
Timing of surgery and radiotherapy in the management of metastatic spine disease: expert opinion
Introduction
Use of both surgery and radiotherapy in the treatment of metastatic disease of the spine continues to evolve. While surgery was previously limited to cases of neurologic deterioration during radiation, radioresistant tumors and failure of radiotherapy, the need for spinal stability (1) in patients experiencing mechanical back pain, as well as symptomatic epidural disease, has widened the indications for surgical intervention. Although the optimal timing of treatment is essential for both primary and metastatic tumors of the spine, it is especially true in the latter, where several landmark papers have demonstrated the benefit and cost effectiveness of combined surgery plus radiation treatment versus radiation alone (2-5).
The greatest concern when considering the proximity and time interval between radiation and surgical treatment is wound healing (6-8). If radiation treatment occurs in the early phases of healing, it may lead to breakdown in the treated area, depending on the total dose and frequency of radiation exposure (9-12). Moreover, this oncologic population is often malnourished, on steroids, chemotherapy and/or anti angiogenic factors, all of which contribute to further fragility of the tissues and impaired healing capacity. The optimal timing between radiation and surgery (and vice versa) is unknown and the clinical decision has up until now been guided by personal experience, rather than any clear guidelines; an alarming acknowledgement given the prevalence and importance of the clinical dilemma.
To try and help answer this question, a systematic review was done to determine the optimal timing between radiation and surgery (13). Very low-quality literature suggested that surgery within seven days of radiation increases the rate of postoperative wound complications. Timing of adjuvant radiotherapy following surgery was not specifically determined. The systematic review combined the literature on general principles of wound healing and effects of radiation on wound healing, to conclude the optimal radiotherapy-surgery/surgery-radiotherapy time interval should be at least one week; however numerous limitations weakens this conclusion. Furthermore, radiation treatment is evolving and three-dimensional conformal radiation therapy or stereotactic spinal radiotherapy is now being used in many centers, which may minimize the radiation dose to the skin at the surgical incision site and thus reduce the likelihood of complications due to wound healing. With limited guidelines from the best available literature on this sentinel clinical question, an evidence-based medicine (EBM) model of best available evidence plus consensus expert opinion is an essential next step.
The purpose of this study was to collate the opinions of experienced radiation oncologists and spine surgeons regarding the timing of radiation (both conventional and stereotactic) and surgery in order to produce an EBM decision aid. This information will help guide oncologists and surgeons in determining the optimal timing of radiation and surgical treatment for the management of metastatic spine disease.
Methods
Respondents
Ethical approval was obtained. Surveys were sent to radiation oncologists and spine surgeons at tertiary care centers throughout North America who regularly treat metastatic spine disease. Members of the Spine Oncology Study Group were all included and members asked to cascade the questionnaire to high volume departmental colleagues. Email, regular mail and a web-based questionnaire (www.surveymonkey.com) allowed confidential distribution of the survey. Physicians were asked to estimate the number of cases of spinal metastases they treat per year. Follow-up letters and email were sent to non-responders in order to elicit a response.
Survey
The survey consisted of four main components:
- The minimum time to wait before performing spine surgery after conventional radiation;
- The minimum time to wait before starting conventional radiation after uncomplicated spine surgery;
- The minimum time to wait before performing spine surgery after stereotactic radiation (1,800–2,400 cGy in 1 fraction);
- The minimum time to wait before starting stereotactic radiation (1,800–2,400 cGy in 1 fraction) after uncomplicated spine surgery.
In each scenario, respondents were asked to select either 1, 2, 3, 4–6 or >6 weeks.
Statistical analysis
Data was tabulated and analyzed in the form of a frequency distribution. The survey data were compiled and analyzed using Microsoft Excel (Microsoft Corporation, Redmond, WA, USA). The mode was used to summarize nominal data. Within the radiation oncologists and surgeon groups, two tail testing (P=0.05) was performed on the binomial probabilities. Furthermore, statistical testing of the difference between the radiation oncologists and surgeons was performed using a two-tail t-test. If necessary, subgroup analysis was performed with respect to the physicians who treated a higher volume of cases (21–30 or 30+ metastases cases per year).
Results
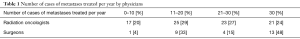
A total of 130 surveys were sent out (100 to radiation oncologists and 30 to specialist spine surgeons). In total, 113 replies (87%) were received (86 from radiation oncologists and 27 from spine surgeons). The treatment demographics of the respondents are presented in Table 1.
Full table
Thirteen out of the 27 responding surgeons (48%) treated more than 30 cases of spinal metastases per year while the distribution was more evenly spread amongst the radiation oncologists (z=2.345; P=0.019) (Table 1).
