
Clinical outcomes with endoscopic resection of lumbar extradural cysts
Introduction
Intraspinal but extradural cysts may be associated with sciatica-type back and leg pain. In comparison to a herniated disc and foraminal or lateral recess stenosis, such intraspinal yet extradural cysts are a relatively uncommon cause of lumbar radiculopathy due to direct compression of spinal nerve roots (1-3). The symptoms of clinical pain syndrome are impossible to differentiate from those of lumbar disc herniation or spinal canal stenosis. However, low back pain and neurogenic claudication symptoms may precede the onset of radicular leg (4-9). The diagnosis of a painful intraspinal cyst is based on history and physical examination and corroborating advanced magnetic resonance imaging (MRI) whose sensitivity has been reported as high as 90% compared to 70% of computed tomography (CT) scan (10-13).
Several types of intraspinal cysts may be encountered during the workup of a symptomatic patient. Typical findings include extradural arachnoid cysts (14,15), perineural (Tarlov) cysts (16,17), dermoid cysts (18,19), neurofibroma with cystic degeneration (20), and synovial or ganglion cysts (13). The latter types of cysts are the most commonly detected cystic structures in the lumbar spine and typically arise from the zygapophysial joints (Z-joints)—the facet joints. These are histologically distinct synovial cysts or ganglion cysts whose presence on advanced imaging studies has been associated with instability (Table 1). Therefore, facet cysts are most commonly found at the single-most mobile segment—L4/5 (13,21,22). The clinical presentation can be acute with sudden onset of severe pain at first. Many patients take an acute-on-chronic course with multiple acute flare-ups before seeking medical attention. The overall clinical course is benign with a self-limiting natural history, which ultimately aids in the establishment of the diagnosis. Juxtafacet cysts are quite uncommon causes of radiculopathy, low back pain, and neurogenic claudication and are often associated with advanced spinal degenerative disease.
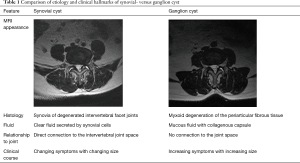
Full table
The nonoperative treatment of these synovial facet joint cysts hinges on medical management with the judicious use of nonsteroidal anti-inflammatories (NSAIDs), and transforaminal epidural steroid injections (TESI). Narcotic pain killers are typically not advised but may be necessary for a short period of times, particularly in patients who have already been on opioids for pain syndromes of the lower back. Activity modification, with a light walking schedule, and physical therapy (PT) with emphasis on core-strengthening exercises, should be recommended. The inability of the patient to improve with these supportive care strategies or to actively participate in an exercise-based program, whether PT or a self-directed program, should raise red flag alerts and prompt the search for other confounding factors. Considering that the synovial cysts could be an incidental finding, other potential pain generators due to instability- or stenosis related neural element compression, infectious, undiagnosed inflammatory (rheumatoid arthritis, ankylosing spondylitis, or gout) or a tumorous process should be carefully considered in the differential diagnosis. Some authors advocate an interventional CT-guided needle aspiration and intra-articular injection as adjunctive therapy (23,24). However, successful treatment can be hit, or miss and even an image-confirmed placement of the needle and aspiration of the facet cyst content have not been shown to either definitively treat the disease, nor to diminish symptoms reliably (24). Instant pain relief is often from the injection of a local anesthetic during the procedure. Whether long-term pain relief can be attributed the intra-articular aspiration remains debatable since the overall clinical course is benign and symptoms may improve because as a result of the natural history of the disease playing out (23). Because of these less reliable outcomes with non-operative treatments, the authors of this study assessed clinical outcomes with endoscopic resection of extradural facet joint cysts in patients as a way to manage the lumbar degenerative disease affecting the facet joint in a staged manner before considering more aggressive translaminar treatments including laminectomy or fusion.
Methods
Study patients
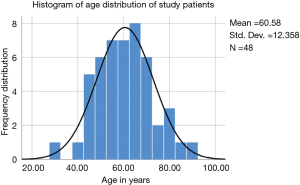
Patients suffering from unrelenting lumbar radiculopathy non-responsive to conservative care underwent outpatient endoscopic spinal surgery for the treatment facet-based cysts found serendipitously on routine lumbar MRI scans ordered for suspected herniated disc or spinal stenosis. In this study, there were 48 patients, 26 of whom were female, and 22 were male patients. The average age was 60.58 years ranging from 30 to 91 years (Figure 1). All patients were operated between 2008 and 2014 by both surgeons at their practice setting. Patients were selected from an extensive case log database maintained by both authors. Patients were only included in this study if 2-year follow-up data without gaps were available. Patients with radiculopathy unresponsive to a minimum of 12 weeks of conservative care, and MRI scans showing foraminal or lateral recess stenosis with a facet cyst were included in this study. Patients were also evaluated for evidence of facet hypertrophy on and whether or not there was MRI evidence of subclinical instability in the facet joint as recently suggested by the presence of a thickened ligamentum flavum, a widened joint space of greater than 2 mm filled with white fluid on T2-weighted image sequences (25,26). Patients with metastatic disease, infection; and more than grade I spondylolisthesis were excluded. Preoperative lateral projection dynamic extension/flexion views were also evaluated for each patient to see whether there was any discernable motion on these images or whether the degenerative spondylolisthesis was rigid.
