 mm tubular retractors, utilizing a “Triple barrel” technique as previously described (4) (Figure 5). The tubes are sequentially placed at the spinal levels of interest before starting the laminectomies so when needed the construct can be pivoted cranially and caudally to extend the exposure to encompassing 4 spinal levels, as illustrated by the intraoperative X-rays in Case 6 (Figure 6). Having all the tubes in place before the beginning of the decompression also allows the surgeon to monitor the hemostasis at the previously operated levels as the laminectomies proceed. Once the multilevel laminectomy is completed, the tubes are sequentially removed and the muscle and fascia can be closed. A surgical drain is usually not necessary but can be placed if needed. Case 6 describes a 4-level laminectomy performed utilizing the above mentioned approach (Figure 6).
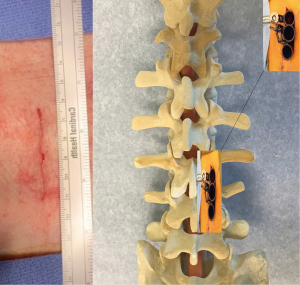
Only one set of METRx tubes can be utilized when performing a laminectomy following a “double/triple barrel” technique”, as the use of tubular dilators of slightly different length at contiguous levels does not create any problem with correct placement and visualization. We usually place an appropriate size tube at the caudal level to be decompressed, as the “next size down” dilator usually fits properly when exposing the contiguous cranial level. If tubular retractors of similar length are to be utilized, than a second set of METRx tubes can be kept available in the Operative Room.
Tandem stenosis
Tandem unilateral tubular laminectomies for multilevel tandem stenosis
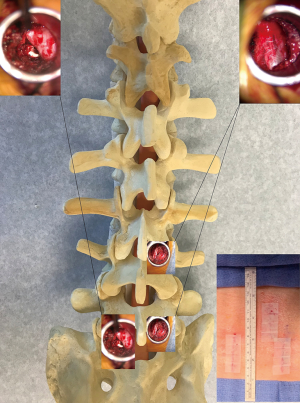
Tandem tubular laminectomies can be used in lieu of the “Triple barrel” technique to achieve multilevel posterior decompression at adjacent levels minimizing the amount of continuous muscle dissection (Figure 7). Two (or more) unilateral 1-inch incisions are utilized and tubular laminectomies are carried out at each level, following the known technique. If needed, and depending on the extent of the stenosis, a “double barrel” approach can also be combined.
Tandem unilateral laminectomies can also be utilized to treat tandem stenosis involving non adjacent spinal levels. Case 3 is an illustrative example of the use of such approach (Figure 8).
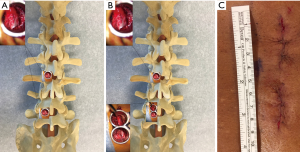
Tandem alternating tubular laminectomies for multilevel stenosis
Tandem tubular alternating laminectomies can be utilized to treat multilevel lumbar stenosis at adjacent levels or tandem stenosis at non adjacent levels (Figure 9). Bilateral 1-inch tandem incisions are placed at the levels of interest and tubular dissection and laminectomies are carried out sequentially. Although we prefer to close the fascia right after a laminectomy is completed at one level, the alternating tubes can also be left in place while treating the other levels, so that hemostasis can be monitored throughout the procedure. If needed, and depending on the extent of the stenosis, a “double barrel” approach can also be combined. Alternating tandem laminectomies were used in Case 4 (Figure 10) and Case 5 (Figure 11). To minimize the degree of unilateral postoperative muscle spasms, we prefer to utilize alternating over unilateral incisions when treating multilevel stenosis.
