
Surgeon motivation, and obstacles to the implementation of minimally invasive spinal surgery techniques
Introduction
The authors of this publication were interested in better understanding the current motivators and deterrents for spine surgeons to implement minimally invasive spinal surgery techniques (MISST) into the day-to-day practice and how these factors could impact the clinical decision-making process in the choice of surgical treatment of common degenerative conditions of the lumbar spine. MISST has developed some significant traction among spine surgeons (1). The lower complication rates with MISST, when compared to of open lumbar spine surgery, has become common knowledge among patients as well (2-5), who are now actively seeking out surgeons and MISST centers (6-8) to receive treatments that are less disruptive to their lives, allow earlier social reintegration, and return to work. Avoiding some of the traditional stigmas of inpatient open lumbar spine surgery by reducing the time to postoperative narcotic independence and diminishing the burden on patients caused by poorly managed postoperative transition of care episodes has become part of this public discussion among its stakeholders who have established the value proposition of the various MISST by demonstrating their safety and efficacy for a number of clinical indications (9).
The obvious is embraced and hardly disputed by nearly everyone: MISST is publically associated with fewer postoperative complications, shorter interval for return to work and an overall reduced burden to patients and the healthcare delivery system. Evidence has emerged to corroborate these ideas from a clinical equivalency point of view stating that MISST outcomes are no worse and at a minimum similar to open spine surgery (10-13). Lower expenditure for un-intended aftercare and readmission associated with decompensated cardiopulmonary medical comorbidities or diabetes mellitus often seen following open lumbar spinal surgery (14-18) alongside with reduced utilization of painkillers has been reported to drive the cost reductions (19). The latter problem is of significance in lieu of the opiate abuse epidemic in the United States (20-22). Therefore, it is no surprise that application of MISST has been shown to be associated with higher patient acceptance (13) due to less approach-related access trauma and surgical pain, fewer anesthesia-related problems (postoperative nausea) (14), and lower exposure to the risk of hospitalization including surgical site complications, medication errors, and hospital-acquired infections. These factors in combination with a recent push by payers to transition simple lumbar decompression surgeries into a more cost-effective outpatient setting have led to a substantial increase of lumbar MISST surgeries being done in an ambulatory surgery center; often under local anesthesia, sedation, and in some cases without intubation (11-13).
While these overarching goals are universally agreed upon, individual implementation from surgeon to surgeon, or institution to institution may substantially vary as the application of MISST is carried out in a different local context, where competing demographic, economic, and health care policy agendas may have a supportive or conflictive impact on MISST implementation and utilization. Some MISST may be associated with higher upfront direct cost due to additional capital and disposable expenses before producing cost savings in the long run (13). Spinal surgeons are not immune to these underlying dynamics. They may locally face very different circumstances in which they are wanting or are being asked to implement a MISST spinal surgery program.
Therefore, the purpose of this study was to understand better what motivates spine surgeons in today’s healthcare environment to implement MISST in relationship to their training and which obstacles they perceive as relevant in their pursuits. Also, the authors were interested in analyzing how spine surgeons attempted to validate their local MISST clinical program to overcome any implementation obstacles. The authors intend to further this opinion-based research with future studies to understand better what drives decision making in common yet controversial clinical questions in spinal surgery.
Methods
The authors solicited responses to an online survey via email, and chat groups in social networks including Facebook, WeChat, WhatsApp, and LinkedIn. The survey was available online and distributed via a link distributed through these social network media to surgeons worldwide. Upon clicking on the link, the prospective surgeon respondent was taken to the typeform website at www.typeform.com where the survey opened automatically. The survey could be answered on the computer, laptop, and any hand-held devices such as an iPad, or a cellular smartphone. The typeform services were chosen because of its ease of use across multiple user-interface platforms. Survey accessibility on the personal smartphone by the surgeon was considered a significant advantage to facilitate recruitment of respondents, ease of use, and respondent’s retention to improve survey completion.
