A radiographic follow-up study of stand-alone-cage and graft-plate constructs for single-level anterior cervical discectomy and fusion
Introduction
Anterior cervical discectomy and fusion (ACDF) is the gold standard treatment for surgical management of cervical radiculopathy refractory to non-operative measures. It is a procedure of low morbidity and the success rates are high. This is in part attributed to the very high fusion rate, particularly for single level procedures (1).
Complications, although rare, arise from time to time. Dysphagia and transient hoarseness can be anticipated in the immediate post-operative period but generally resolve quickly (2). Longer-term problems include pseudo arthrosis, adjacent segment disease (ASD), adjacent level ossification (ALO) and subsidence of the construct (1,3,4). Various strategies are used to reduce the risk of these occurring. Appropriate positioning of the plate anteriorly, more than 5 mm away from the adjacent disc is thought to minimize the risk of ASD and ALO (5). Suitable endplate preparation can be expected to enhance the likelihood of fusion.
A variety of implants are available for ACDF. Surgeons can choose from a variety of interbody devices including those manufactured from titanium, polyetherethylketone (PEEK) and allograft structural bone. Various modes of fixation are available and the main modality utilized is anterior plating. Some argue that the anterior plate is unnecessary, creating a prominence anteriorly predisposing to avoidable adjacent level problems such as ALO and swallowing difficulty (3). Stand-alone (SA) devices avoid the anterior prominence but some concern exists about their durability and biomechanical performance alongside the traditional cage and plate construct.
The aim of this study was to review the radiographic outcome of patient’s undergoing ACDF with either a SA device or a traditional cage and plate construct. The primary outcome of interest was implant subsidence while secondary outcome measures included both segmental and total lordosis.
Methods
This is a retrospective review of patients with cervical degenerative disc disease that underwent single level anterior cervical decompression and fusion for cervical radiculopathy by a single surgeon. The senior author used two different implants when performing an ACDF over the period under review. All other aspects of the procedure including operating room set-up, patient positioning, tractions, approach, technique and post-operative care were the same. Specifically, all patients were placed in Holter traction with 10 pounds of weight and traction pins were used to distract the disc space. As is the senior authors preference, all patients had a Jackson-Pratt drain inserted at the end of surgery and had this removed the following morning. All patients received a soft-collar for comfort for two weeks following surgery.
For the SA group, the Solitaire-CΤΜ cervical spacer system was used (Biomet). The spacer comprises a titanium alloy faceplate and PEEK-OPTIMA® body. Within the cage body, corticocancellous chips are placed along with bone shaving from the vertebral bodies and concentrated autologous bone marrow aspirate from the pelvis. One screw is placed into each of the caudal and cephalad vertebral bodies for fixation. In the graft and plate (GP) group, a corticocancellous allograft block, premachined (Biomet), was used for interbody support and the construct secured with the use of an anterior plate—MaxAn® Anterior Cervical Plate System (Biomet)—secured with two locked, fixed angle screws into each of the caudal and cephalad vertebral bodies.
Medical records were reviewed to collect demographic details and confirm diagnostic details. Radiographic records were obtained from the immediate post-operative period and the latest follow-up clinical visit. All radiographs were taken in the standing position. Patients without adequate cervical spine radiographs at follow up and those with prior cervical fusion procedures were excluded from the study.
Immediate postoperative and final follow up lateral radiographs were evaluated using Surgimap 2.1.8® (Nemaris, New York 2015, USA) to obtain measurements on subsidence, total and segmental lordosis. Radiographic calibration was confirmed by measuring the known screw diameter. Segmental height was measured drawing a line from cranial endplate of the proximal vertebral body to caudal endplate of distal body fused (Figure 1). Subsidence was defined as a decrease in the total intervertebral disc height between the two fused vertebral bodies and was determined by comparing the follow-up lateral radiographs with the first post-operative radiographs. A decrease in total intervertebral disc height >2 mm was considered to be significant subsidence. Global lordosis was measured using the inferior endplate of C2 and superior endplate of C7. Segmental lordosis was measured using the superior endplate of the cephalad and inferior endplate of the caudal vertebrae (Figure 2).


Statistical analysis
All data was anonymized and entered into a Microsoft Excel spreadsheet. Statplus for Mac was used for statistical analysis. T-tests and Chi-squared tests were applied where appropriate correlation coefficients were calculated where needed.
Results
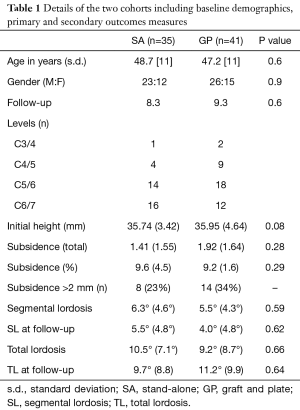
A total of 75 patients were eligible for inclusion. 35 underwent ACDF using the SA cage device while 41 underwent ACDF using a structural allograft and anterior plating. Basic demographics across the two groups were similar as was the mean follow-up (Table 1).