Lumbar spondylolisthesis
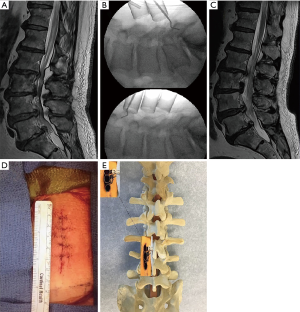
Lumbar spondylolisthesis with stenosis or disk herniation at the adjacent level (with unilateral instrumentation)
The use of minimally invasive transforaminal lumbar interbody fusion (TLIF) with adjacent segment unilateral laminectomy and decompression has been already described by Hartl and colleagues in the so called “One and a half” approach to lumbar spondylolisthesis and adjacent level stenosis (5). In low grade (grade 1-2) spondylolisthesis (SPL), the minimally invasive instrumented fusion is performed with a unilateral exposure and bilateral decompression, by tilting the tubular retractor contralaterally to achieve “over the top” and foraminal decompression as previously described (6).
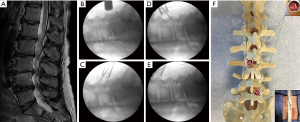
When no preoperative mechanical instability is present, or when the TLIF is performed for recurrent disk herniations, degenerative disk disease or lateral foraminal stenosis, a unilateral construct, especially in elderly patients, can be biomechanically sound possibly limiting the rate of adjacent disk disease (7-9). In this combined approach the incision used for the TLIF may be extended to allow a more medial fascial incision at the level of the adjacent laminectomy or tailored to the laterality of the compression in case of disk herniation (Figure 12). In case of adjacent level central stenosis, we prefer to make a contralateral incision to minimize the degree of unilateral muscle/fascial opening (and relative postoperative unilateral muscle spasms) as illustrated in Case 7, where SPL and lumbar stenosis at the adjacent level were present (Figure 13).
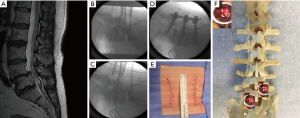
Lumbar spondylolisthesis with stenosis or disk herniation at the adjacent level (with bilateral instrumentation with or without pars defect)
In the presence of adjacent level stenosis (or disk herniation) to a spondylolisthesis and when a bilateral construct is recommended (mechanical instability, high degree listhesis, need to remove both joints to facilitate satisfactory intraoperative reduction in osteoporotic patients, or when a bilateral pars deficit decompression is planned), the TLIF can be combined with a single tubular laminectomy by extending one of the skin incisions to allow a more medial third fascial incision, or by placing a third separate small incision at the level involved by the adjacent pathology (Figure 14). Case 8 illustrates the use of such “one and a half TLIF” combined approach in a case of SPL with bilateral pars defect and adjacent level disk herniation (Figure 15).
Two level “Alternating” tubular TLIF
In cases of “staircase” SPL, multilevel degenerative disk disease or combined pathologies, a multiple level minimally invasive TLIF may be indicated.
In these cases, unless a unilateral approach is to be performed (disk herniations on the same side, purely unilateral symptoms etc.), we prefer to alternate the sides of the TLIF. In our experience this approach minimizes the amount of unilateral postoperative muscle spasms and facilitates the tubular exposure as the retractor does not tend to “slip” toward the previously operated side when performing the second TLIF. An alternating approach may also limit the extent of paraspinal muscle dissection, as the muscles superior to the posterior joint may not need to be dissected using an alternating approach (Figure 16). Case 9 is an illustrative example of the use of such alternating tubular approach for a multilevel TLIF (Figure 17).
Multilevel (or holocord) spinal epidural abscess (SEA)
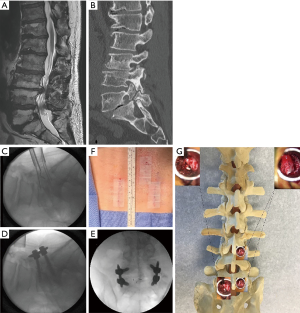
Spinal epidural abscesses involving multiple levels or encompassing more than one spinal region, may pose a surgical challenge as treatment with extensive open multilevel decompressive laminectomies in an urgent setting may not be inconsequential.