The survey consisted of five questions. The questions were aimed at soliciting information deemed to be important motivators or deterrents of MISST implementation, whereas another question requested demographic information of the respondent including the gender, age, country of residence, practice setting, extent of postgraduate residency and fellowship training, and the percentage of his/her practice being devoted to MISST. Instead of user queries with a Likert scale, the survey was constructed of either simple “YES” or “NO” questions, or simple multiple-choice questions some of which with multiple possible answers for ease of use and to maximize respondent retention once on the web site and to facilitate survey completion. Surgeons were asked the following five questions:
- Tell us a little about yourself:
- What postgraduate residency training did you complete (please select one response)?
- Neurosurgery.
- Orthopaedic surgery.
- Other.
- Did you complete a fellowship is spine surgery (yes/no)?
- What percentage of your practice is devoted to MIS (please select one response)?
- I don’t exactly know.
- <25%.
- 25–50%.
- 50–75%.
- >75%.
- Which avenue did you use to train for the MISST you currently employ in your clinical practice today (please select all responses that apply)?
- I attended workshops and local meetings.
- I attended national and international meetings.
- I learned from likeminded peers in small groups.
- What is or was your primary motivation to implement MISST into your clinical practice (please select all responses that apply)?
- Personal interest.
- Patient demand.
- I use it for marketing & business development of my medical practice.
- I perceive pressure from my peers and colleagues.
- I am pressured by my organization to implement MISST.
- I am afraid of being left behind and my practice could be perceived as outdated.
- Which obstacles to MISST implementation apply to you (please select all responses that apply)?
- There are no obstacles.
- Lack of industry support.
- High upfront equipment cost is hindering me implementing MISST.
- High cost of disposables is problematic.
- Reimbursement is too low to economically justify MISST.
- Health insurance denial.
- MISST is considered experimental, outside the treatment- or coverage guidelines.
- How do you validate your clinical MISST program (please select all responses that apply)?
- I organize and present data of my clinical MISST program at local meetings.
- I attend and try to present data of my clinical MISST program at national and international meetings.
- I seek the exchange of ideas in small groups of likeminded peers.
- I seek validation of my clinical MISST program with peer-reviewed journal publications.
The survey ran from October 26 to November 14, 2018. The authors were blinded as to the identity of the responding surgeon at all times. Individual personal identifiers were not recorded. The typeform.com survey created a time-stamp upon initiation of the study and once the completed questionnaire was submitted. Also, a unique network identifier (ID without IP address) was recorded for each responding surgeon. Upon completion of the survey, the responses were downloaded in an Excel file format and imported into IBM SPSS (version 25) statistical software package for further data analysis.
Descriptive statistic measures were used to count responses and calculate the mean, range, and standard deviation as well as percentages. Wherever applicable, a P value of 0.05 or less was considered statistically significant, and a confidence interval of 95% was considered for all statistical tests. The responses from spine surgeons to the five questions were analyzed as categorical variables. The authors also used linear regression and kappa analysis of agreement in an attempt to measure the presumed consistency of the submitted responses in real time as they came in in lieu of unknown sample size required to have sufficient power for clinically meaningful statistical analysis.
Results
The online survey was accessed by 430 surgeons, of which 293 submitted a survey recording 292 submissions as valid responses. The survey site had 500 total visits. The completion rate was 67.4% and the average time to complete the survey was 08 minutes and 54 seconds. Twenty-eight surgeons completed the survey on a PC or laptop with 37 total and 34 unique visits with a completion rate of 87.5% and average time to finish 2 minutes and 30 seconds. The majority of surgeons [261] responded to the survey using their smartphones during 459 total and 395 unique visits with a completion rate of 66.1% taking an average time of 09 minutes and 38 seconds to complete. Only one surgeon used a tablet to complete the survey.