Surgical management
Surgical treatment is reasonable when all non-operative treatment measures fail, or when patients present with rapid onset of severe neurological deficit that is associated with severe pain (3,8,27,28). Several open or minimally invasive surgical excision techniques have been described. The procedure of choice may be dictated by the size and localization of the synovial facet cyst and its relationship to the neural elements. The preferred treatment chosen by the authors was the endoscopic removal of synovial cysts. Since they are often acutely inflammatory, painful and may present with multi-loculated cystic architecture, these cysts can repeatedly fill and leak onto the neural element; particularly if there is an underlying inflammatory disease process. Hence, chronic epidural fibrosis may be found at the time of surgery, potentially making the endoscopic dissection more difficult and increasing the risk for nerve root injuries or incidental durotomies. These are typically encountered in the axilla between the exiting and traversing nerve root as many cysts emanate at the tip of the superior articular process (SAP) and are close to the dorsal root ganglion (DRG). The endoscopic resection of the cyst often requires dissection in the hidden zone of Macnab. Hence, postoperative dysesthesias and motor dysfunction may occur—many of which resolve spontaneously with supportive care measures, TESI, and medical management using gabapentin or pregabalin. The authors used the following two surgical techniques.
Transforaminal approach
The patient is positioned prone and prepped and draped in standard surgical fashion. Anatomic landmarks, including the midline, iliac crest, and a line parallel to the disc space can be drawn on the patient to facilitate placement of the skin incision for the transforaminal approach. The interpedicular line may be drawn on the symptomatic side as well to measure the lateral distance of the skin incision from the lateral recess to be accessed. The subsequent surgical procedure is performed under posteroanterior (PA) and lateral fluoroscopic guidance. The C-Arm should be lined up to the patient in a way as to avoid parallax and unnecessary radiation of the patient, surgeon, and the OR staff. The endplates should line up parallel. The entry point for the skin incision is determined individually by measuring the attack angles and distances on the PA and lateral fluoroscopic views taking any anatomical variations and structures obstructing access to the surgical neuroforamen, the extent of pathology and its location into consideration.
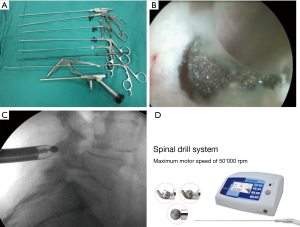
The authors prefer the surgery under monitored anesthesia care (MAC) and apply local anesthesia at the determined entry point as well as the entire surgical corridor before a small skin incision is made. Care should be taken to avoid injection of a local anesthetic into the exiting nerve root to prevent injury while maintaining excellent communication with the patient. A 16 or 18 G needle is advanced toward the target area followed by dilators which are carefully introduced over a guide wire towards the foramen in a clockwise rotation. After serial dilation, the working sleeve is introduced and positioned strategically to retract the exiting nerve root. Now, the endoscope is introduced, allowing direct visualization during the foraminoplasty with the power- shaves or burs. Additional instruments, including Kerrison rongeurs, punches, and hooks may prove useful during the lateral recess decompression. A bipolar or a radiofrequency probe may be handy during dissection of any soft tissue of the bone and to control bleeding (Figure 2). The working cannula can now be introduced into the intervertebral disc (inside-out technique), or into the lateral recess above the posterior annulus (outside-in technique). The choice of transforaminal decompression technique may depend on the size and location of the facet cyst, or any associated herniated discs as well as surgeon’s preference. Both methods allow good visualization of the axillary hidden zone of Macnab. Typically, the inside-out approach involves some resection of the posterior annulus or creation of an annular window which allows direct visual inspection of the anterior aspect of the dural sac. Utilization of inside-out techniques may prove useful in the setting of excessive epidural fibrosis and difficult to dissection adhesions wherein the interest of avoiding dural tears it may be safer to perform a posterior annular resection and leaving some scar tissue on the neural elements rather than trying to dissect the interval between dura and cyst at all cost. This approach was performed in 79.2% (38/48) of the study patients. A case example is shown in Figure 3.