The use of tandem alternating tubular laminectomies tailored on preoperative imaging can facilitate a relatively quick and bloodless surgical drainage with decompression of the epidural space.
In such cases, we prefer to tailor the level of the laminectomies to the sagittal length of the SEA, while the laterality of the incisions for the tubular approach is guided by the radiological extension of the fluid collection on the axial plane (Figure 18). Case 10 describes the use of tandem alternating laminectomies for the urgent treatment of a rare holocord SEA (Figure 19).

The use of similar “skip” laminectomies for the treatment of multilevel spinal hematomas was also recently described (10).
Discussion
With the acquisition of long term outcome data and the evolution of instrumentation and procedures, surgeons have become more acquainted with the use of less invasive spinal techniques, which has led to a gradual expansion of their surgical indications.
The use of minimally invasive techniques in spine surgery has proven to positively affect length of stay, surgical blood loss and need for postoperative opioids, without compromising long term surgical outcome (11,12) and tubular approaches have now becoming part of the surgeons’ armamentarium for the treatment of numerous spinal conditions (13-24).
Minimally invasive muscle sparing techniques and other minimally invasive procedures have also proven to be cost effective in recently published cost-utility analysis (25,26). The amount of muscle injury from tubular approaches also positively compares with open techniques when MRI postoperative studies are analyzed (27). Despite some of the advantages introduced by the use of lesser invasive procedures, there are drawbacks that should be considered when selecting such approaches. The learning curve associated with becoming proficient with these procedures can in fact be steep and lengthy (28). Also the need for dedicated instrumentation, the lack of familiarity with the surgical anatomy that a tailored but limited tubular dissection can expose and the anatomical distortion created by the pathology at hand, may all add challenges that even experienced spine surgeons should keep into consideration before planning an operation.
Iatrogenic durotomy and subsequent CSF leak is unfortunately not uncommon during minimally invasive spine surgery. In light of the limited exposure provided by the tubular approach, a CSF leak occurring at the beginning of the procedure can adds additional challenges to the procedure and lengthen the duration of the surgery. In the presence of an active leak, the dural sac may deflate and venous bleeding from the epidural plexus may start clouding the surgical field. The presence of blood next to a durotomy may also increase the risk of adhesive arachnoiditis in the postoperative period. In some instances, nerve rootlets may also protrude from the arachnoidal opening and be exposed to involuntary iatrogenic injury during the procedure. Direct coagulation of the epidural plexus is usually poorly effective and may result in worsening of the venous oozing due to dural shrinkage, while the use of powdered hemostatic agents directly over a durotomy should be avoided. In these cases we have found useful to temporarily repair the leak with some subcutaneous fat graft and fibrin glue, so that the leak can be controlled, the dural sac can gradually re-expand and good hemostasis can be facilitated. Final repair can be then performed at the end of the procedure.
In our experience with the use of tubular laminectomies, direct suturing of iatrogenic durotomies has not been necessary, as CSF leaks are successfully repaired with the use of autologous fat graft and fibrin glue.
Among the benefits offered by minimally invasive tubular approaches in fact, is that iatrogenic CSF leaks are usually contained by the spontaneous closure of the paraspinal muscles (which are not removed/detached during the approach), when tubular retractors are removed.
Depending on the degree of central stenosis an “over the top” tubular laminectomy may be needed, so to reach and decompress the contralateral neural elements (6). Tilting the tubular retractor toward the contralateral joint will allows visualization of the contralateral foramens and bilateral decompression can be achieved via a unilateral approach. If such contralateral decompression is planned, we suggest to perform it near the end of the procedure so if a durotomy occurs, the repair is easier and no significant time is added to the duration of surgery.
In cases where a bilateral joint removal is planned/needed (e.g., pars defect with SPL, in need of reduction), a bitubular approach is utilized. Otherwise, an effective bilateral decompression can be achieved with an “over the top” laminectomy by tilting the tube toward the contralateral side while using a 45-degree Kerrison to perform a contralateral foraminotomy.