The vast majority of responding surgeons were male (94.8%) versus female surgeons accounting for 3.8% of respondents. Four surgeons preferred not to indicate their gender (1.4%). The age group crosstabulation by region showed that most responding spinal surgeons were between the age of 34 and 45 years of age in Asia (52.2%), Africa & Middle East (50.0%), North America (36.2%), and South America (33.3%). The majority of responding surgeons in Europe was between the ages of 44 and 55 (38.9%). In descending order, most responding surgeons were from Mexico (27.6%), China (16.8%), Brazil (10.8%), India (5.9%), United States (4.2%), Germany (2.8%), Taiwan (2.8%), Colombia (2.4%), South Korea (2.4%), Argentina (2.1%), Egypt (2.1%), Spain (1.4%), Italy (1%), and other countries (16.8%).
A regional breakdown of responding surgeons showed the majority of them were residing in North America (32.2%) and Asia (31.1%), followed by South America (18.5%), and Europe (12.3%). The majority of surgeons (170/292; 58.2%) participating in this survey were orthopaedic surgeons, followed by neurosurgeons (99/292; 33.9%), and a small group of surgeons (23/292; 7.9%) who indicated that they completed another form of postgraduate residency program (Table 1). Concerning their practice setting, 42.8% reported that they worked in groups of 2–10 peers, followed by 17.4% of surgeons indicating they were part of an organization employing 11–50 peers.
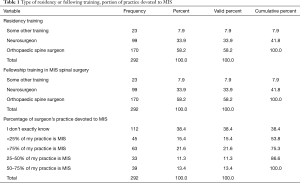
Full table
The vast majority (251; 86.0%) of the 292 responding surgeons were not fellowship trained in MISST. In contrast, only 14.0% (41/292) of surgeons had completed a MISST fellowship at the time they returned the survey. Thirty-five percent of spine surgeons indicated that more than half of their practice involves MISST cases compared to 26.7% who reported less than half of their cases employing MISST. The remaining 38.4% of surgeons were unsure what the exact percentage of MISST cases in their practice was (Table 1). The majority of spine surgeons (183/292; 62.7%) admitted to getting there continued medical education in the area of MISST from national and international meetings, followed by local meetings (139/292; 47.6%) in their area that they either organized, or attended, and from meetings in small groups (93/292, 31.8%) of like-minded peers.
Opinion research on their primary motivation for the implementation of a MISST program into their clinical practice revealed that spine surgeons listed their interest as the number one motivating factor (241/292; 82.5%). Patient demand (142/292; 48.6%) was the second most common reason why spine surgeons were implementing MISST into their clinical practice. Another significant group of spine surgeons admitted to using MISST to market themselves (59/292; 20.2%) and to drive business to their practice (Table 2). Other factors thought to be of relevance to the team of investigators of this study, such as pressure from peers and colleagues (17/292; 5.8%), pressure from their practice or employing organization (16/292; 5.5%), or fear of being left behind by their competitors and fear of negative impact on their reputation if they were not using MISST in their local health care markets (36/292; 12.3%), were of lesser concerns to the responding surgeons.
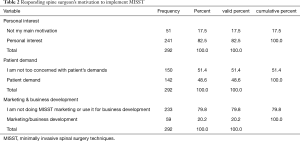
Full table
Of the 292 spine surgeons who completed the survey, 218 (74.7%) indicated that they encountered obstacles with MISST implementation (Table 3). Spine surgeons universally listed the high cost of capital equipment purchases (141/292; 48.3%) necessary to successfully launch such a formalized program and high cost of disposables (85/292; 29.1%) as the leading obstacles. Health insurance company’s preauthorization request denials were the third most common reason of failure to implement MISST programs reported by responding spine surgeons (62/292; 21.2%). Low reimbursement (48/292; 16.4%) or being told that MISST are outside accepted clinical treatment and coverage guidelines (36/292; 12.3%) were less commonly reported obstacles. Only 35 of 292 (12.0%) responding spine surgeons indicated that their MISST program was actively sponsored by industry (Tables 3 and 4).