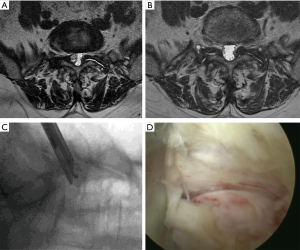
Interlaminar approach
The interlaminar approach has recently gained popularity for accessing pathologies located at the L5–S1 level (Figure 4). It was chosen in 10 (20.8%) of the 48 patients in this series. Nine of these 10 patients underwent surgery by the first author at L5/S1. This miniaturized posterior muscle splitting approach also diminishes the collateral damage significantly, but the working area is limited to the interlaminar window allowing resection of the yellow ligament and decompression of the central spinal canal and lateral recess. Essential for the resection of a juxtafacet cyst is the proper bony decompression of the inferior articular process (IAP). Synovial cyst extending into the lateral recess often requires partial resection of the IAP to complete the decompression and to provide for full visualization of the cyst and to facilitate its dissection from the neural structures. If the interlaminar window is smaller or absent at the upper lumbar levels, extensive removal of the lamina and the lateral facet joint may be necessary. A high-speed burr may prove indispensable (Figure 2).
For surgery, the patient is positioned (prone) and prepped similarly as if surgery using the transforaminal approach was intended. Anatomic landmarks, such as the midline, the interlaminar window, the intervertebral disc space, and the facet joints are marked on intraoperative PA and lateral views. Once the attack angles and the entry points are established considering the location, size, and relationship to other anatomical structures, all the subsequent procedures are performed under lateral fluoroscopic guidance maintaining parallel endplates and most importantly under direct and continuous video endoscopic visualization. The working cannula is inserted over sequential dilators positioning it at the medial aspect of the facet joint at its junction with the lamina. The beveled side of the working cannula should be turned towards the ligament flavum, and the inferior lateral edge of the lamina may be exposed with rongeurs, a radiofrequency probe, and burs as needed. As the decompression proceeds with removal of the inferomedial portion of the facet joint, the working cannula can be advanced into the lateral recess to expose the synovial cyst. The choice of the preferred burr may vary and should be at the surgeon’s discretion. For example, the first author (SH) prefers the use of a diamond burr, whereas the senior author (KUL) prefers a slow speed high-torque round drill bit. At times, the ligamentum flavum has to be opened with a blunt dissector and subsequently removed with the use of an endoscopic Kerrison rongeur. After exposure of the cyst, adhesion with dura and nerve root should be separated with the dissector. The bevel cannula should be turned over the cyst to protect the neural structures retracting either the traversing or exiting nerve with the bevel. Now, the cyst can be removed with different graspers and punches. While a rapid direct posterior piecemeal resection of the cyst may be more comfortable with the interlaminar than with the transforaminal approach, the hidden zone of Macnab in the axilla of the two nerve roots is less well visualized mainly if there are adhesions. Therefore, care must be taken that the neural element decompression is complete and that multiloculated cyst tissue is not entrapped or hidden by or under epidural adhesions. If a large portion of the medial facet joint has to be resected to expose the cyst and gain access to the symptomatic lateral recess, the surgeon should consider a simultaneous transforaminal, hence full endoscopic, decompression during the same index procedure. This may facilitate visualization of the axillary hidden zone of Macnab and aid in minimizing the extent of medial facet resection to avoid iatrogenic propagation of postoperative instability. At the end of the case, the cannula will be turned to visualize the neural structures and to control the decompression by a palpation hook.
Statistical and outcome analysis
Primary clinical outcomes measures for patients who underwent endoscopic facet cyst resection were the Macnab criteria at final follow-up two years postoperatively (27). Statistical tests employed in the outcome analysis of this study included two-way cross-tabulation statistics to measure any statistically significant association between variables using IBM SPSS Statistics software, Version 25.0. Pearson Chi-Square and Fisher’s Exact test were employed to assess the strength of association between variables statistically. The mean, range, and standard deviation (STD), and percentages of all nominal variables were calculated.