Depending on the nature and extent of the pathology at hand, as well as patients’ comorbidities, the use of open multilevel laminectomies may not always be inconsequential, with the morbidity associated to a lengthy and extensive open surgery, especially if in an urgent setting (SEA, cauda equina syndrome etc.), that are well known to the surgeons (29). Significant blood loss, extensive paraspinal muscles trauma, long incisions in bedridden patients and risks of postoperative progressive spinal deformity, should all be factored in when planning and selecting the best surgical operation to treat multilevel spinal conditions. Furthermore, treatment of non-adjacent pathologies such as tandem stenosis involving distinct spine regions (30), can sometimes be facilitated by the use of less invasive procedures.
With the introduction of tubular dissection techniques, many surgical variations have been reported and terms such as “skip”, “apical”, “alternating sides”, “double-triple barrel” laminectomies have been introduced (4,31-33). The use of “skip” laminectomies with alternating side incisions for unilateral approaches and bilateral decompression, was introduced with the goals of minimizing soft tissue trauma, muscles imbalance as well as iatrogenic postoperative instability (33). Aside from facilitating daily postoperative wound care, the use of level-skipping muscle sparing procedures can minimize intraoperative blood loss also reducing postoperative pain and overall time in the operative room (34).
Tandem or alternating laminectomies can be utilized for the treatment of multiple degenerative conditions such as tandem stenosis, multilevel disk herniation and multilevel spinal stenosis. Combination of tubular procedures is safe and feasible and such approaches can be tailored to patients’ need on a case by case bases.
Conclusions
Minimally invasive techniques are part of the spine surgeons’ armamentarium and treatment of severe degenerative conditions such as multilevel spinal stenosis, tandem stenosis, combination of spondylolisthesis and stenosis/disk herniation at adjacent spinal levels, as well as multilevel spinal epidural abscesses, may require a tailored multilevel surgical approach. Minimally invasive tubular laminectomies can be safely utilized and combined to provide safe and effective treatment of many multilevel spinal conditions. We presented a schematic, case-based, illustrative review of tubular minimally invasive techniques, based on our personal experience with these approaches that may be used to facilitate the preoperative selection of such procedures or their use in combination.
Acknowledgments
Funding: None.
Footnote
Peer Review File: Available at http://dx.doi.org/10.21037/jss-20-635
Conflicts of Interest: Both authors have completed the ICMJE uniform disclosure form (available at http://dx.doi.org/10.21037/jss-20-635). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Smith BW, Joseph JR, Kirsch M, et al. Minimally invasive guidewireless, navigated pedicle screw placement: a technical report and case series. Neurosurg Focus 2017;43:E9. [Crossref] [PubMed]
- Garg B, Mehta N. Minimally invasive transforaminal lumbar interbody fusion (MI-TLIF): A review of indications, technique, results and complications. J Clin Orthop Trauma 2019;10:S156-S162. [Crossref] [PubMed]
- Chang PY, Wang MY. Minimally invasive transforaminal lumbosacral interbody fusion. Neurosurg Focus 2016;41 Video Suppl 1:1.