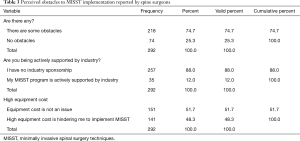
Full table
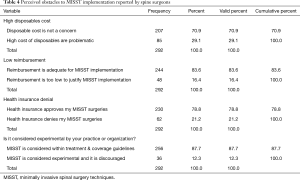
Full table
Spine surgeons were also polled as to how they use validation of their local MISST program. Over half of the responding spine surgeons (153/292; 52.4%) did not organize or present data of their clinical MISST program at local meetings implying that MISST utilization in their surgical practice did not impact their referrals. However, the remaining 47.6% (139/292) of spine surgeons were keenly aware of the need to present clinical data of their MISST program in local meetings that they either organized or attended. A more substantial portion of spine surgeons (183/292; 62.7%) utilized bigger national and international meeting venues to validate the status of the local MISST program. Nearly an equal one third of the polled spine surgeons submitted their clinical MISST data in the form of articles (105/292; 36.0%) for publication to peer-reviewed medical journals for validation purposes, and another one third preferred to validate data of their clinical MISST program in intellectual exchanges (93/292; 31.8%) in their familiar circles of small groups of like-minded peers. Kappa analysis of agreement and linear regression analysis of nominal variables recoded into numerical variables showed consistent asymetric distribution of variances of variables tested suggesting consistency in the responses as the survey submissions increased over the three-week data acquisition time.
Discussion
The authors solicited responses to an online survey from spine surgeons residing in Asia and other countries. The survey was distributed via email and social media. Average response rates have been reported for an in-person survey at 57%, mail survey at 50%, email survey at 30%, online survey at 29%, telephone survey at 18%, an in-app survey of 13%, with an overall average survey response rate of 33% (23-29). Clinical examples include a postal survey sent to 2,048 prospective respondents with a response rate of 46% (30). Another web-based 59 items survey with 260 respondents had a response rate of 60% (31), and a written paper survey reported a response rate of 49.5% (302/610) (32). An online patient satisfaction survey in 9,975 Medicare beneficiaries with 434 unduplicated survey submissions had a response rate of 4.3% (33). Clinical opinion survey research amongst spine surgeons showed response rates ranging from 49% (n=51) obtained in a study on surgical management of spinal stenosis amongst Norwegian spine surgeons (34), to 61.3% (n=357) amongst members of the Scoliosis Research Society surveyed on use of MIS Techniques in the Treatment of Adult Spinal Deformity (35). In comparison, another sizeable online survey study sent to trauma, spine and craniomaxillofacial surgeon members of the AO Foundation, yielded 1,212 valid and completed submission at an overall response rate of 4.1% (36). These examples illustrate that there can be a wide range of survey response rates and that 67.4% obtained in this study is higher than the average reported for clinical online survey research.
This survey on training and skill level of MISST amongst spine surgeons was blinded, and the team of authors had no information as to the identity of the responding spine surgeons, hence, minimizing the impact of intuition and hindsight bias amongst the investigators. With a response rate of 67.4%, the authors also considered the impact of non-response bias less problematic since it was still higher than the average reported response rates in several surveys amongst spine surgeons which were published in well-respected journals. Non-response bias has been recognized as an indicator of survey quality. Although lower response rates in the 20% range have been related to more accurate measurements than surveys with 60% to 70% response rates which are still considered preferable since the missing data have not been found to be random (37). Nonetheless, there could have been geographic bias where the digital communication used in this survey study could have obliterated existing geographic diversity and various cultural perspectives of responding spine surgeons. Therefore, the authors were cautious not to generalize the findings of this survey in the context of their preconceived notions of MISST and to counter the homogenizing effect of the digital data acquisition across multiple cultural boundaries while recognizing its limitations in the quest for genuinely alternative insights by other surgeons. To minimize the potentially distorting effects of such geographic biases, this team of authors from multiple countries in Asia, the Americas, and Europe worked closely together on the survey data analysis and interpretation taking the cultural diversities among respondents in the practice of MISST into account.