Results
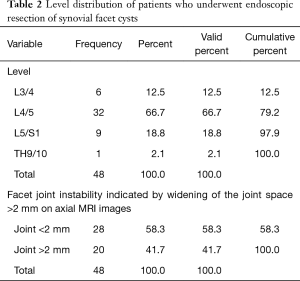
The age histogram of our study patients with a superimposed expected standard distribution curve was plotted and is shown in Figure 1. The average age was 60.58 years (STD 12.358 years) with the youngest patient being 30 years of age and the oldest patient 91 years, respectively. The mean follow-up was 55.46 months, ranging from 24 to 129 months. The endoscopic facet cyst resection was most commonly performed at the L4/5 level in 26 patients (72.2%) followed by the L5/S1 level in 8 patients (22.2%). An additional two patients (5.6%) underwent endoscopic facet cyst resection at the L3/4 level. One patient had surgery at the T9/10 level (2.1%; Table 2). The transforaminal approach was chosen in 38 (79.2%) of the 48 study patients. The interlaminar approach was applied by the first author (SH) in the remaining 10 (20.8%) patients nine of which had surgery at the L5/S1 level. The intraoperative blood loss was minimal in all patients. Most patients had an uneventful postoperative recovery with only 6 patients (12.5%) reporting postoperative dysesthesias due to irritation of the DRG. One patient had a recurrent disc herniation (2.1%), and another patient did not improve due to unrecognized underlying chronic neuropathy. Two patients (4.2%) underwent reoperation with transforaminal interbody fusion (TLIF)—one for recurrent herniation and the other natural progression of the underlying degenerative process. There were no statistically significant differences in any of the variables tested between the surgeons including level- and patients’ age distribution, outcome measures, reoperation or dysesthesia rates (P>0.2 for lowest P value). Preoperative axial MRI scanning indicated instability of the operative motion segment by widening of the facet joint space to greater than 2 mm in 20 (41.7%) of the 48 study patients (Table 2).
Full table
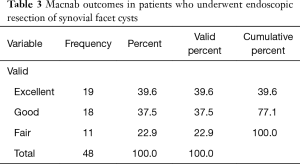
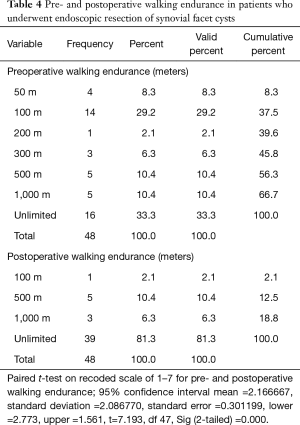
Two years postoperatively, 39.6% (19/48) of patients reported Excellent, and another 37.5% (18/48) Good Macnab outcomes. Hence, 77.1% of all patients had Excellent and Good clinical outcomes, according to Macnab 2 years postoperatively. However, approximately one-quarter of the patients (11/48; 22.9%) reported Fair Macnab outcomes (Table 3). The average preoperative VAS score for leg pain was 8.06±1.57 and reduced at a statistically significant level (P<0.000) postoperatively to 1.92±1.49, and 1.77±1.32 at final follow-up, respectively. At final follow-up, the average VAS reduction was 6.29±1.9. Patients’ walking endurance improved significantly as well as a result of the endoscopic decompression procedure. Only 16 of the 48 (33.3%) study patients had unlimited walking endurance preoperatively. Most patients reported the walking endurance to the pain limit as 100 meters (14/48; 29.2%). Another 13 (27.03%) patients, indicated that they are only able to walk less than 500 meters before having to stop (Table 4). At final follow, walking endurance had improved at a statistically significant level (P<000) from 33% preoperatively (16/48) to 81.3% (39/48) of the study patients (Table 4). Only one patient did not improve and reported a walking endurance to 100 meters postoperatively. This patient was diagnosed with a chronic neuropathy, which ultimately was unamenable to surgical treatment. The remaining eight patients improved their walking endurance to from less than 100 meters preoperatively to 500 and 1,000 meters postoperatively (Table 4).
Full table
Full table
All patients regardless of outcome reported resolution of radicular leg pain and claudication symptoms postoperatively. All patients with good (18/48) and fair (11/48) outcomes complained of residual mechanical low back pain. During the 2-year follow-up period, each of these 29 patients was successfully treated with non-operative supportive care measures, including NSAIDS, activity modification, and PT. There was no statistically significant correlation between clinical Macnab outcomes and the patients’ primary surgeon, gender, age, or the level of surgery. There were no study patients with notable complications related to approach, surgery or anesthesia. There were no nerve root injuries or postoperative weakness. The choice of transforaminal or interlaminar approach also did not bear out in any statistically significant differences in the variables tested. No other complications were observed in the immediate 90-day postoperative period or after that during the available follow-up period.