- Roberti F, Arsenault KL. The Use of a "Double-Triple Barrel" Technique during Minimally Invasive Multilevel Tubular Laminectomy. A Technical Note. J Neurol Surg A Cent Eur Neurosurg 2017;78:202-5. [PubMed]
- Wipplinger C, Melcher C, Hernandez RN, et al. "One and a half" minimally invasive transforaminal lumbar interbody fusion: single level transforaminal lumbar interbody fusion with adjacent segment unilateral laminotomy for bilateral decompression for spondylolisthesis with bisegmental stenosis. J Spine Surg 2018;4:780-6. [Crossref] [PubMed]
- Kirnaz S, Wipplinger C, Schmidt FA, et al. Minimally Invasive Laminotomy for Contralateral "Over-the-Top" Foraminal Decompression Using 3-Dimensional Total Navigation: 2-Dimensional Operative Video. Oper Neurosurg (Hagerstown) 2020;19:E296. [Crossref] [PubMed]
- Ould-Slimane M, Cantogrel P, Lefèvre E, et al. Minimally invasive unilateral lumbar interbody fusion (UNILIF) in over-80-year-olds. Continuous series of 42 patients at 1.4 years' follow-up Orthop Traumatol Surg Res 2020;106:275-9. [Crossref] [PubMed]
- Nie T, Chen DJ, Tang B, et al. In vivo dynamic motion characteristics of the lower lumbar spine: L4-5 lumbar degenerative disc diseases undergoing unilateral or bilateral pedicle screw fixation combined with TLIF. J Orthop Surg Res 2019;14:171. [Crossref] [PubMed]
- Lee HJ, Kim JS, Ryu KS. Minimally Invasive TLIF Using Unilateral Approach and Single Cage at Single Level in Patients over 65. Biomed Res Int 2016;2016:4679865. [Crossref] [PubMed]
- Di Rienzo A, Brunozzi D, Dobran M, et al. Skip Hemilaminectomy for Large, Multilevel Spinal Epidural Hematomas: Report of a Series of 11 Patients. World Neurosurg 2018;111:e933-e940. [Crossref] [PubMed]
- Hammad A, Wirries A, Ardeshiri A, et al. Open versus minimally invasive TLIF: literature review and meta-analysis. J Orthop Surg Res 2019;14:229. [Crossref] [PubMed]
- Xie Q, Zhang J, Lu F, et al. Minimally invasive versus open Transforaminal lumbar Interbody fusion in obese patients: a meta-analysis. BMC Musculoskelet Disord 2018;19:15. [Crossref] [PubMed]
- Noggle JC, Sciubba DM, Samdani AF, et al. Minimally invasive direct repair of lumbar spondylolysis with a pedicle screw and hook construct. Neurosurg Focus 2008;25:E15. [Crossref] [PubMed]
- Mummaneni PV, Bisson EF, Kerezoudis P, et al. Minimally invasive versus open fusion for Grade I degenerative lumbar spondylolisthesis: analysis of the Quality Outcomes Database. Neurosurg Focus 2017;43:E11. [Crossref] [PubMed]
- Ryu DS, Ahn SS, Kim KH, et al. Does minimally invasive fusion technique influence surgical outcomes in isthmic spondylolisthesis? Minim Invasive Ther Allied Technol 2019;28:33-40. [Crossref] [PubMed]
- Kim JY, Park JY, Kim KH, et al. Minimally Invasive Transforaminal Lumbar Interbody Fusion for Spondylolisthesis: Comparison Between Isthmic and Degenerative Spondylolisthesis. World Neurosurg 2015;84:1284-93. [Crossref] [PubMed]
- Fan G, Gu G, Zhu Y, et al. Minimally Invasive Transforaminal Lumbar Interbody Fusion for Isthmic Spondylolisthesis: In Situ Versus Reduction. World Neurosurg 2016;90:580-587.e1. [Crossref] [PubMed]
- Peng P, Chen K, Chen H, et al. Comparison of O-arm navigation and microscope-assisted minimally invasive transforaminal lumbar interbody fusion and conventional transforaminal lumbar interbody fusion for the treatment of lumbar isthmic spondylolisthesis. J Orthop Translat 2019;20:107-12. [Crossref] [PubMed]