Findings of this opinion survey of 292 spine surgeons who returned a completed online questionaire indicate that the primary motivation to implement MISST into their day-to-day practice was personal interest (82.5%) and patient demand (48.6%). Other motivators, such as marketing their practice (20.2%), peer-pressure (5.8%), and fear of their clinical practice being considered outdated and being left behind (12.3%) were by far less of a priority to spine surgeons. This suggests that MISST is embraced by the vast majority of spine surgeons as mainstream and considered integral part of their clinical practice.
Nearly three-quarters of spine surgeons polled (74.4%) reported some sort of an obstacle preventing them to effectively implement an MISST program. A current breakdown of the most significant implementation hurdles shows that their innovation attempts are being hampered by high cost of new capital equipment purchases (reported by 48.3% of surgeons) and high cost of disposables (reported by 29.1% of surgeons) suggesting that they are getting pushback from their institutions where they are wanting to perform MISST surgeries because higher upfront implementation cost and higher ongoing operational costs. Low reimbursement (reported by 16.4% of surgeons) was reported to be less of an issue as this team of authors expected. However, it is unclear whether surgeons only reflected on their professional fees, or on the facility fee paid to the institution where the surgeries were conducted. It is reasonable to assume that high cost for equipment and disposables is also an issue for the health care institution where MISST is being implemented. Industry support to absorb some of these high upfront and ongoing operational costs was reported by only 12% of spine surgeons. The authors of this survey have no further information as to the details of these arrangements. However, it seems clear that industry does play a role in overcoming MISST implementation hurdles and that they should be studied further. Preauthorization denials by health insurance companies alongside with pushback for seemingly attempting to perform MISST surgeries that are not considered within accepted treatment and coverage guidelines was less problematic than previously reported. This suggests that MISST today has gained in acceptance among the stakeholders of the patient care equation (38-40).
Validation of their local MISST program was sought by nearly half of the responding spine surgeons (47.6%) who did so by organizing, attending and presenting clinical data of their MISST program in local meetings and at national and international meetings venues (62.7%). The authors of this study were also surprised by the high percentage of spine surgeons who validated their clinical program with articles submitted to peer-reviewed medical journals (36%). This clearly suggests that a third of the spine surgeons polled recognized the burden of proof to justify the rationale for their innovation attempts during the MISST implementation. Unfortunately, this survey did not collect any information as to whether this subset of publishing surgeons was predominately in academic setting or not. Other means of MISST validation were used by another one third of responding surgeons who preferred exchanging ideas on MISST (31.8%) in their familiar circles of small groups of like-minded peers. Obviously, this mode of validation is less cumbersome and involves less formal analysis of clinical data and is the easiest way to position one’s clinical MISST program within the norm of what is being performed by others but does not exceed beyond level V evidence (personal communication).
The online survey proofed an effective means of collecting tangible clinical information from spine surgeons in real time. This survey reached 430 surgeons with 292 valid submissions. The completion rate was 67.4% and surgeons that used a computer or laptop took significantly less time to complete. The smartphone accessibility of the survey clearly extended its reach to more surgeons who could respond on-the-go anytime and anywhere regardless of busy work schedules. However, the average time to completion more than tripled when using a smartphone (08:54) as if a computer or laptop was used. Presumably, the smaller screen size on the smartphone is of disadvantage when conducting a survey on complex clinical questions.