Full table
There was no statistically significant difference between the two groups in the primary outcome measure with a mean subsidence in the SA and GP groups of 1.41 and 1.92 mm respectively. When considering the proportion of cases in each cohort with a significant amount of subsidence (>2 mm), again no statistically significant difference was seen although the absolute proportion was higher in the allograft and plate group.
Neither total lordosis nor segmental lordosis were related to the degree of subsidence. When tested, there was no correlation in either grouped between cage size and amount of subsidence nor did the level of fusion have any relationship to the degree of subsidence.
Discussion
The aim of this study was to compare the radiographic outcomes in patients undergoing single level ACDF with either a SA interbody construct or with structural allograft and anterior plate system. The key finding is the similar amount and rate of subsidence with a SA construct when compared to the more established construct using an anterior plate. Furthermore, when considering clinically significant subsidence (>2 mm) there was greater absolute proportion of the graft-plate group with this finding although this finding failed to reach statistical significance.
Subsidence has always been a concern about using SA devices for ACDF. However, in addition to our findings that suggest subsidence is no worse in single level disease treated with a SA device, a retrospective review of 28 patients undergoing ACDF using SA PEEK cages reported by Dufour et al. found no subsidence (6). Additionally they used computed tomography for assessing fusion (94%) whereas we did not seek out this outcome measure—CT is only used by the senior author during the follow-up period for evaluating symptomatic patients (6).
Njoku et al. analyzed outcomes from ACDF using a zero-profile, SA PEEK interbody spacer in 41 patients with a mean follow-up of just over 18 months (7). At latest follow-up the mean subsidence was 4.1 mm (s.d. 4.7 mm) but this did not influence clinical outcome. They reported a higher fusion rate than elsewhere in the literature, also over 90%, using SA devices.
In a previous review of 82 cases, Kao et al. suggested that using a larger cage was associated with greater subsidence when using a SA PEEK cage (8). Accepting 3 mm as a significant amount of subsidence, 31/81 had evidence of subsidence. Additionally, they noted that subsidence was more likely at the lower levels (C5–7) than the upper (C2–5). Brenke et al. have shown that bone mineral density reduces in a craniocaudad direction in the cervical spine and this may in part explain the greater degree of subsidence at the lower levels (9). We did not demonstrate any relationship between level and amount of subsidence but admittedly our study may be under powered in this regard and we did however use a lower cut-off (2 mm) for accepting subsidence as significant hence our study is more sensitive.
In a study comparing tricortical graft with anterior plate and a cage-plate construct and cage alone, Lee et al. found that the cage alone resulted in a lower fusion rate and greater subsidence rate than the other two options (10). The conclusion was made that the anterior plating, irrespective of interbody construct protects against subsidence and enhances the chance of fusion. They did note that subsidence was evident in cases even with anterior plating and clinical outcomes were not different between the groups except for arm pain.
Lee et al. have also noted failure to demonstrate a relationship between subsidence and worse clinical outcome postulating that the lack of correlation is due to the preservation of posterior vertebral body height, segmental kyphosis and the overall preservation of cervical alignment (4). Song et al. reported a subsidence rate of 32% in cases treated with cage alone compared to 9% in those treated with a cage-plate construct (11). Again no difference between the two groups regarding clinical outcome was noted, a recurring theme in the literature (12-14). We have not considered pre-operative alignment in this series but have at least measured global alignment on the immediate post-operative radiograph without finding a relationship of alignment with amount of or incidence of subsidence.
Certain risk factors for increased amount or incidence of subsidence have been suggested. The presence of a global cervical kyphosis has been shown to result in increased risk of subsidence and hence may represent a contraindication to the use of SA devices (15). In one report by Lee et al., subsidence was almost 14 times more likely in those with pre-operative kyphotic alignment than in those with lordosis (15). Increased level of distraction at the operated level was suggested to a risk factor for increased subsidence while similarly an increased graft size has also been linked to increased subsidence (13,16).
We acknowledge our study has limitations. We have used a relatively small sample size but by restricting the analysis to single level disease we have eliminated the possible influence of multilevel surgery. Although we have compared a SA construct with a GP construct the interbody devices in each case were made from different material.
In summary, we found no significant difference in radiographic outcomes following ACDF in patients using either a cage-plate or an allograft bone-plate construct. Segmental and global lordosis was maintained in both groups. Although there was no statistically significant difference, the absolute proportion of patients with significant subsidence (>2 mm) was higher in the allograft and plate group. Future studies should aim to establish to potential role for SA constructs and the influence of biomaterials on graft subsidence.