- Elmekaty M, Kotani Y, Mehy EE, et al. Clinical and Radiological Comparison between Three Different Minimally Invasive Surgical Fusion Techniques for Single-Level Lumbar Isthmic and Degenerative Spondylolisthesis: Minimally Invasive Surgical Posterolateral Fusion versus Minimally Invasive Surgical Transforaminal Lumbar Interbody Fusion versus Midline Lumbar Fusion. Asian Spine J 2018;12:870-9. [Crossref] [PubMed]
- Hubbe U, Franco-Jimenez P, Klinger JH, et al. Minimally invasive tubular microdiscectomy for recurrent lumbar disc herniation. J Neurosurg Spine 2016;24:48-53. [Crossref] [PubMed]
- Branch BC, Hilton DL, Watts C. Minimally invasive tubular access for posterior cervical foraminotomy. Surg Neurol Int 2015;6:81. [Crossref] [PubMed]
- Birch BD, Aoun RJN, Elbert GA, et al. Minimally Invasive Tubular Resection of Lumbar Synovial Cysts: Report of 40 Consecutive Cases. World Neurosurg 2016;94:188-96. [Crossref] [PubMed]
- Alvi MA, Kerezoudis P, Wahood W, et al. Operative Approaches for Lumbar Disc Herniation: A Systematic Review and Multiple Treatment Meta-Analysis of Conventional and Minimally Invasive Surgeries. World Neurosurg. 2018;114:391-407.e2. [Crossref] [PubMed]
- Akinduro OO, Kerezoudis P, Alvi MA, et al. Open Versus Minimally Invasive Surgery for Extraforaminal Lumbar Disk Herniation: A Systematic Review and Meta-Analysis. World Neurosurg 2017;108:924-38.e3. [Crossref] [PubMed]
- Parker SL, Mendenhall SK, Shau DN, et al. Minimally Invasive versus Open Transforaminal Lumbar Interbody Fusion for Degenerative Spondylolisthesis: Comparative Effectiveness and Cost-Utility Analysis. World Neurosurg 2014;82:230-8. [Crossref] [PubMed]
- Singh K, Nandyala SV, Marquez-Lara A, et al. A perioperative cost analysis comparing single-level minimally invasive and open transforaminal lumbar interbody fusion. Spine J 2014;14:1694-701. [Crossref] [PubMed]
- Stevens KJ, Spenciner DB, Griffiths KL, et al. Comparison of minimally invasive and conventional open posterolateral fusion using magnetic resonance imaging and retraction pressure studies. J Spinal Disord Tech 2006;19:77-86. [Crossref] [PubMed]
- Sharif S, Afsar A. Learning Curve and Minimally Invasive Spine Surgery. World Neurosurg 2018;119:472-8. [Crossref] [PubMed]
- Payer M, Walser H. Evacuation of a 14-vertebral-level Cervico-Thoracic Epidural Abscess and Review of Surgical Options for Extensive Spinal Epidural Abscesses. J Clin Neurosci 2008;15:483-6. [Crossref] [PubMed]
- Overley SC, Kim JS, Gogel BA, et al. Tandem Spinal Stenosis: A Systematic Review. JBJS Rev 2017;5:e2. [Crossref] [PubMed]
- Abd-El-Barr MM, Bi WL, Bahluyen B, et al. Extensive spinal epidural abscess treated with “apical laminectomies” and irrigation of the epidural space: report of 2 cases. J Neurosurg Spine 2015;22:318-23. [Crossref] [PubMed]
- Kurudza E, Stadler JA 3rd, Kurudza E, et al. Pediatric Holocord Epidural Abscess Treated with Apical Laminotomies with Catheter-directed Irrigation and Drainage. Cureus 2019;11:e5733. [Crossref] [PubMed]
- Hwang R, Yung BH, Sedney C, et al. Treatment of holocord spinal epidural abscess via alternating side unilateral approach for bilateral laminectomy. W V Med J 2015;111:14-16-8. [PubMed]
- Yukawa Y, Kato F, Ito K, et al. Laminoplasty and Skip Laminectomy for Cervical Compressive Myelopathy: Range of Motion, Postoperative Neck Pain, and Surgical Outcomes in a Randomized Prospective Study. Spine (Phila Pa 1976) 2007;32:1980-5. [Crossref] [PubMed]