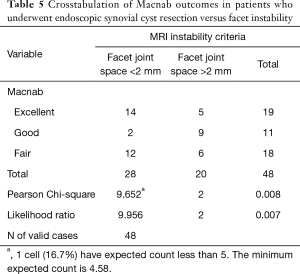
MRI findings of mechanical incompetency and subclinical instability of the motion segment (MRI instability markers) such as thickened ligamentum flavum and widening of the facet joint complex on axial T2-weighted images (Figure 2A) measured to be greater than 2 mm across the joint space were noted in 20 (41.7%) of the 48 patients. The majority of these patients (14/20) had fixed grade I spondylolisthesis on preoperative dynamic extension/flexion views without any discernable motion. The other two patients with grade I spondylolisthesis only showed less than 3 mm of anterolisthesis in flexion with a reduction in extension on preoperative dynamic lateral views. Crosstabulation of the primary clinical outcome measures versus MRI instability markers showed a statistically significant correlation between Fair clinical Macnab outcomes and positive MRI instability markers (P<0.001; Table 5).
Full table
Discussion
The study demonstrated the feasibility of staged management of synovial facet cysts with endoscopic surgery as an alternative to other forms of traditional or minimally invasive (MIS) translaminar surgery. It was motivated at least in part to address some of the concerns with open spine surgery with its well-documented risk of postlaminectomy-syndrome and instability. The principal advantages of the various endoscopic transforaminal, interlaminar, or full endoscopic approaches lie in the minimal bony resection of the facet joint complex during the initial foraminoplasty to gain access to the facet cyst in the foramen and lateral recess. Central canal involvement is less common but may be present in patients with very large cysts, thus, prompting interlaminar or over-the-top techniques to perform an adequate decompression could theoretically be necessary but was not a common problem in this series of 36 patients. Additional advantages of the endoscopic lumbar decompression techniques—initially developed for discectomy—are associated with a much lower burden to the patient from approach-related iatrogenic soft-tissue injuries, significantly reduced intraoperative blood loss, and postoperative pain and nausea. Many of these endoscopic spinal surgeries are carried out in an ambulatory surgery center (ASC) under MAC with light sedation, without formal intubation and with or without prone laryngeal mask anesthesia (LMA). Typically, patients are sent home within one hour, and readmission to a hospital for unintended aftercare is very uncommon (29).
The etiology of intraspinal cysts is not clearly understood, and several explanations have been discussed. These include osteoarthritis, degenerative spondylolisthesis, mechanical irritation of the facet joint due to hypermobility, chronical or direct trauma, and leaking synovial liquid followed by slime degeneration of the surrounding connective tissue. Iatrogenic causes may also exist (30). A surge of intraspinal facet cysts has been reported with a peak incidence in up to 8.6% of patients within 3 to 12 months following routine microsurgical decompression surgery for lumbar spinal stenosis (31). Typically, spontaneous regression is observed in up to 70% of cases within 6–36 months. Half of the reported instances have been asymptomatic (31,32). However, post-laminectomy segmental and rotational instability has been reported to be associated with postoperative appearance of intraspinal facet cysts at a statistically significant level particularly if there is progression of spondylolisthesis and disc degeneration (33). Other possible reported explanations for the development of intraspinal cysts include myxoid degeneration and softening of collagen connecting tissue of the joint capsule, metaplasia of pluripotent mesenchymal cells, embryonal synovial tissue in the periarticular fibrous connective tissue growing through constant stimulus, the proliferation of fibroblasts with increasing hyaluronic acid production due to irritation, and benign neoplastic origin. Regardless of the specific etiology, a synovial cyst can easily be misdiagnosed when low back- and radicular pain persists. Often distinction of a synovial and from a ganglion cyst based on routine lumbar MRI scan is not possible. History and physical examination rarely help in the differential diagnosis since the clinical symptoms are the same. Sometimes ganglion cysts can be found even inside synovial cysts, and bleeding into the cysts makes a definitive histological classification of the cyst content occasionally impossible. For these reasons, the exact histopathological definition of the juxtafacet cyst seems irrelevant since the clinical presentation and therapies are similar.