Analyzing the training background of the spine surgeons who responded to the survey revealed that the majority of them were orthopaedic surgeons (58.2%), followed by neurosurgeons (33.9%), and another small group of surgeons (7.9%) who completed another form of postgraduate residency program. This team of authors was surprised by the low percentage (14%) of responding spine surgeons performing MISST who had completed a formal spine fellowship. In spite of lack of formal fellowship training in the majority (86%) of spine surgeons, 61.6% of them indicated that a substantial portion of the clinical practice was devoted to performing MISST surgeries suggesting that they were self-taught. Unfortunately, this survey did not collect any information on how many years in practice these responding surgeons were after graduating from the respective postgraduate training programs. Neither did the survey obtain any information as to whether spine fellowships are keeping up with the fast-moving field of MISST. However, the survey implies that they are not, or at a minimum not the training centers of contemporary MISST. In fact, most surgeons (47.6%) received their MISST training in small workshops corroborating the idea of spine fellowships lagging behind in teaching contemporary MISST.
This survey study on motivation for MISST implementation amongst spine surgeons, and the types of obstacles they encountered had the advantage of blinded responses which minimized the impact of intuition and hindsight bias amongst the investigators. After all, the study investigators did not know the distribution of responses and which underlying trends would emerge when the survey launched. Hence, it was unclear at the outset of the online data acquisition when sufficient statistical sample size would have been achieved to close the survey. Linear regression monitoring of the change in response rates to the questions over the three-week period and kappa analysis of agreement in the 292 survey submissions showed a relatively stable distribution of asymmetric variances suggesting that similar percentage response rates could have been reasonably expected with a broader polling sample. Therefore, the authors of this study are confident that results presented herein are in fact representative of current opinions regarding MISST implementation amongst spine surgeons.
Conclusions
This online survey reached 430 spine surgeons in just three weeks suggesting that making a questionnaire accessible on a hand-held device facilitates data acquisition. Personal interest and patient demand were the main motivators for spine surgeons to implement MISST into their clinical practice. High cost for upfront capital equipment purchase and high ongoing operational expenses for disposables was listed as the most significant obstacles to MISST implementation. One third of surgeons validated their clinical MISST with peer-reviewed journal articles, and another third preferred personal exchange in small familiar circles of like-minded peers. Two-thirds of responding spine surgeons attended national and international meetings to validate the position of their local MISST program. This survey clearly indicates that MISST have become mainstream in spinal surgery. Local workshops and meetings in small groups instead of spine fellowships are the main knowledge sources for spine surgeons trying to implement MISST.
Acknowledgments
None.
Footnote