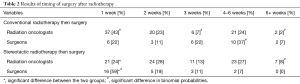
Timing of surgery after radiotherapy
Table 2 shows the results of the practices of the radiation oncologists and spine surgeons on the timing of surgery after both conventional and stereotactic radiotherapy. One respondent did not answer the question on stereotactic surgery. Consensus differed between the radiation oncologists and surgeons with regard to conventional radiotherapy: 43% of radiation oncologists advocated a 1-week delay after conventional radiotherapy, whereas 37% of surgeons preferred to wait 4–6 weeks before surgery (z=−1.94; P=0.05), with the majority of surgeons preferring to wait 3 weeks or more (66%) (z=3.03; P=0.002). Subgroup analysis of the higher volume physicians revealed that 10 out of 17 surgeons would wait at least 4–6 weeks to operate after a patient with spinal metastases received conventional radiotherapy compared to 13 out of 44 radiation oncologists (z=2.12; P=0.03). However, there is consensus if the total number of respondents in the 1- and 2-week groups are combined (58%; 38% suggesting 1 week and 20% suggesting 2 weeks).
Full table
A similar but reversed disparity in opinion is seen in the case of stereotactic radiotherapy preceding surgery. While there was no overall consensus amongst the radiation oncologists, 59% of surgeons would be prepared to proceed with surgery one week after stereotactic radiotherapy compared to 24% of radiation oncologists (z=−3.37; P=0.0008). Subgroup analysis of the 17 high volume surgeons showed that 11 spine surgeons consider surgery after stereotactic radiotherapy a safer option, with these 11 respondents reducing the time they would wait compared to conventional radiotherapy. This optimistic view regarding stereotactic radiotherapy is not shared by the radiation oncologists, where only 5 out of the 44 high volume group (20–30 metastases and 30+ metastases per year) would reduce the time for wound healing after stereotactic radiation (z=−4.25; P<0.0002). However, once again, there is consensus if the total number of respondents in the 1- and 2-week groups are combined (59%; 33% suggesting 1 week and 26% suggesting 2 weeks).
Timing of radiotherapy after surgery
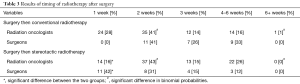
Table 3 shows the results of timing of conventional and stereotactic radiotherapy after surgery. The results here are much more concordant, with joint consensus between both groups indicating that the optimum time for conventional radiotherapy after surgery is 2 weeks (41% of radiation oncologists and surgeons) (z=−0.004; P=0.997).
Full table
Slight disparity is seen in the case of stereotactic radiotherapy treatment after surgery with 43% of radiation oncologists, but only 30% of surgeons advocating a 2-week delay (z=1.25; P=0.22); 41% of surgeons suggest a 1-week delay is sufficient (z=−2.67; P=0.008). However, there is consensus if the responses of the 1- and 2-week groups are combined (59% of radiation oncologists and 73% of surgeons) (z=−1.03; P=0.30). Subgroup analysis of the 17 high volume surgeons demonstrates that 13 consider stereotactic radiotherapy after surgery a safer option. Again, the optimism shared by the surgeons with regard to stereotactic radiotherapy is not shared by the radiation oncologists, where only 10 out of the 44 high volume group would reduce the time for wound healing after stereotactic radiotherapy.
Discussion
The timing of surgical and radiotherapy treatment is encountered frequently in the management of spine oncology. A systematic review (13) showed that there was a paucity of good quality literature which directly addressed this specific concern. An assimilation of the current evidence together with an understanding of the effects of radiation on wound healing lead the authors to recommend an interval of at least one week between radiotherapy and surgery and vice versa for the treatment of spinal metastases, regardless of the type (conventional or stereotactic) of radiotherapy given.
Timing of surgery after radiotherapy
Interestingly, expert opinion is divided between radiation oncologists and surgeons on the timing of surgery following radiation therapy. The consensus amongst surgeons is to wait 4–6 weeks to operate after conventional radiotherapy whereas radiation oncologists advocate only a 1-week time interval. This disparity may be a reflection of the treatment pathway and the timing of subsequent clinical follow-up. Wound complications are devastating events often necessitating reoperations, delaying systemic treatment and prolonging the hospital length of stay for this fragile oncologic population with limited life expectancy. It is the surgeon, more than the radiation oncologist, who deals first hand with the wound complications, possibly giving the radiation oncologist a biased impression surrounding the wound complication rate.