In 2002, Shima et al. proposed to categorize both synovial and ganglion cysts as degenerative intraspinal cysts (34). Other authors proposed the term periarticular cyst, joint cysts, synovial cysts, or as mentioned juxta facet cysts (11). Kao proposed the term “juxta-facet cyst” which was derived from lat. iuxta = “close by” in 1974 (35). He used this term to describe both synovial and ganglion cysts (35). To date, there is no uniform nomenclature. A synovial cyst can only be histologically distinguished from a ganglion cyst. Histologically, the outer synovial cell layer often consists of a soft synovial epithelial cell layer and is in direct contact with the adjacent capsule. The origin of most juxtafacet cysts is the Synovium. The cyst tends to be filled with a clear, serous or xanthochrome liquid, containing substantial mucopolysaccharides (35). The vast majority of patients presenting synovial cysts are likely to be asymptomatic (36-38). Typically ganglion cysts show a loose connective tissue coating and are filled with a more protein enriched viscous liquid as well origin tissue. Ganglion cysts are the result of mucoid degeneration of periarticular connective tissue. Additional variable terminologies found in the literature besides synovial cysts (10,26,33,39), include ganglion cysts (36), pseudocysts (38), lumbar intraspinal facet cysts or fibrous cysts (40), and cystic formations of the mobile spine (41). Moreover, atypical cysts have been observed and reported as “ectopic” synovial tissue (42,43). In an asymptomatic population of 852 patients undergoing positional MRI, Niggemann et al. diagnosed 50 patients with intraspinal juxtafacet cysts (=5.87%) (41). The clinical presentation of many joint cysts is such that symptoms may develop within a short period. Most of them are found in the hand, elbow, hip, and knee. They are rarely found in the lumbar spine and are even less common in the thoracic and cervical regions (21). In comparison to joint based cysts, the pathogenesis of discal cysts is not well understood. Synovial and ganglion cysts are often also described as pseudotumors, and often are associated with degenerative spondylolisthesis where hypermobility or overt instability of the degenerated lumbar spinal motion segment and its facet joints is believed to be the underlying cause.
Treatment of de novo synovial cyst within the spine without severe compression of the neural structures usually consists of conservative treatment. Many patients respond well to epidural corticosteroid injections with short-term relief (24,25). Additional non-operative treatment include short-term bed rest, bracing, PT, selective nerve root blocks, medical management with NSAIDs or short term treatment with opioids. Interventional treatment with a CT-guided needle aspiration is reserved for non-responsive patients. Surgical removal either by microsurgical hemilaminectomy, or endoscopic excision can be considered in patients refractory to conservative care. It often produces very satisfactory clinical results (5). In surgery, a simple puncture or squeezing of the cysts should be avoided. It is associated with minimal or short-term pain relief and a higher recurrence rate (5). During the endoscopic decompression the traversing nerve root should be identified before the cyst is carefully separated from the dural sac. It may be resected either en-bloc or by piecemeal using endoscopic graspers and other dissection devices after release of any liquid or mucoid content. Sometimes there is neovascularization or cellular infiltration, similar to those seen with herniated discs (44). The decompression should always be performed under direct visualization, and the stalk of the cyst should be sealed using bipolar RF. To date, there are no universally accepted treatment guidelines.
The goal of surgical treatment should be a full excision of the cyst either by endoscopic means or microsurgical dissection (37,38). The authors chose the transforaminal or interlaminar endoscopic surgery to excise any synovial cysts to minimize trauma and scarring of the posterior spinal structures with the intent of lowering the risk of postoperative segmental instability requiring spinal fusion. The endoscopic technique for cyst removal is a relatively new option (45). It is not an overly complicated technique but requires some fineness with attention to some surgical pearls. The skilled endoscopic spine surgeon should be able to replace traditional microsurgical hemilaminectomy decompression and resection of any juxta-synovial facet cyst with the endoscopic technique. As shown by the results of this study, all patients improved with complete resolution of the radiculopathy symptoms. Excellent and good Macnab outcomes were obtained in 77.1% of patients; even in the one patient with an uncommon T9/10 facet cyst. Macnab outcome measures were corroborated by statistically significant postoperative VAS score reductions averaging 6.29±1.9. Walking also improved to unlimited endurance in 81.2% of patients following their endoscopic decompression procedure. Good and fair outcomes were rated that way because of persistence of mechanical back pain. Statistical analysis showed a significant correlation between advanced degeneration of the facet joint and instability of the motion segment as evidenced by the MRI instability markers including thickening of the ligamentum flavum and greater than 2-mm widening of the facet joint space. These MRI instability markers may be useful as prognosticators of clinical outcomes. Future studies could investigate whether or not these MRI-findings are associated with better long-term outcomes with decompression or a reconstructive fusion procedure that involves resection of the affected facet joints.
Conclusions
In the hands of a skilled surgeon, endoscopic removal of facet cysts is a viable alternative to microsurgery. It minimizes collateral damage from aggressive tissue dissection and is expected to be associated with lower postoperative instability rates. An effective decompression can be done under direct endoscopic visualization. Endoscopic resection of any facet cyst should be considered before any translaminar open or MIS laminectomy and as an alternative to a joint-resection based spinal fusion. It is a classic application of a staged disease management strategy without the treatment contributing to disease acceleration.
Acknowledgments
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. The study was approved by IRB (CEIFUS 106-19) and written informed consent was obtained from all patients.
References
- Yeung A, Yeung CA. Endoscopic Identification and Treating the Pain Generators in the Lumbar Spine that Escape Detection by Traditional Imaging Studies. J Spine 2017;6:369.