Conflicts of Interest: The first author has no direct or indirect conflicts. This manuscript is not meant for or intended to endorse any products or push any other agenda other than the associated clinical outcomes with endoscopic spine surgery. The motive for compiling this clinically relevant information is by no means created and/or correlated to directly enrich anyone due to its publication. This publication was intended to substantiate contemporary endoscopic spinal surgery concepts to facilitate technology advancements. JF Ramírez León is shareholder & President of Board of Directors Ortomac, Colombia, consultant Elliquence, USA. Drs. CR Martínez, N Prada and JG Rugeles Ortíz are consultants for Elliquence, USA. Dr. G Choi is consultant for Maxmore and Elliquence. The senior author designed and trademarked his inside-out YESS™ technique and receives royalties from the sale of his inventions. Indirect conflicts of interest (honoraria, consultancies to sponsoring organizations are donated to IITS.org, a 501c 3 organization). The other authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
References
- Park Y, Seok SO, Lee SB, et al. Minimally Invasive Lumbar Spinal Fusion Is More Effective Than Open Fusion: A Meta-Analysis. Yonsei Med J 2018;59:524-38. [Crossref] [PubMed]
- Mancuso CA, Duculan R, Cammisa FP, et al. Fulfillment of patients' expectations of lumbar and cervical spine surgery. Spine J 2016;16:1167-74. [Crossref] [PubMed]
- Mancuso CA, Duculan R, Cammisa FP, et al. Proportion of Expectations Fulfilled: A New Method to Report Patient-centered Outcomes of Spine Surgery. Spine (Phila Pa 1976) 2016;41:963-70. [Crossref] [PubMed]
- Tabibian BE, Kuhn EN, Davis MC, et al. Patient Expectations and Preferences in the Spinal Surgery Clinic. World Neurosurg 2017;106:595-601. [Crossref] [PubMed]
- Stambough JL. Matching patient and physician expectations in spine surgery leads to improved outcomes. Spine J 2001;1:234. [Crossref] [PubMed]
- Mehrotra A, Sloss EM, Hussey PS, et al. Evaluation of a center of excellence program for spine surgery. Med Care 2013;51:748-57. [Crossref] [PubMed]
- McClelland S 3rd, Goldstein JA. Minimally Invasive versus Open Spine Surgery: What Does the Best Evidence Tell Us? J Neurosci Rural Pract 2017;8:194-8. [Crossref] [PubMed]
- Goldstein CL, Macwan K, Sundararajan K, et al. Perioperative outcomes and adverse events of minimally invasive versus open posterior lumbar fusion: meta-analysis and systematic review. J Neurosurg Spine 2016;24:416-27. [Crossref] [PubMed]
- Bookwalter JW 3rd, Busch MD, Nicely D. Ambulatory surgery is safe and effective in radicular disc disease. Spine (Phila Pa 1976) 1994;19:526-30. [Crossref] [PubMed]
- Fokter SK, Yerby SA. Patient-based outcomes for the operative treatment of degenerative lumbar spinal stenosis. Eur Spine J 2006;15:1661-9. [Crossref] [PubMed]
- Yeung AT. Lessons Learned from 27 Years’ Experience and Focus Operating on Symptomatic Conditions of the Spine under Local Anesthesia: The Role and Future of Endoscopic Spine Surgery as a “Disruptive Technique” for Evidenced Based Medicine. J Spine 2018;7:413. [Crossref]
- Asch HL, Lewis PJ, Moreland DB, et al. Prospective multiple outcomes study of outpatient lumbar microdiscectomy: should 75 to 80% success rates be the norm? J Neurosurg 2002;96:34-44. [PubMed]
- Hersht M, Massicotte EM, Bernstein M. Patient satisfaction with outpatient lumbar microsurgical discectomy: a qualitative study. Can J Surg 2007;50:445-9. [PubMed]
- Pendharkar AV, Shahin MN, Ho AL, et al. Outpatient spine surgery: defining the outcomes, value, and barriers to implementation. Neurosurg Focus 2018;44:E11. [Crossref] [PubMed]
- Su AW, Habermann EB, Thomsen KM, et al. Risk Factors for 30-Day Unplanned Readmission and Major Perioperative Complications After Spine Fusion Surgery in Adults: A Review of the National Surgical Quality Improvement Program Database. Spine (Phila Pa 1976) 2016;41:1523-34. [Crossref] [PubMed]
- Kim BD, Smith TR, Lim S, et al. Predictors of unplanned readmission in patients undergoing lumbar decompression: multi-institutional analysis of 7016 patients. J Neurosurg Spine 2014;20:606-16. [Crossref] [PubMed]
- Modhia U, Takemoto S, Braid-Forbes MJ, et al. Readmission rates after decompression surgery in patients with lumbar spinal stenosis among Medicare beneficiaries. Spine (Phila Pa 1976) 2013;38:591-6. [Crossref] [PubMed]