Acknowledgements
JF Baker received the Joint RCSI/Gussie Mehigan Scholarship in support of Fellowship training.
Footnote
Conflicts of Interest: Dr. Baker reports personal fees from 3D4Medical, outside the submitted work, other authors have no conflicts of interest to declare.
Ethical Statement: This article does not contain any studies with human participants performed by any of the authors. Ethical Committee review was waived for this retrospective radiographic analysis.
References
- Shriver MF, Lewis DJ, Kshettry VR, et al. Pseudoarthrosis rates in anterior cervical discectomy and fusion: a meta-analysis. Spine J 2015;15:2016-27. [Crossref] [PubMed]
- Nemoto O, Kitada A, Naitou S, et al. Stand-alone anchored cage versus cage with plating for single-level anterior cervical discectomy and fusion: a prospective, randomized, controlled study with a 2-year follow-up. Eur J Orthop Surg Traumatol 2015;25:S127-34. [Crossref] [PubMed]
- Yang H, Chen D, Wang X, et al. Zero-profile integrated plate and spacer device reduces rate of adjacent-level ossification development and dysphagia compared to ACDF with plating and cage system. Arch Orthop Trauma Surg 2015;135:781-7. [Crossref] [PubMed]
- Lee CH, Kim KJ, Hyun SJ, et al. Subsidence as of 12 months after single-level anterior cervical inter-body fusion. Is it related to clinical outcomes? Acta Neurochir (Wien) 2015;157:1063-8. [Crossref] [PubMed]
- Kim HJ, Kelly MP, Ely CG, et al. The risk of adjacent-level ossification development after surgery in the cervical spine: are there factors that affect the risk? A systematic review. Spine (Phila Pa 1976) 2012;37:S65-74. [Crossref] [PubMed]
- Dufour T, Huppert J, Louis C, et al. Radiological analysis of 37 segments in cervical spine implanted with a peek stand-alone device, with at least one year follow-up. Br J Neurosurg 2010;24:633-40. [Crossref] [PubMed]
- Njoku I Jr, Alimi M, Leng LZ, et al. Anterior cervical discectomy and fusion with a zero-profile integrated plate and spacer device: a clinical and radiological study: Clinical article. J Neurosurg Spine 2014;21:529-37. [Crossref] [PubMed]
- Kao TH, Wu CH, Chou YC, et al. Risk factors for subsidence in anterior cervical fusion with stand-alone polyetheretherketone (PEEK) cages: a review of 82 cases and 182 levels. Arch Orthop Trauma Surg 2014;134:1343-51. [Crossref] [PubMed]
- Brenke C, Dostal M, Scharf J, et al. Influence of cervical bone mineral density on cage subsidence in patients following stand-alone anterior cervical discectomy and fusion. Eur Spine J 2015;24:2832-40. [Crossref] [PubMed]
- Lee CH, Hyun SJ, Kim MJ, et al. Comparative analysis of 3 different construct systems for single-level anterior cervical discectomy and fusion: stand-alone cage, iliac graft plus plate augmentation, and cage plus plating. J Spinal Disord Tech 2013;26:112-8. [Crossref] [PubMed]
- Song KJ, Taghavi CE, Lee KB, et al. The efficacy of plate construct augmentation versus cage alone in anterior cervical fusion. Spine (Phila Pa 1976) 2009;34:2886-92. [Crossref] [PubMed]
- Tomé-Bermejo F, Morales-Valencia JA, Moreno-Pérez J, et al. Degenerative cervical disc disease: long-term changes in sagittal alignment and their clinical implications after cervical interbody fusion cage subsidence: a prospective study with standalone lordotic tantalum cages. Clin Spine Surg 2017;30:E648-55. [PubMed]
- Yamagata T, Takami T, Uda T, et al. Outcomes of contemporary use of rectangular titanium stand-alone cages in anterior cervical discectomy and fusion: cage subsidence and cervical alignment. J Clin Neurosci 2012;19:1673-8. [Crossref] [PubMed]
- Zajonz D, Franke AC, von der Höh N, et al. Is the radiographic subsidence of stand-alone cages associated with adverse clinical outcomes after cervical spine fusion? An observational cohort study with 2-year follow-up outcome scoring. Patient Saf Surg 2014;8:43. [PubMed]
- Lee YS, Kim YB, Park SW. Risk factors for postoperative subsidence of single-level anterior cervical discectomy and fusion: the significance of the preoperative cervical alignment. Spine (Phila Pa 1976) 2014;39:1280-7. [Crossref] [PubMed]
- Yoo M, Kim WH, Hyun SJ, et al. Comparison between two different cervical interbody fusion cages in one level stand-alone ACDF: carbon fiber composite frame cage versus polyetheretherketone cage. Korean J Spine 2014;11:127-35. [Crossref] [PubMed]