- Kouyialis AT, Boviatsis EJ, Korfias S, et al. Lumbar synovial cyst as a cause of low back pain and acute radiculopathy: a case report. South Med J 2005;98:223-5. [Crossref] [PubMed]
- Reddy P, Satyanarayana S, Nanda A. Synovial cyst of lumbar spine presenting as disc disease: a case report and review of literature. J La State Med Soc 2000;152:563-66. [PubMed]
- Howington JU, Connolly ES, Voorhies RM. Intraspinal synovial cysts: 10-year experience at the Ochsner Clinic. J Neurosurg 1999;91:193-9. [PubMed]
- Kono K, Nakamura H, Inoue Y, et al. Intraspinal extradural Cysts communicating with adjacent herniated disks: imaging characteristics and possible pathogenesis. AJNR 1999;20:1373-7. [PubMed]
- Trummer M, Flaschka G, Tillich M, et al. Diagnosis and surgical management of intraspinal synovial cysts: report of 19 cases. J Neurol Neurosurg Psychiatry 2001;70:74-7. [Crossref] [PubMed]
- Kurz LT, Garfin SR, Unger AS, et al. Intraspinal synovial cyst causing sciatica. J Bone Joint Surg Am 1985;67:865-71. [Crossref] [PubMed]
- Baum JA, Hanley EN. Intraspinal synovial cyst simulating spinal stenosis. A case report. Spine 1986;11:487-9. [Crossref] [PubMed]
- Banning CS, Thorell WE, Leibrock LG. Patient outcome after resection of lumbar juxtafacet cysts. Spine 2001;26:969-72. [Crossref] [PubMed]
- Hemminghytt S, Daniels DL, Williams AL, et al. Intraspinal synovial cysts: natural history and diagnosis by CT. Radiology 1982;145:375-6. [Crossref] [PubMed]
- Kao CC, Uihlein A, Bickel WH, et al. Lumbar intraspinal extradural ganglion cyst. J Neurosurg 1968;29:168-72. [Crossref] [PubMed]
- Jackson DE, Atlas SW, Mani JR, et al. Intraspinal synovial cysts: MR imaging. Radiology 1989;170:527-30. [Crossref] [PubMed]
- Boviatsis EJ, Stavrinou LC, Kouyialis AT, et al. Spinal synovial cysts: pathogenesis, diagnosis and surgical treatment in a series of seven cases and literature review. Eur Spine J 2008;17:831-7. [Crossref] [PubMed]
- Liu JK, Cole CD, Kan P, et al. Spinal extradural arachnoid cysts: clinical, radiological, and surgical features. Neurosurg Focus 2007;22:E6. [Crossref] [PubMed]
- Choi JY, Kim SH, Lee WS, et al. Spinal extradural arachnoid cyst. Acta Neurochir (Wien) 2006;148:579-85; discussion 585. [Crossref] [PubMed]
- Voyadzis JM, Bhargava P, Henderson FC. Tarlov cysts: a study of 10 cases with review of the literature. J Neurosurg 2001;95:25-32. [PubMed]
- Mitra R, Kirpalani D, Wedemeyer M. Conservative management of perineural cysts. Spine 2008;33:E565-8. [Crossref] [PubMed]
- Kanev PM, Park TS. Dermoids and dermal sinus tracts of the spine. Neurosurg Clin N Am 1995;6:359-66. [Crossref] [PubMed]
- Baker JK, Hanson GW. Cyst of the ligamentum flavum. Spine 1994;19:1092-4. [Crossref] [PubMed]
- Métellus P, Fuentes S, Dufour H, et al. An unusual presentation of a lumbar synovial cyst: case report. Spine 2002;27:E278-80. [Crossref] [PubMed]
- Shah RV, Lutz GE. Lumbar intraspinal synovial cysts: conservative management and review of the world's literature. Spine J 2003;3:479-88. [Crossref] [PubMed]
- Sabo RA, Tracy PT, Weinger JM. A series of 60 juxtafacet cysts: clinical presentation, the role of spinal instability, and treatment. J Neurosurg 1996;85:560-5. [Crossref] [PubMed]
- Sabers SR, Ross SR, Grogg BE, et al. Procedure-based nonsurgical management of lumbar zygapophyseal joint cyst-induced radicular pain. Arch Phys Med Rehabil 2005;86:1767-71. [Crossref] [PubMed]
- Bjorkengren AG, Kurz LT, Resnick D, et al. Symptomatic intraspinal synovial cysts: opacification and treatment by percutaneous injection. AJR Am J Roentgenol 1987;149:105-7. [Crossref] [PubMed]