The opinion of radiation oncologists regarding the optimal timing of surgery following stereotactic radiotherapy was divided relatively homogenously. In the subgroup analysis, radiation oncologists actually consider this form of radiotherapy to lead to a greater risk of wound complications compared to conventional radiotherapy treatment. In contrast, surgeons hold a very optimistic view with the majority advocating safe surgery just one week following a stereotactic procedure. Clinical experience in this field is limited as shown by the paucity of literature on the matter. Wound healing in patients who underwent stereotactic radiosurgery (SRS) prior to surgery was discussed in only two studies (14,15) including nine patients and the interval between procedures was not specified. As a result, the surgical viewpoint may be biased by a lack of true clinical evidence, reliance on theoretical knowledge, and anecdotal evidence from experienced centers.
Combining clinical data and the current practices of experienced radiation oncologists and spine surgeons allows us to draw firm recommendations for the optimal timing of surgical treatment after conventional radiotherapy. Data from a systematic review, the understanding of wound healing process, as well as opinion from surgeons and radiation oncologists would support a minimum of a one-week interval and preferably a 2-week interval between radiation (regardless of type) and spine surgery. Published cases of surgery undertaken within a week of radiation, were due to clinical deterioration during radiation treatment. Acute neurological deterioration, as well as emergent surgical decompression may certainly contribute to higher rates of wound complications. In subjectively weighing all the variables, from best available evidence and consensus expert opinion, a qualitative assessment would be to wait 2 weeks for surgery after conventional or stereotactic radiotherapy and at minimum one week.
Timing of radiotherapy after surgery
From a purely histological perspective, we know that radiation has the greatest negative impact during the inflammatory and proliferative phase of wound healing. This occurs in the first week, when collagen production by fibroblasts is at its peak (9,10,16-19).
Very limited data is available on wound complications when SRS is employed post-operatively. Available literature (14,15,20-23) suggests that treatment with surgery followed by SRS may pose less risk to postoperative healing compared to the combination of surgery and conventional radiotherapy. The same literature also suggests that the wound complication in patients undergoing SRS is significantly greater in cases of previous exposure to conventional radiation.
Current practice amongst experienced radiation oncologists and spine surgeons is concordant and suggests that a 2-week delay for conventional radiotherapy after surgery is sufficient. Expert opinion on the optimal time interval between surgery and stereotactic radiotherapy is slightly different between the two groups, surgeons being once again more confident in recommending stereotactic treatment earlier than their radiation oncologist colleagues.
Combining consensus expert opinion with the published literature allows us to recommend a 2-week delay for conventional radiation therapy after uncomplicated spine surgery. This delay is usually clinically acceptable since spinal cord decompression and stabilization of the spinal column are usually accomplished with surgery. A recommendation of a 2-week time interval is also made for the case of post-operative SRS. However, based on surgeons’ opinion and the limited available literature, it seems than a shorter time interval could be reasonable, but warrants further clinical research.
Our study is limited by the small number of spine surgeons compared to the radiation oncologists; however, this reflects the specialized nature of this field of surgery and indeed many of these surgeons who completed the survey are experienced key opinion leaders. The results of this study along with the previous systematic review still only provide at best class III evidence, according to the criteria for the classification of evidence developed by the U.S. Preventative Services Task Force (24).
The study does however represent the EBM model of best available evidence plus expert opinion to facilitate clinical decision-making. The findings may be applied in the context of clinical experience and circumstances, including patient preference. Moreover, it provides a foundation on which to move forward with a large prospective multi-center study to generate the numbers of patients and cohorts needed to determine the optimal timing of surgery and radiation for the management of spinal metastases with a higher level of scientific integrity.
Conclusions
Based on the available literature and understanding the practices of experienced radiation oncologists and spine surgeons regarding the timing of radiation (both conventional and stereotactic) and surgery, the authors provide an EBM recommendation to guide oncologists and surgeons in determining the optimal timing of radiation and surgical treatment for the management of metastatic spine disease. We recommend that the interval between radiotherapy (either stereotactic or conventional) and surgery (and vice versa) should ideally be a minimum of 2 weeks.
Acknowledgements
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
Ethical Statement: Ethical approval was obtained.