- Kocher KE, Nallamothu BK, Birkmeyer JD, et al. Emergency department visits after surgery are common for Medicare patients, suggesting opportunities to improve care. Health Aff (Millwood) 2013;32:1600-7. [Crossref] [PubMed]
- Zolot J. A Worsening Opioid Epidemic Prompts Action. Am J Nurs 2017;117:15. [PubMed]
- Cheatle MD. Facing the challenge of pain management and opioid misuse, abuse and opioid-related fatalities. Expert Rev Clin Pharmacol 2016;9:751-4. [Crossref] [PubMed]
- Hupp JR. The Surgeon’s Roles in Stemming the Prescription Opioid Abuse Epidemic. J Oral Maxillofac Surg 2016;74:1291-3. [Crossref] [PubMed]
- Kee JR, Smith RG, Barnes CL. Recognizing and Reducing the Risk of Opioid Misuse in Orthopaedic Practice. J Surg Orthop Adv 2016;25:238-43. [PubMed]
- What Low Response Rates Mean for Telephone Surveys. Available online: http://www.pewresearch.org/2017/05/15/what-low-response-rates-mean-for-telephone-surveys/
- The Complete Guide to Acceptable Survey Response Rates. Available online: https://www.genroe.com/blog/acceptable-survey-response-rate/
- What is an acceptable survey response rate? Available online: http://socialnorms.org/what-is-an-acceptable-survey-response-rate/
- Mobile Survey Response Rates: Averages and Benchmarks by App Category. Available online: http://www.apptentive.com/blog/2016/10/04/mobile-survey-response-rates/
- 12 Mind-blowing Employee Survey Statistics. Available online: http://www.officevibe.com/blog/employee-surveys-infographic
- Improving Response to Web and Mixed-Mode Surveys. Available online: https://www.academic.oup.com/poq/article/75/2/249/1860211
- 7 Secret Ways to Increase Your Survey Response Rate. Available online: https://www.promoter.io/blog/increase-survey-responses
- Todd AL, Porter M, Williamson JL, et al. Pre-notification letter type and response rate to a postal survey among women who have recently given birth. BMC Med Res Methodol 2015;15:104. [Crossref] [PubMed]
- Odgaard L, Kothari M. Survey of oral nursing care attitudes, knowledge and practices in a neurorehabilitation setting. J Oral Rehabil 2019;46:730-7. [PubMed]
- Dombrecht L, Deliens L, Chambaere K, et al. Neonatologists and neonatal nurses have positive attitudes towards perinatal end-of-life decisions, a nationwide survey. Acta Paediatr 2019. [Epub ahead of print]. [Crossref] [PubMed]
- Brandt NJ, Cooke CE, Sharma K, et al. Findings from a National Survey of Medicare Beneficiary Perspectives on the Medicare Part D Medication Therapy Management Standardized Format. J Manag Care Spec Pharm 2019;25:366-91. [Crossref] [PubMed]
- Weber C, Lønne G, Rao V, et al. Surgical management of lumbar spinal stenosis: a survey among Norwegian spine surgeons. Acta Neurochir (Wien) 2017;159:191-7. [Crossref] [PubMed]
- Anand N, Agrawal A, Burger EL, et al. The Prevalence of the Use of MIS Techniques in the Treatment of Adult Spinal Deformity (ASD) Amongst Members of the Scoliosis Research Society (SRS) in 2016. Spine Deform 2019;7:319-24. [Crossref] [PubMed]
- Joeris A, Knoll C, Kalampoki V, et al. Patient-reported outcome measurements in clinical routine of trauma, spine and craniomaxillofacial surgeons: between expectations and reality: a survey among 1212 surgeons. BMJ Open 2018;8:e020629. [Crossref] [PubMed]
- Wang J, Alotaibi NM, Ibrahim GM, et al. The Spectrum of Altmetrics in Neurosurgery: The Top 100 "Trending" Articles in Neurosurgical Journals. World Neurosurg 2017;103:883-895.e1. [Crossref] [PubMed]
- Haldeman S, Johnson CD, Chou R, et al. The Global Spine Care Initiative: care pathway for people with spine-related concerns. Eur Spine J 2018;27:901-14. [Crossref] [PubMed]
- Haldeman S, Nordin M, Chou R, et al. The Global Spine Care Initiative: World Spine Care executive summary on reducing spine-related disability in low- and middle-income communities. Eur Spine J 2018;27:776-85. [Crossref] [PubMed]
- Johnson CD, Haldeman S, Nordin M, et al. The Global Spine Care Initiative: methodology, contributors, and disclosures. Eur Spine J 2018;27:786-95. [Crossref] [PubMed]