- Snoddy MC, Sielatycki JA, Sivaganesan A, et al. Can facet joint fluid on MRI and dynamic instability be a predictor of improvement in back pain following lumbar fusion for degenerative spondylolisthesis? Eur Spine J 2016;25:2408-15. [Crossref] [PubMed]
- Cho IY, Park SY, Park JH, et al. MRI findings of lumbar spine instability in degenerative spondylolisthesis. J Orthop Surg (Hong Kong) 2017;25:2309499017718907. [Crossref] [PubMed]
- Lyons MK, Atkinson JL, Wharen RE, et al. Surgical evaluation and management of lumbar synovial cysts: the Mayo Clinic experience. J Neurosurg 2000;93:53-7. [PubMed]
- Macnab I. Negative disc exploration: An analysis of the causes of nerve-root involvement in sixty-eight patients. J Bone Joint Surg Am 1971;53:891-903. [Crossref] [PubMed]
- Lewandrowski KU. Readmissions After Outpatient Transforaminal Decompression for Lumbar Foraminal and Lateral Recess Stenosis. Int J Spine Surg 2018;12:342-51. [Crossref] [PubMed]
- Oertel MF, Ryang YM, Gilsbach JM, et al. Lumbar foraminal and far lateral juxtafacet cyst of intraspinal origin. Surg Neurol 2006;66:197-9; discussion 199. [Crossref] [PubMed]
- Sehati N, Khoo L, Holly L. Treatment of lumbar synovial cysts using minimally invasive surgical techniques Neurosurg Focus 2006;20:E2-6. [Crossref] [PubMed]
- Yasuma T, Arai K, Yamauchi Y. The histology of lumbar intervertebral disc herniation; the significance of small blood vessels in extruded tissue. Spine (Phila Pa 1976) 1993;18:1761-5. [Crossref] [PubMed]
- Wildi LM, Kurrer MO, Benini A, et al. Pseudocystic degeneration of the lumbar ligamentum flavum: a little known entity. J Spinal Disord Tech 2004;17:395-400. [Crossref] [PubMed]
- Shima Y, Rothman SL, Yasura K, et al. Degenerative intraspinal cyst of the cervical spine: case report and literature review. Spine (Phila Pa 1976) 2002;27:E18-22. [Crossref] [PubMed]
- Kao CC, Winkler SS, Turner JH. Synovial cyst of spinal facet. Case report. J Neurosurg 1974;41:372-6. [Crossref] [PubMed]
- Kjerulf TD, Terry DW, Boubelik RJ. Lumbar synovial or ganglion cysts. Neurosurgery 1986;19:415-20. [Crossref] [PubMed]
- Abdullah AF, Chambers RW, Daut DP. Lumbar nerve root compression by synovial cysts of the ligamentum flavum. Report of four cases. J Neurosurg 1984;60:617-20. [Crossref] [PubMed]
- Khan AM, Synnot K, Cammisa FP, et al. Lumbar synovial cysts of the spine: an evaluation of surgical outcome. J Spinal Disord Tech 2005;18:127-31. [Crossref] [PubMed]
- Christophis P, Asamoto S, Kuchelmeister K, et al. "Juxtafacet cysts", a misleading name for cystic formations of mobile spine (CYFMOS). Eur Spine J 2007;16:1499-505. [Crossref] [PubMed]
- Ikuta K, Tono O, Oga M. Prevalence and clinical features of intraspinal facet cysts after decompression surgery for lumbar spinal stenosis. J Neurosurg Spine 2009;10:617-22. [Crossref] [PubMed]
- Niggemann P, Kuchta J, Hoeffer J, et al. Juxtafacet cysts of the lumbar spine: a positional MRI study. Skeletal Radiol 2012;41:313-20. [Crossref] [PubMed]
- Phuong LK, Atkinson JLD, Thielen KR. Far lateral extraforaminal lumbar synovial cyst: report of two cases. Neurosurgery 2002;51:505-7; discussion 507-8. [Crossref] [PubMed]
- Salmon BL, Deprez MP, Stevenaert AE, et al. The extraforaminal juxtafacet cyst as a rare cause of L5 radiculopathy: a case report. Spine 2003;28:E405-7. [Crossref] [PubMed]
- Pendleton B, Carl B, Pollay M. Spinal extradural bengin synovial or ganglion cyst: case report. Neurosurgery 1983;13:322-6. [Crossref] [PubMed]
- Min WJ, Chang SH, Yang HY, et al. Endoscopically managed synovial cyst of the lumbar spine. Korean Spine J 2006;3:242-5.