References
- Fisher CG, DiPaola CP, Ryken TC, et al. A novel classification system for spinal instability in neoplastic disease: an evidence-based approach and expert consensus from the Spine Oncology Study Group. Spine (Phila Pa 1976) 2010;35:E1221-9. [Crossref] [PubMed]
- Falicov A, Fisher CG, Sparkes J, et al. Impact of surgical intervention on quality of life in patients with spinal metastases. Spine 2006;31:2849-56. [Crossref] [PubMed]
- Patchell RA, Tibbs PA, Regine WF, et al. Direct decompressive surgical resection in the treatment of spinal cord compression caused by metastatic cancer: a randomised trial. Lancet 2005;366:643-8. [Crossref] [PubMed]
- Thomas KC, Nosyk B, Fisher CG, et al. Cost-effectiveness of surgery plus radiotherapy versus radiotherapy alone for metastatic epidural spinal cord compression. Int J Radiat Oncol Biol Phys 2006;66:1212-8. [Crossref] [PubMed]
- Furlan JC, Chan KK, Sandoval GA, et al. The combined use of surgery and radiotherapy to treat patients with epidural cord compression due to metastatic disease: a cost-utility analysis. Neuro Oncol 2012;14:631-40. [Crossref] [PubMed]
- Chadwick MA, Vieten D, Pettitt E, et al. Short course preoperative radiotherapy is the single most important risk factor for perineal wound complications after abdominoperineal excision of the rectum. Colorectal Dis 2006;8:756-61. [Crossref] [PubMed]
- O'Sullivan B, Davis AM, Turcotte R, et al. Preoperative versus postoperative radiotherapy in soft-tissue sarcoma of the limbs: a randomised trial. Lancet 2002;359:2235-41. [Crossref] [PubMed]
- Schwartz SR, Yueh B, Maynard C, et al. Predictors of wound complications after laryngectomy: A study of over 2000 patients. Otolaryngol Head Neck Surg 2004;131:61-8. [Crossref] [PubMed]
- Wang J, Boerma M, Fu Q, et al. Radiation responses in skin and connective tissues: effect on wound healing and surgical outcome. Hernia 2006;10:502-6. [Crossref] [PubMed]
- Tibbs MK. Wound healing following radiation therapy: a review. Radiother Oncol 1997;42:99-106. [Crossref] [PubMed]
- Payne WG, Naidu DK, Wheeler CK, et al. Wound healing in patients with cancer. Eplasty 2008;8. [PubMed]
- Hom DB, Unger GM, Pernell KJ, et al. Improving surgical wound healing with basic fibroblast growth factor after radiation. Laryngoscope 2005;115:412-22. [Crossref] [PubMed]
- Itshayek E, Yamada J, Bilsky M, et al. Timing of surgery and radiotherapy in the management of metastatic spine disease: a systematic review. Int J Oncol 2010;36:533-44. [PubMed]
- Degen JW, Gagnon GJ, Voyadzis JM, et al. CyberKnife stereotactic radiosurgical treatment of spinal tumors for pain control and quality of life. J Neurosurg Spine 2005;2:540-9. [Crossref] [PubMed]
- Levine AM, Brenner M, Coleman C, et al. Surgical wound complications in patients treated with CyberKnife stereotactic radiosurgery for tumors of the spine. In Editor (ed): Surgical wound complications in patients treated with CyberKnife stereotactic radiosurgery for tumors of the spine. Hollywood, Florida: CyberKnife User's Meeting, 2009.
- Shamberger R. Effect of chemotherapy and radiotherapy on wound healing: experimental studies. Recent Results Cancer Res 1985;98:17-34. [Crossref] [PubMed]
- Gu Q, Wang D, Cui C, et al. Effects of radiation on wound healing. J Environ Pathol Toxicol Oncol 1998;17:117-23. [PubMed]
- Grillo HC, Potsaid MS. Studies in wound healing. IV. Retardation of contraction by localx-irradiation, and observations relating to the origin of fibroblasts in repair. Ann Surg 1961;154:741-50. [PubMed]
- Dobbs W. A statistical study of the effect of roenttgen rays on wound healing. AJR 1939;41:625-32.
- Gagnon GJ, Nasr NM, Liao JJ, et al. Treatment of spinal tumors using cyberknife fractionated stereotactic radiosurgery: pain and quality-of-life assessment after treatment in 200 patients. Neurosurgery 2009;64:297-306; discussion 306-7. [Crossref] [PubMed]
- Harel R, Chao S, Krishnaney A, et al. Spine instrumentation failure after spine tumor resection and radiation: comparing conventional radiotherapy with stereotactic radiosurgery outcomes. World Neurosurg 2010;74:517-22. [Crossref] [PubMed]
- Moulding HD, Elder JB, Lis E, et al. Local disease control after decompressive surgery and adjuvant high-dose single-fraction radiosurgery for spine metastases. J Neurosurg Spine 2010;13:87-93. [Crossref] [PubMed]
- Rock JP, Ryu S, Shukairy MS, et al. Postoperative radiosurgery for malignant spinal tumors. Neurosurgery 2006;58:891-898; discussion 891-8. [Crossref] [PubMed]
- Harris RP, Helfand M, Woolf SH, et al. Current methods of the US Preventive Services Task Force: a review of the process. Am J Prev Med 2001;20:21-35. [Crossref] [PubMed]


